Health literacy (HL) has been associated with lower mortality in heart failure (HF). However, the results of previous studies may not be generalizable because the research was conducted in relatively young and highly-educated patients in United States settings. This study assessed the association of HL with disease knowledge, self-care, and all-cause mortality among very old patients, with a very low educational level.
MethodsThis prospective study was performed in 556 patients (mean age, 85 years), with high comorbidity, admitted for HF to the geriatric acute-care unit of 6 hospitals in Spain. About 74% of patients had less than primary education and 71% had preserved systolic function. Health literacy was assessed with the Short Assessment of Health Literacy for Spanish-speaking Adults questionnaire, knowledge of HF with the DeWalt questionnaire, and HF self-care with the European Heart Failure Self-Care Behaviour Scale.
ResultsDisease knowledge progressively increased with HL; compared with being in the lowest (worse) tertile of HL, the multivariable beta coefficient (95%CI) of the HF knowledge score was 0.60 (0.01-1.19) in the second tertile and 0.87 (0.24-1.50) in the highest tertile, P-trend = .008. However, no association was found between HL and HF self-care. During the 12 months of follow-up, there were 189 deaths. Compared with being in the lowest tertile of HL, the multivariable HR (95%CI) of mortality was 0.84 (0.56-1.27) in the second tertile and 0.99 (0.65-1.51) in the highest tertile, P-trend = .969.
ConclusionsNo association was found between HL and 12-month mortality. This could be partly due to the lack of a link between HL and self-care.
Keywords
Health literacy (HL) is the degree to which individuals can obtain, process, and understand basic health information and services needed to make appropriate health decisions.1 Adequate HL is important to ensure proper patient-clinician interaction, full understanding of health counseling and treatment prescription, and competent self-care.2 Therefore, HL is of particular importance for those patients with complex health problems requiring long-term self-management. A good example of this type of problems is heart failure (HF), because appropriate self-care entails integration of knowledge and skills to monitor symptoms and weight, take adequate physical exercise, follow a healthy diet with low salt intake, titrate diuretics, and recognize early manifestations of worsening HF, among other measures3,4; in fact, clinical guidelines for the management of HF recommend a structured care plan that promotes self-care for every patient.5,6
Among patients with HF, there is evidence that HL is associated with better disease knowledge, but information on the impact of HL on self-care is inconclusive because studies have reported conflicting results.7,8 Moreover, we are aware of only 2 studies that have investigated the relationship between HL and all-cause mortality. The first, conducted in ambulatory patients with chronic HF in an integrated managed care organization in the US, found that low HL was associated with higher mortality over a 1.2-year follow-up.9 The second study, performed in patients hospitalized for HF in a quaternary care center in the US, reported that lower HL was linked to an increased risk of death during a 21-month follow-up.10
However, these results may not be generalizable because the effect of low HL could vary with the characteristics of the patient population and the health care system.9 These 2 studies included patients with a mean age of 75 and 63 years, respectively9,10; thus, compared with HF patients currently attended in many clinical practices, patients in these 2 studies were younger and probably had less morbidity and a lower percentage of preserved left ventricular ejection fraction, which lacks an effective HF-specific drug treatment.11 Moreover, most of the study participants had completed at least high school. Lastly, both studies were conducted in the United States, and given that HL is a complex characteristic that influences the ability to navigate the health care system,1,2 their results may not apply to National Health Service-like systems characterized by public funding and free access to specialized services regardless of socioeconomic status.
Accordingly, this work aimed to assess the prospective association of HL with disease knowledge, self-care, and all-cause mortality among very old patients admitted for HF in 6 hospitals in Spain, a country with a state-funded and free-access health care system.
METHODSStudy Design and ParticipantsWe conducted a prospective cohort study of participants in the HF-geriatrics randomized controlled trial, which assessed the effectiveness of a disease management program among very old patients with HF and major comorbidity (ClinicalTrials.gov number, NCT01076465). The study methods and main results have been published elsewhere.12,13 Briefly, we recruited patients aged ≥ 75 years admitted with a primary diagnosis of HF to the geriatric acute-care unit of 6 hospitals in Spain. Diagnosis of HF was performed according to the European Society of Cardiology and Framingham criteria.14 To be included, each patient had to meet at least 1 of the following comorbidity criteria: Charlson index ≥ 3, dependence in ≥ 2 activities of daily living, treatment with ≥ 5 drugs, active treatment for ≥ 3 diseases, recent emergency hospitalization (in the last 3 months), severe visual or hearing loss, cognitive impairment, depressive syndrome, Parkinson's disease, diabetes mellitus, chronic obstructive pulmonary disease, anemia, or constitutional syndrome.
