There is broad consensus that for the treatment of atrial fibrillation (AF) with catheter ablation, the goal of the procedure is pulmonary vein isolation (PVI)–that is, electrical isolation of the pulmonary veins (PV) from the rest of the left atrium by the creation of a ring of scar tissue. However, while acute PVI is typically achieved in most AF ablation procedures performed worldwide, the durability of this isolation is not necessarily assured. That is, the mechanism of acute PVI may not be tissue necrosis (as desired), but rather a combination of tissue necrosis and reversible tissue injury (such as tissue edema, hemorrhage, etc). This is an important issue since when this reversible tissue injury actually reverses (occurring in the order of a few weeks postprocedure), the resumption of electrical conduction provides the substrate for recurrent AF if/when that particular PV becomes electrically active. Over the past 5 to 10 years, there has been an important clinical understanding that durable PVI is much more elusive than previously appreciated. This is largely related to the technically demanding nature of the traditional approach of point-to-point radiofrequency ablation (RFA) to achieve PVI–that is, the difficulty of placing these points in a perfectly continuous/contiguous manner so as to avoid gaps in the ablation line. Indeed, because of these technical limitations, there has been, and continues to be, tremendous development in technological advances to facilitate the PVI procedure in creating transmural ablation lesions in a continuous ring. Furthest along of these technological advances are the balloon ablation catheters. The first such balloon catheter, the cryoballoon, has been approved by regulatory agencies in most countries, and has been used in general clinical use for 5 years or more. More recently, the visually-guided laser balloon (VGLB) catheter has been introduced; while it is still not approved for clinical use in many places in the world, it has been approved for use in Europe and is now being used clinically.
The VGLB catheter (called HeartLight; manufactured by CardioFocus Inc., Marlborough, Massachusetts, United States) is a novel technology designed to overcome the limitations of point-by-point ablation by permitting direct visualization of the target atrial tissue during ablation.1 To enable this, the catheter system incorporates a 2 F endoscope located at the proximal end of the balloon so as to visualize the face of the balloon as it is positioned apposed to the left atrial-PV junction. The balloon material allows for variable-sizing and deformation, such that there is only once balloon “size” to accommodate the highly-variable sizes and shapes characteristic of PVs. There is also an easily maneuverable 30° light arc to deliver ablative laser energy (980nm) to the target tissue. A combination of preclinical and clinical studies have demonstrated that the laser balloon is highly effective in creating transmural and durable lesions.1,2 However, beyond these initial clinical studies evaluating this technology, which by their very nature were performed in quite controlled settings, there are only early data on the use of this novel technology in broad clinical practice.3 It is in this context that the recent article by Osca et al4 published in Revista Española de Cardiología is interesting and relevant.
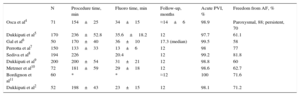
Osca et al report the ∼1 year results of using the VGLB catheter for the treatment of paroxysmal and persistent AF patients. The procedures were performed at a single center in Spain with otherwise unselected patients presenting for clinical care in a “real world” setting. A total of 71 patients were included in the acute isolation analysis. While the findings are comparable to other reports of high acute success with isolation of 99% of veins, it is nonetheless striking that this was achieved even though this was the initial experience with this catheter for the 2 operators performing the procedures. That is, the full learning curve with the use of this catheter was captured within this published experience itself. Of this cohort, 59 patients were included in the long-term follow-up, which included an average of ∼16±6 months. The clinical outcome of patients free from AF during follow-up was quite impressive: 88% and 70% success in the paroxysmal and persistent groups, respectively. While these data are fairly impressive relative to other previously published outcomes with VGLB ablation (Table), there are a number of caveats that need to be considered.
Comparison of Visually Guided Laser Balloon Trials
| N | Procedure time, min | Fluoro time, min | Follow-up, months | Acute PVI, % | Freedom from AF, % | |
|---|---|---|---|---|---|---|
| Osca et al4 | 71 | 154±25 | 34±15 | ≈14±6 | 98.9 | Paroxysmal, 88; persistent, 70 |
| Dukkipati et al5 | 170 | 236±52.8 | 35.6±18.2 | 12 | 97.7 | 61.1 |
| Gal et al6 | 50 | 170±40 | 36±10 | 17.3 (median) | 99.5 | 58 |
| Perrotta et al7 | 150 | 133±33 | 13±6 | 12 | 98 | 77 |
| Sediva et al8 | 194 | 226 | 20.4 | 12 | 99.2 | 81.8 |
| Dukkipati et al9 | 200 | 200±54 | 31±21 | 12 | 98.8 | 60 |
| Metzner et al10 | 72 | 181±59 | 29±18 | 12 | 98.6 | 62.7 |
| Bordignon et al11 | 60 | * | * | ≈12 | 100 | 71.6 |
| Dukkipati et al2 | 52 | 198±43 | 23±15 | 12 | 98.1 | 71.2 |
AF, atrial fibrillation; PVI, pulmonary vein isolation.
