Transcatheter aortic valve implantation (TAVI) has become the mainstay treatment for severe symptomatic aortic stenosis in patients older than 75 years. Because this technique is minimally invasive, it reduces both hospital stays and health care resource utilization. The growing number of procedures,1 however, has placed increasing pressure on coronary care units and cardiology wards. Procedural advances and a better understanding of associated complications have opened a new chapter in which same-day discharge can be safely considered in selected patients undergoing TAVI.2 The aim of this study was to describe our initial experience with a same-day post-TAVI discharge protocol for pacemaker carriers. Informed consent was obtained from all patients for publication of case details. The study was approved by the ethics committee of our hospital.
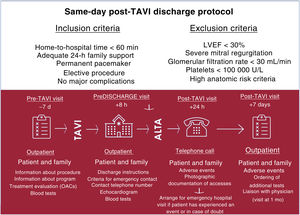
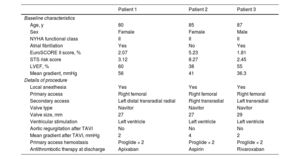
We analyzed a 2-month period in which 51 patients underwent TAVI. Three patients (5.8%) were eligible for discharge within the same-day post-TAVI discharge program of the hospital and were included in this study. The inclusion and exclusion criteria and follow-up steps specified in the protocol are shown in Figure 1. The baseline characteristics of the 3 patients discharged on the same day as TAVI are shown in table 1. All procedures were performed using a minimally invasive approach: local anesthesia without intubation, ultrasound-guided transfemoral access with vascular closure devices, transradial secondary access, or ventricular pacing using a guidewire. The patients were kept under observation for 8hours. Compression bandaging was removed from the vascular access site 4hours after the procedure and mobilization started 1 hour later. An echocardiogram and blood tests were performed before discharge. A follow-up telephone call was made 24hours after the procedure to check for major adverse events, defined as major vascular complications, major bleeding, acute myocardial infarction, stroke, or readmission with photographic documentation of vascular access sites. Possible complications were ruled out at an outpatient visit 7 days after the procedure. At this visit, all 3 patients were classified as being in functional class I according to the New York Heart Association (NYHA) classification. NYHA functional status remained unchanged at the 30-day visit, and none of the patients had experienced complications or adverse events requiring hospitalization.
Baseline characteristics of patients eligible for same-day discharge after TAVI and details of procedure
| Patient 1 | Patient 2 | Patient 3 | |
|---|---|---|---|
| Baseline characteristics | |||
| Age, y | 80 | 85 | 87 |
| Sex | Female | Female | Male |
| NYHA functional class | II | II | II |
| Atrial fibrillation | Yes | No | Yes |
| EuroSCORE II score, % | 2.07 | 5.23 | 1.81 |
| STS risk score | 3.12 | 8.27 | 2.45 |
| LVEF, % | 60 | 38 | 55 |
| Mean gradient, mmHg | 56 | 41 | 36.3 |
| Details of procedure | |||
| Local anesthesia | Yes | Yes | Yes |
| Primary access | Right femoral | Right femoral | Right femoral |
| Secondary access | Left distal transradial radial | Right transradial | Left transradial |
| Valve type | Navitor | Navitor | Navitor |
| Valve size, mm | 27 | 27 | 29 |
| Ventricular stimulation | Left ventricle | Left ventricle | Left ventricle |
| Aortic regurgitation after TAVI | No | No | No |
| Mean gradient after TAVI, mmHg | 2 | 4 | 2 |
| Primary access hemostasis | Proglide × 2 | Proglide × 2 | Proglide × 2 |
| Antithrombotic therapy at discharge | Apixaban | Aspirin | Rivaroxaban |
EuroSCORE II, European System for Cardiac Operative Risk Evaluation II; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; STS, Society of Thoracic Surgeons; TAVI, transcatheter aortic valve implantation.
The 20th anniversary of the first-ever TAVI procedure, performed by Dr Cribier and his team, was celebrated in 2022. Since its inception, the procedure has undergone numerous modifications in terms of patient selection, technique, valve technology, and postprocedural management. One of the last milestones to be achieved was same-day discharge, which has been shown to be safe in carefully selected patients.2 A fast-track TAVI discharge program implemented at our hospital during the COVID-19 pandemic proved to be both safe and effective.3 To our knowledge, the present study is the first to describe same-day discharge for TAVI in Spain. Involvement of a multidisciplinary team including an advanced practice nurse specialized in outpatient interventional cardiology procedures is essential for proper patient selection and education. One of the goals of this team is to assess and inform patients and their families about the procedure and the detection of possible complications. The main limitation of this study is its small sample size. The strict inclusion and exclusion criteria used in the same-day post-TAVI discharge protocol at our hospital limit the generalizability of our findings to less selected patient populations. In conclusion, same-day discharge after TAVI is feasible in carefully selected patients. Larger studies are needed to confirm the safety of the protocol, as well as strategies to evaluate the feasibility of same-day discharge in a broader set of patients, including those without a pacemaker.
FundingNone.
Authors’ ContributionsA. Regueiro conceived and designed the analysis. P. Cepas-Guillen, R. Gabani, T. Espinosa, M. Trilla, and P. Vidal-Calés performed the analysis. A. Regueiro, P. Cepas-Guillen, R. Gabani, T. Espinosa, M. Trilla, and P. Vidal-Calés reviewed and edited the manuscript.
Conflicts of InterestP.L. Cepas-Guillen and P. Vidal-Calés have received a research grant from Hospital Clínic de Barcelona (Contractes Clínic de Recerca Emili Letang-Josep Font). A. Regueiro is a proctor for Abbott Vascular. The other authors do not report any conflicts of interest.