Keywords
Heart failure affects 10% of individuals over the age of 70 and currently accounts for around 80 000 hospital admissions per year in Spain, a number that has progressively increased over the last decade. Heart failure is the third most common cause of mortality in our country and was responsible for 4% of deaths in men and 8% in women in 2000.1
Ischemic heart disease and hypertension (HT) are the main causes of this condition.2 Less common causes include primary or toxic cardiomyopathy, valvular or congenital lesions, right ventricular dysfunction caused by lung disease, and arrhythmia. Other important additional factors related to heart failure are diabetes,2 renal dysfunction, obesity, smoking, dyslipidemia, and atrial fibrillation (AF).2
Heart failure should be treated by joint collaboration in different health care settings, and should include the participation of hospital and community nursing professionals as well as physicians.4-6 Most heart failure patients are older individuals with several concomitant diseases, who are mainly attended by primary care physicians on an outpatient basis and by internal medicine specialists or cardiologists when they are admitted to hospital. Several studies published in recent years have brought to light various differences in the clinical and demographic profiles and the diagnostic and therapeutic management of heart failure patients depending on the specialty of the physician responsible for their care.4,5,7-9 The EPISERVE study was designed to analyze these aspects; in particular, to characterize the clinical profile of patients with heart failure and the degree of compliance with clinical practice guidelines in their diagnosis and treatment.
METHODS
Study Design and Patients Included
The EPISERVE study was designed as a multicenter, cross-sectional, uncontrolled, open, epidemiologic registry. The recruitment period spanned 5 months (June to November 2005). A total of 507 investigators participated, distributed over the entire territory of Spain, with the exception of the Rioja region, which did not participate. These physicians, who attended patients in primary care (n=181; 46%), cardiology (n=172; 34%), and internal medicine (n=154; 30%) outpatient clinics, voluntarily agreed to participate in the study after receiving an invitation by mail (response rate, 16%). Following a training session, each investigator recorded data from all the patients they saw until they had compiled, in strict order of arrival, the first 5 (different) patients over 18 years old and diagnosed with heart failure, as defined by the presence of at least 1 of the following criteria: a) prior hospitalization for heart failure; or b) diagnosis of heart failure established by the presence of 2 major criteria or 1 major criterion and 2 minor criteria according to the modified Framingham system.10 The only patients excluded were those who refused to participate (<1%). The study was approved by the Research Committee of Hospital Clínico de Santiago de Compostela. All patients signed a consent form to participate after being informed of the expected risks and benefits, and the methods of the study.
Data Collection and Diagnostic Criteria
Data were compiled in a computer database managed by professionals who were not involved in collecting the information. Heart failure was graded according to the standard NYHA classification.6 The main etiology was established based on the following criteria: ischemic disease when there was a documented history of myocardial infarction and presence of Q waves or evident left ventricular dyskinesia on echocardiography, hypertensive disease when there was a long-term history of high blood pressure and no other cause of heart failure, valve disease when there was echocardiographic evidence of significant valve involvement and no other cause of heart failure, cor pulmonale when there was a history of chronic lung disease and no other cause of heart failure, and idiopathic cardiomyopathy when that specific diagnosis was established on prior cardiologic study; all other etiologies were included under the heading Others.
The diagnosis of diabetes was based on the criteria of the American Diabetes Association.11 The diagnosis and grading of hypertension were established according to the guidelines of the Sociedad Española de Cardiología (Spanish Society of Cardiology).12 Cerebrovascular disease was defined as stroke or transient ischemic attack documented in the specialist's report, and peripheral vascular disease was established by intermittent claudication with an abnormal ankle-brachial index, presence of an abdominal or thoracic aneurysm, or a history of peripheral revascularization. Atrial fibrillation (AF) was considered to exist when there was electrocardiographic evidence of this condition, and includes the paroxysmal, persistent, and permanent types. Analytic variables corresponded to tests performed at the time of the study visit or within the previous 6 months. The diagnosis of anemia was based on the standard criteria of the World Health Organization13: hemoglobin <13 g/L in men and <12 g/L in women. Renal failure was established in patients showing glomerular filtration rates <60 mL/min/1.73 m2, estimated with the equation presented in the MDRD study.14 Data from electrocardiograms, chest x-rays, and echocardiograms acquired within the last year were included.