First, the population studied included predominantly men, with a mean age of 56 years and relatively few risk factors (mean CHA2DS2-VASC score=1.15). This type of relatively “healthy” population has important implications for the probability of ablation success. There are a number of clinical characteristics that predict improved success of AF ablation, including younger age and male sex. Furthermore, there are also imaging characteristics that predict improved ablation success. One of the most important predictors of success is smaller left atrial size; this is important since the mean left atrial size in this study cohort was only 26±8mm2. Thus, the population studied in this experience can be said to be relatively low risk–a point that indicates the feasibility of comparing these results to studies with other ablation technologies.
Second, the long-term follow-up success in this study was high in both patients with paroxysmal and persistent AF. However, the observed clinical success rate can be affected not only by the procedure quality, but also by the intensity of follow-up. In this study, follow-up occurred every 3 months with electrocardiograms and 24- to 48-hour Holter monitoring. However, a more robust follow-up would have increased our confidence that asymptomatic or nocturnal episodes of AF were not missed. For comparison, the Food and Drug Administration (FDA) HeartLight study was a prospective multicenter randomized trial comparing the VGLB catheter with standard RFA in 353 paroxysmal AF patients.5 For the primary efficacy endpoint of 1-year freedom from AF, the major finding was that laser balloon ablation was equivalent to RFA with respect to freedom from AF at 12 months (61.1% vs 61.7%; P=.003 for noninferiority). This FDA trial required follow-up with telephonic monitors starting at 3 months postprocedure and continuing to 12 months, in addition to Holter monitoring at 6 and 12 months. Indeed, the lower reported success rate in this FDA trial is consistent with this more intense follow-up protocol. Again, this does not necessarily mean that the 88% success rate observed by Osca et al is incorrect, but rather that it is inappropriate to make comparisons across clinical studies.
It was interesting that the present cohort also included patients with persistent AF. This strategy of balloon-based PVI for persistent AF, both with the cryoballoon and the VGLB catheters, has previously been described. Indeed, in one nonrandomized comparison of the laser balloon catheter with standard radiofrequency ablation, the freedom from AF at 1 year was similar in the VGLB and RFA groups (recurrence rates were 27.5% vs 22.5%, respectively, P=.87).12 However, there are important limitations of both that study and the present study: a) both studies enrolled AF patients with relatively short duration of persistent AF (in the study comparing VGLB with RFA, the median AF duration was only ∼2 months), and b) both studies enrolled a relatively small number of patients (only 17 patients had persistent AF in the present study). Thus, while the preliminary data are interesting, it is still too early to know exactly which persistent AF patients would benefit from VGLB ablation alone.
With regards to safety, in this study, the authors did not report several of the major complications that can occur with standard RFA: PV stenosis, stroke or atrioesophageal fistula. While the number of patients in this study is small, these data are certainly consistent with other published data indicating the safety of VGLB ablation.5,9 There were 2 instances of pericardial effusion, but these were not related to the VGLB catheter, but rather to the transeptal sheath. Also, as noted with other balloon-based ablation catheters, there were instances of phrenic nerve injury (n=4 patients, 5%). While 3 of 4 affected patients were reported recover phrenic nerve function, it is not clear how long after the procedure the recovery occurred. On the other hand, it is important that all events occurred in the center's first 18 procedures with the VGLB catheter. After this initial learning curve, the operators modified their technique to avoid further injury, including minimizing power when ablating near the course of the phrenic nerve anterior to the right superior PV.
Experience using the visually guided laser balloon has previously been reported to affect procedure and fluoroscopy times.9,12 This observation was demonstrated again in this study–there was a statistically significant difference in these measures with each successive tertile of 20 patients. This is similar to a previously published larger study of 150 patients in which tertiles of 50 patients noted incremental improvement in acute isolation of PV, procedure time, and fluoroscopy time.7 Furthermore, with greater experience, there were both: a) fewer observed complications, and b) improvements in clinical outcome related to increases in the amount of energy used for ablation.7,11
Thus, the present series adds to our knowledge of the safety and efficacy of the visually guided ablation laser balloon technology–particularly in the “real world” setting. It reinforces prior studies that have also demonstrated its efficacy in paroxysmal patients, along with early suggestions of efficacy in persistent AF. In addition, as with all new technologies, a learning curve was noted for both procedure/fluoroscopy times and complications. Future comparative studies will better inform its role relative to other balloon ablation catheters or RFA in both paroxysmal and persistent AF.
CONFLICTS OF INTERESTV.Y. Reddy acts as a consultant to and received grant support from CardioFocus, Inc.