Exclusion criteria were end-stage or rapidly fatal disease and estimated life expectancy < 6 weeks, severe functional or cognitive impairment preventing patients from understanding their illness and lack of a caregiver agreeing to participate in the study, being on the waiting-list for cardiac surgery, difficulty in being followed up (eg, due to change of address), and being institutionalized without a known primary caregiver. Patient recruitment took place from December 1, 2010 to November 30, 2012. Among 796 eligible patients, 630 (79.2%) accepted to participate. Unfortunately, no data were collected on the reasons for nonparticipation.
Study participants were randomly assigned to a disease management program led by a case manager or to usual care and were followed up for 12 months to assess clinical outcomes. Information on HL, disease knowledge and management was reported by the patient or caregiver depending on the clinical status and patients’ preference. The study sample was calculated to ensure sufficient statistical power to assess the effectiveness of a disease management program.12
All patients and/or 1 family member provided informed consent. The study protocol was approved by the clinical research ethics committees of the participating hospitals.
Health LiteracyAt baseline, HL was assessed with the Short Assessment of Health Literacy for Spanish-speaking Adults (SAHLSA) questionnaire.15 This is an interviewer-administered instrument developed from the Rapid Estimates of Adult Literacy in Medicine, which is one of the most widely used tools for assessing HL in English.16 The SAHLSA includes 50 items that explore recognition and comprehension of common medical terms, using multiple-choice questions designed by an expert panel. The SAHLSA-50 score is associated with the physical health status of Spanish-speaking participants and has shown good internal reliability and test-retest reliability. The SAHLSA score ranges from 0 to 50 and a higher score indicates higher HL.15
Study OutcomesKnowledge of HF and self-care were measured at baseline and at 6 months of follow-up. Knowledge of HF was ascertained with the instrument developed by DeWalt et al.,17 which includes 15 questions about the concept and symptoms of HF and dehydration, as well as manifestations of worsening HF. The score ranges from 0 to 15, and a higher score represents better knowledge.
Self-care was assessed with the European Heart Failure Self-Care Behaviour Scale, which includes 12 items on weight monitoring, attitude to worsening HF signs and symptoms, limiting fluid and salt intake, physical exercise, vaccination, and adherence to drug treatment.18 This scale ranges from 1 to 60, and lower scores indicate better care.
All-cause death was identified during the follow-up by reviewing clinical charts and by contact with relatives and primary caregivers. Identification of all-cause death was complete.
Other VariablesData were also collected on other variables that could be associated with both HL and the study outcomes. Specifically, we used age (years), sex, treatment (disease management program) group, hospital, functional status as summarized by the New York Heart Association grade (I-II vs III-IV), left ventricular ejection fraction (≥ 45 vs < 45%), atrial fibrillation, hemoglobin (mg/dL), and serum creatinine (mg/dL). We also assessed depression with the 15-item Geriatric Depression Scale,19 comorbidity with the Charlson index, and cognitive impairment with the Mini-mental State Examination (< 22 vs ≥ 22).20 Lastly we registered limitations in activities of daily living with the Katz index,21 hospitalization for HF in the preceding year, and level of education (unable to read or no formal education, less than primary education, and primary education or higher).
Statistical AnalysisAmong the 630 study participants, 74 were excluded because of missing data in 1 or more study variables. Thus, analyses were conducted with 556 individuals. They were classified into tertiles of HL (SAHLSA-50 scores), and differences in baseline sociodemographic and clinical characteristics between tertiles were assessed with chi-square and ANOVA (analysis of variance) tests, as appropriate.
We used linear regression models to estimate the association of baseline HL with HF knowledge or self-care at 6 months; the results are presented as beta coefficients of HF knowledge or self-care, and their corresponding 95% confidence intervals (95%CI). The lowest tertile of HL was used as the reference group in the analyses. To test the dose-response relationship, we estimated a P-value for trend by modeling tertiles of HL as a continuous variable. We built 3 hierarchical models: the first was adjusted for age, sex, treatment group, hospital, and baseline values of HF knowledge or HF self-care scores, as appropriate; the second model further adjusted for the New York Heart Association grade, left ventricular ejection fraction, atrial fibrillation, hemoglobin, creatinine, depression, Charlson index, cognitive impairment, Katz index, and hospitalization for HF in the last year; and the third model was additionally adjusted for educational level, because HL and education are associated but a certain level of education may not ensure adequate HL.