Clinical quality control was assessed attending to the guidelines of the European Society of Cardiology.15 The following criteria were considered to indicate inadequate clinical control: hyponatremia (<135 mEq/L), hypokalemia (<3.5 mEq/L), hyperkalemia (>5.2 mEq/L), and renal failure (creatinine >1.7 mg/dL). The following were considered inadequately controlled risk factors: blood pressure >130/80 mm Hg,16 body mass index >25, and smoking (any amount in the last year). Pharmacological treatment was classified as "adequate" if patients received drugs that are indicated, and not ones that are not indicated, in clinical practice guidelines6,15 according to their NYHA functional class, and "inadequate" in the remaining cases (therapies that are not indicated or failure to receive drugs that are indicated), as follows: beta-blockers in any functional class, providing that the patient did not have asthma or severe chronic obstructive pulmonary disease; angiotensin-converting-enzyme inhibitors in all functional classes; diuretic agents in classes III and IV, as well as class II when symptoms were present; spironolactone in functional class III and IV in the absence of renal dysfunction and hyperkalemia; digitalis agents in patients with AF and those in functional classes III and IV; and dicoumarin in the presence of AF.
Statistical Analysis
Variables with a continuous distribution (or quantitative variables) are summarized by measurement of the central tendency and spread of the data (mean, standard deviation, median, and 25th and 75th percentiles) and compared between groups with the non-parametric Mann-Whitney or Kruskal-Wallis tests. Variables with a discrete distribution (or qualitative variables) are shown by frequency tables and compared with the c2 or Fisher exact test, when appropriate. In all cases, 95% confidence intervals (CI) were applied and calculated over each percentage. A P value less than .05 was considered significant.
Univariate logistic regression was performed to detect factors related with adequacy of treatment. Adequate treatment was considered the dependent variable and comorbid conditions (diabetes, dyslipidemia, obesity, smoking, coronary revascularization, cognitive deterioration, renal failure, chronic obstructive pulmonary disease, and cerebral or peripheral vascular disease), cause of heart failure, demographic variables, and the health care setting were considered the explanatory variables. Variables showing statistical significance (P<.5) in the univariate analysis were included in a stepwise multivariate regression model.
RESULTS
Patients Included
The overall prevalence of heart failure was 4.7% (2% in primary care, 17% in cardiology, and 12% in internal medicine). Among a total of 2534 patients initially identified, 285 (11%) were excluded because they did not meet the criteria for heart failure (n=130) or were missing data for the study (n=155). Among the 2249 assessable patients, 778 were seen by a primary care physician, 777 by a cardiologist, and 694 by an internal medicine specialist. Mean age of the population was 72 (10) years and 55% were men (54%, 61%, and 51% of the primary care, cardiology, and internal medicine groups, respectively). The main clinical characteristics of the patients included are shown in Table 1. Hypertension and ischemic heart disease, alone or in combination, were the cause of more than 80% of cases. There were numerous associated conditions: HT in 76% of cases, atrial fibrillation in 46%, and diabetes in 38%. Other cardiovascular risk factors included obesity (64%), hypercholesterolemia (50%), smoking (30%), and hypertriglyceridemia (24%). The mean glomerular filtration rate was 72.1 (84.2) mL/min.
Diagnostic Procedures
The availability of diagnostic tests in the 3 outpatient settings is presented in Table 2. On chest radiography, available in 86% of patients, cardiomegaly was described in 88% of patients and pulmonary congestion in 51%. Electrocardiography was available in 87% of patients, with documentation of left bundle branch block in 18%, left ventricular hypertrophy in 59%, and permanent AF in 34%.
Electrocardiography
Electrocardiography had been carried out the previous year in 61% of all patients, with noticeably more tests in the group attended by cardiologists. The EF was <0.3 in 18%, 0.3 to 0.4 in 25%, 0.4 to 0.5 in 19%, and >0.5 in 38%. Left ventricular hypertrophy was documented in 60%, and the left atrial diameter was 51.7 (9.4) mm. Cardiac catheterization was performed in 31%, and was significantly more common in patients attended in cardiology.
There were no differences between men and women with regard to availability of electrocardiography and chest radiography. In contrast, more echocardiograms were carried out in men than women (63% vs 58%; P <.01), although differences were significant only in primary care (35% vs 28%). Cardiac catheterization was also performed in a higher percentage of men than women (35% vs 26%), with no statistical differences between the 3 health care settings.Treatment Applied
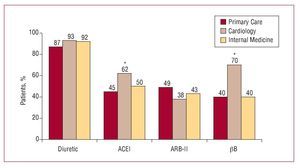
Almost all patients were under pharmacological treatment for heart failure: 98% were taking diuretics, 57% an angiotensin-converting-enzyme inhibitor (ACEI), 47% an angiotensin II receptor blocker (ARB) (combination of both agents in 7%), and 54%, a beta-blocker. The breakdown of these drugs according to the prescribing professional is shown in Figure 1. In addition, 56% were taking lipid-lowering drugs, 21% calcium channel blockers, and 35% digoxin, with no differences between the 3 groups of specialists.
Figure 1. Percentages of patients who took specific treatments for heart failure distributed according to the health care setting (n=2241). *P<.05 with respect to the other groups. ACEI indicates angiotensin-converting enzyme inhibitors; ARB, angiotensin II receptor blocker; bB, beta-blockers.
Significant differences were found between sexes related to the use of the various drug groups (men vs women): beta-blockers, 55% versus 44% (P<.001), diuretics, 88% versus 92% (P<.01), and lipid-lowering drugs, 57% versus 47% (P<.001). Differences in the use of beta-blockers and lipid-lowering drugs were significant between the 3 groups of professionals, whereas the use of diuretics was only significant in primary attention. Loop diuretics were the most common in this group. Enalapril was the most frequently prescribed ACEI (57%) at a mean dose of 17 mg/day, irbesartan was the most frequently used ARB (57%) at a mean dose of 242 mg/day, and carvedilol was the most commonly used beta-blocker (54%) at a dose of 25 mg/day. The specific agents from each drug family and the doses used to treat heart failure are summarized in Table 3.
Clinical Clinical Control According to the Guidelines
The percentages of patients with optimal control of the clinical factors are shown in Table 4. Only 20% of patients received adequate treatment according to the current European and Spanish guidelines, and treatment was significantly better in patients under the care of cardiologists. Inclusion in the category "inadequate treatment" was mainly due to the indication of diuretics in NYHA class I and failing to prescribe ACEI, beta-blockers, or spironolactone in NYHA class >III. The proportion of patients receiving anticoagulant treatment for AF was 79% in primary care, 86% in cardiology, and 86% in internal medicine, with no significant differences.
The clinical variables related to inadequate treatment in the univariate analysis were age, diabetes, dyslipidemia, smoking, ischemic heart disease, coronary revascularization, HT, and peripheral vascular disease, as well as the health care setting. In the multivariate analysis (Table 5), the only variables independently related to inadequate treatment were the health care setting (cardiology vs internal medicine or primary care), hypercholesterolemia, advanced age, and etiology of heart failure (neither ischemic nor hypertensive).
DISCUSSION
The results of the EPISERVE study indicate considerable disparity in the clinical and therapeutic characteristics of heart failure patients attended in the 3 usual health care settings for this disease in Spain. To our knowledge, this is the first study of this nature conducted in Spain. In addition to providing a complete overview of heart failure, the findings of EPISERVE underline the need to manage the disease as a cross-sectional health care process that includes all the professionals involved (physicians and nursing staff from various hospital and outpatient specialties, as well as social services), with the aim of offering more integrated and coordinated health care to patients with this condition.
Characteristics of Outpatients With Heart Failure
The EPISERVE study disclosed that 17% of outpatient cardiologic consultations are for heart failure. Perhaps for this reason there was a higher percentage of ischemic causes than hypertensive etiologies, when in most registries these 2 causes tend to be present in similar proportions.1,2,17,18 The mean age of our sample, 72 years, concurs with population registries, as does the 55% of men, a figure that gradually decreases as the age of the population analyzed increases. It is likely that ischemic etiology, which is more prevalent in the cardiology setting, led to a slight increase in the percentage of middle-aged men. The comorbid conditions that stand out include diabetes (13%), HT (76%), and AF (46%; permanent in 34%). The likely explanation is that the diagnosis of heart failure had been made more than 1 year earlier in 72% of patients. The high prevalence of comorbid conditions such as chronic obstructive pulmonary disease, cerebral vascular disease, anemia, and renal failure is notable, and these conditions were predictably more predominant in patients seen in the internal medicine setting.