Survival during the 12-month follow-up according to tertiles of HL was estimated with the Kaplan-Meier methods, and between-group differences were tested with the log rank test. Cox regression was used to assess the association between baseline HL and all-cause mortality, and the results were summarized with hazard ratios (HR) of mortality and their 95%CI across tertiles of HL. We also built the 3 hierarchical models described above. In addition, we built a fourth model that further adjusted for HF knowledge, and a fifth model that also adjusted for HF self-care. These last 2 models aimed to assess whether the potential association between HL and morbidity could be mediated by HF knowledge or HF self-care. In statistical analyses, potential confounders were selected because they are known risk factors for mortality in HF patients and because in the study sample their HR of mortality were usually in the expected direction (Table 1 of the supplementary material).
To assess the robustness of the results, we conducted a number of sensitivity analyses; specifically, we replicated the analyses in strata defined by age (< 85 vs ≥ 85 years), New York Heart Association grade (I-II vs III-IV), the median Charlson index score (< 3 vs ≥ 3), left ventricular ejection fraction (< 45% vs ≥ 45%), depression (yes vs no), Mini-mental State Examination (< 22 vs ≥ 22), HF hospitalization in the last year (yes vs no), and educational level (unable to read or no formal education, less than primary education, and primary education or higher). We tested if the study results varied between strata by using likely ratio tests that compared models with and without interaction terms (products of HL tertiles by stratum categories).
The proportional hazards assumption was tested both graphically and with interaction terms for HL and time of follow-up. No evidence was found of departure from this assumption (P > .05). All tests were 2-sided and statistical significance was set at P < .05. Analyses were performed with STATA 13.0.
RESULTSAmong study participants, the mean ± standard deviation age was 85.6 ± 5.1 years, 62.2% were women, 70.5% had preserved systolic function, and 43.8% had been hospitalized for HF in the last year. A total of 73.7% has less than primary education. The frequency of morbidity was high, because ischemic heart disease was present in 16.8%, chronic obstructive lung disease in 31.3%, diabetes in 33.9%, hypertension in 81.8%, and depression in 34%, the Mini-mental State Examination score was < 22 in 36.2% and 17.1% had had a stroke. The mean ± standard deviation Charlson index was 3.4 ± 1.9.
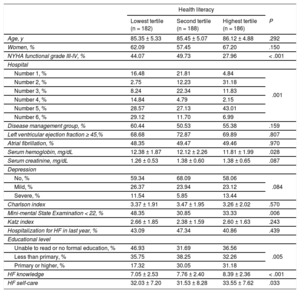
Compared with patients in the lowest (worse) tertile of HL, those in the higher tertiles less frequently had III-IV grade of the New York Heart Association and cognitive impairment, and had lower hemoglobin level (Table 1). Moreover, these patients had a higher educational level. The distribution of HL varied substantially across hospitals (Table 1).