Conventional cardiovascular risk was high in patients in the EPISERVE registry: 64% were obese, a value clearly higher than in the general population (around 24%). The distressing proportion of smokers (30%) is also noteworthy.
The BADAPIC8 registry in Spain and the EuroHeart Survey17 in Europe are among most far-reaching studies focusing on heart failure, and a comparison of their results with those of EPISERVE would be of interest. The main difference between the BADAPIC registry and EPISERVE is the health care setting (specialized heart failure clinics in the former and different settings in EPISERVE). This may be the reason why the mean age of the patients included was lower in BADAPIC, and there was a higher percentage of men. Ischemic etiology predominated in both studies, almost certainly because of the inevitable bias of this factor toward cardiology. Functional class was higher in the BADAPIC registry, whereas most of the patients in EPISERVE (54%) were in functional class II. The patients' risk profile is similar in BADAPIC, EPISERVE, and the EuroHeart Survey.
Diagnostic Procedures
It is logical that there would be a higher frequency of consultations in primary care centers: around 90% of patients were seen at intervals of <3 months in primary care, whereas most of the cardiology patients were seen about twice a year. The limited availability of electrocardiography in primary care was noteworthy, despite the fact that it is a recommended test in clinical practice guidelines.6,15 The small percentage of centers equipped with this test has been reported in other studies performed in outpatient populations.5,7 In contrast, electrocardiography was available to most patients seen in cardiology and two-thirds of those attended in the internal medicine setting.
The lower frequency of indications for electrocardiography in women is also in keeping with the findings of other studies. In our series, this difference was only significant in patients seen in primary care. Several factors may have influenced these results in addition to differences in sex: more advanced age and comorbid conditions, as well as the health care setting have been described. It has been proven that electrocardiographic testing during hospitalization for decompensated heart failure or chronic heart failure is an independent determinant of short- and long-term survival.19,20
The presence of 38% of patients with EF >0.5 stands out in this study. This value is higher than that reported in the BADAPIC registry (32% of patients with EF >0.45), but is consistent with heart failure studies in settings other than hospital departments and specialized heart failure units.5,7,9,17,18 As in the other registries, our study documented left ventricular hypertrophy in almost 60% of patients in whom echocardiography had been performed, probably because of the high prevalence of HT.21
Treatment Applied
Specific diets, particularly low-salt diets, were followed by more than 80% of the total series of patients. However, a high percentage of patients did not engage in any physical exercise. This seems to indicate that the health professionals caring for these individuals did not sufficiently emphasize the information about this vital factor.
Nearly all patients were taking some type of pharmacological treatment: more than 90% had diuretics; more than 80%, ACEI; and 50%, beta-blockers. The percentages of treated patients were comparable to values reported in other registries, such as the BADAPIC8 and EuroHeart Survey.17 Although the doses of heart failure-specific drugs used were lower than those recommended in the guidelines,8,15 they are comparable to doses reported in other registries.4,5,8,17
The percentage of patients treated with beta-blockers in cardiology was clearly higher than in the other 2 settings. This fact cannot be attributed to the higher percentage of patients with ischemic heart disease, since the clinical practice guidelines indicate the relevance of this treatment in heart failure patients in NYHA functional class II, regardless of the etiology.6,15
Another point of interest is the preference of primary care physicians and internal medicine specialists for ARB rather than ACEI, which are prescribed more often by cardiologists.6,15
Consistent with other studies,22 there were no significant differences in the treatments applied in relation to the type of systolic or diastolic dysfunction present. The absence of specific therapeutic recommendations in the latest clinical practice guidelines6,15 for patients with heart failure and preserved systolic function is, without a doubt, a determinant factor related to this finding. However, the fact that ACEI treatment showed no significant favorable effect in these patients in the CHARM23 and PEP-CHF24 studies indicates that this particular type of heart failure may have a different response to treatment than that of patients with heart failure and decreased systolic function. Some authors have even suggested that these may be 2 conditions with similar forms of clinical presentation, but a different pathogenesis.18
A smaller percentage of women received beta-blocker treatment than men in all 3 health care settings studied. This datum, which is consistent in all the registries,5,8,17,18 may be related to older age and a lower prevalence of ischemic heart disease in women.
In general, the percentage of patients receiving adequate treatment according to the recommendations of the Practice Guidelines of the European Society of Cardiology for the Diagnosis and Treatment of Chronic Heart Failure15 was higher among patients attended in cardiology than among those seen in the primary care or internal medicine setting (26% vs 18% and 17%, respectively); other studies have documented similar findings.25 In contrast, laboratory monitoring of sodium, potassium, hemoglobin, and creatinine was satisfactory in the 3 settings. In addition to smoking, the cardiovascular risk factor showing poorest control was HT. This is seen in all the studies investigating HT, whatever may be/regardless of the concomitant diseases and health care settings.5,7-9,12,16,17
Among other factors, the higher prevalence of ischemic heart disease as the main determinant of heart failure, lower age of the patients, and lower prevalence of associated diseases may help explain why cardiologists showed better compliance with the guidelines. Nonetheless, taking into account the changing clinical situation of heart failure, it does not suffice to prescribe specific therapeutic interventions with proven prognostic benefits. Close follow-up of affected patients is equally important to avoid decompensated disease, a goal that can only be achieved with integration and coordination among the various health care settings involved. Without a doubt, this issue points to one of the main shortcomings of cardiovascular medicine in Spain.Limitations of the Study
Because the patients included were seen in various settings (cardiology, internal medicine, and primary care), it was not possible to assess the clinical characteristics of the population of patients with heart failure in Spain; the study simply reflects the status of daily practice in these specific specialties. Moreover, it cannot be determined whether the type of sample chosen (consecutive rather than random sampling) has had a decisive influence on the results. The diagnosis of heart failure was not confirmed by objective tests in all cases (as occurs in most registries of this type); hence, patients with other conditions may have been included.
The data recorded in the registry were not submitted to a quality control system; therefore, we cannot exclude the possibility of selection bias if inclusion was not correlative, as the investigators were clearly told it should be. The fact that the participating investigators were volunteers may have introduced selection in the samples, although this would probably have little relevant impact. It does not seem likely that the small differences in the baseline characteristics of the population attended in the various settings would have an influence on the diagnostic and treatment approaches applied. Nonetheless, the greater comorbidity of patients seen by internal medicine and primary care physicians may have had an effect on the therapeutic strategy used.
Lastly, the small percentage of physicians who accepted the invitation to participate in the registry (16%) might have introduced some degree of selection bias in the patient population included and may have had some influence on the results.
CONCLUSIONS
Heart failure patients comprise a large volume of the total outpatient activity (17% in cardiology, 12% in internal medicine, and 2% in primary care). The recommendations set down in clinical practice guidelines are followed for only 20% of these patients. Cardiology specialists adhere more closely to these recommendations than do primary care and internal medicine specialists. The diagnostic and therapeutic procedures indicated in clinical practice guidelines are prescribed less often in women than men.
The EPISERVE study underlines the concept that outpatient heart failure care should be performed in a coordinated manner with the participation of other professionals through multidisciplinary care and continuing education.
ABBREVIATIONSAF: atrial fibrillation
EF: ejection fraction
HT: hypertension
NYHA: New York Heart Association
This study was funded by an unrestricted grant from Sanofi-Aventis. The company was not involved in the design, data analysis, or writing of the manuscript, or the decision to submit it to Revista Española de Cardiología. The database was created, maintained, and analyzed by Infociencia Clinical Research. Both companies deserve acknowledgement of their effective, professional assistance.
Correspondence:
Prof. J.R. González Juanatey.
Servicio de Cardiología. Hospital Clínico Universitario.Avda. Choupana, s/n. 15706 Vidan. Santiago de Compostela. A Coruña. Spain.
E-mail: jose.ramon.gonzalez.juanatey@sergas.es
Received March 7, 2007.
Accepted or publication March 3, 2008.