Characteristics of Study Participants Across Tertiles of Health Literacy
| Health literacy | ||||
|---|---|---|---|---|
| Lowest tertile (n = 182) | Second tertile (n = 188) | Highest tertile (n = 186) | P | |
| Age, y | 85.35 ± 5.33 | 85.45 ± 5.07 | 86.12 ± 4.88 | .292 |
| Women, % | 62.09 | 57.45 | 67.20 | .150 |
| NYHA functional grade III-IV, % | 44.07 | 49.73 | 27.96 | < .001 |
| Hospital | ||||
| Number 1, % | 16.48 | 21.81 | 4.84 | .001 |
| Number 2, % | 2.75 | 12.23 | 31.18 | |
| Number 3, % | 8.24 | 22.34 | 11.83 | |
| Number 4, % | 14.84 | 4.79 | 2.15 | |
| Number 5, % | 28.57 | 27.13 | 43.01 | |
| Number 6, % | 29.12 | 11.70 | 6.99 | |
| Disease management group, % | 60.44 | 50.53 | 55.38 | .159 |
| Left ventricular ejection fraction ≥ 45,% | 68.68 | 72.87 | 69.89 | .807 |
| Atrial fibrillation, % | 48.35 | 49.47 | 49.46 | .970 |
| Serum hemoglobin, mg/dL | 12.38 ± 1.87 | 12.12 ± 2.26 | 11.81 ± 1.99 | .028 |
| Serum creatinine, mg/dL | 1.26 ± 0.53 | 1.38 ± 0.60 | 1.38 ± 0.65 | .087 |
| Depression | ||||
| No, % | 59.34 | 68.09 | 58.06 | .084 |
| Mild, % | 26.37 | 23.94 | 23.12 | |
| Severe, % | 11.54 | 5.85 | 13.44 | |
| Charlson index | 3.37 ± 1.91 | 3.47 ± 1.95 | 3.26 ± 2.02 | .570 |
| Mini-mental State Examination < 22, % | 48.35 | 30.85 | 33.33 | .006 |
| Katz index | 2.66 ± 1.85 | 2.38 ± 1.59 | 2.60 ± 1.63 | .243 |
| Hospitalization for HF in last year, % | 43.09 | 47.34 | 40.86 | .439 |
| Educational level | ||||
| Unable to read or no formal education, % | 46.93 | 31.69 | 36.56 | .005 |
| Less than primary, % | 35.75 | 38.25 | 32.26 | |
| Primary or higher, % | 17.32 | 30.05 | 31.18 | |
| HF knowledge | 7.05 ± 2.53 | 7.76 ± 2.40 | 8.39 ± 2.36 | < .001 |
| HF self-care | 32.03 ± 7.20 | 31.53 ± 8.28 | 33.55 ± 7.62 | .033 |
HF, heart failure; NYHA, New York Heart Association.
Unless otherwise indicated, values are expressed as mean ± standard deviation.
Range of values for tertiles of health literacy: 0 to 34 for the lowest tertile, 35 to 41 for the second tertile, and 42 to 50 for the highest tertile.
Heart failure knowledge, as per the DeWalt et al.17 Heart failure self-care as per the European Heart Failure Self-Care Behaviour Scale.
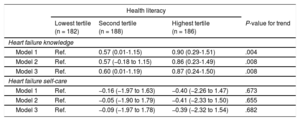
Table 2 shows the association between HL at baseline and HF knowledge or HF self-care at 6 months of follow-up, with adjustment for baselines values of these 2 variables. Given that the results of analyses adjusted for sociodemographic variables, treatment group, hospital, and baseline values of the dependent variables (model 1) and those with full adjustment for potential confounders (model 3) were similar, we emphasize the fully-adjusted results throughout the manuscript. Disease knowledge increased progressively with higher HL; compared with patients in the lowest (worse) tertile of HL, the beta coefficient (95%CI) of the HF knowledge score was 0.60 (0.01-1.19) in the second tertile and 0.87 (0.24-1.50) in the highest tertile, P-trend = .008. However, no association was found between HL and HF self-care score; the corresponding results were −0.09 (−1.97 to 1.78) in the second tertile and −0.39 (−2.32 to 1.54) in the highest tertile of HL, P-trend = .682.
Beta Coefficients (95% Confidence Interval) of Heart Failure Knowledge and Self-care Scores at 6 Months Post-discharge According to Tertiles of Baseline Health Literacy
| Health literacy | ||||
|---|---|---|---|---|
| Lowest tertile (n = 182) | Second tertile (n = 188) | Highest tertile (n = 186) | P-value for trend | |
| Heart failure knowledge | ||||
| Model 1 | Ref. | 0.57 (0.01-1.15) | 0.90 (0.29-1.51) | .004 |
| Model 2 | Ref. | 0.57 (−0.18 to 1.15) | 0.86 (0.23-1.49) | .008 |
| Model 3 | Ref. | 0.60 (0.01-1.19) | 0.87 (0.24-1.50) | .008 |
| Heart failure self-care | ||||
| Model 1 | Ref. | −0.16 (−1.97 to 1.63) | −0.40 (−2.26 to 1.47) | .673 |
| Model 2 | Ref. | −0.05 (−1.90 to 1.79) | −0.41 (−2.33 to 1.50) | .655 |
| Model 3 | Ref. | −0.09 (−1.97 to 1.78) | −0.39 (−2.32 to 1.54) | .682 |
Model 1 was adjusted for age (< 85, ≥ 85 years), sex (male, female), treatment group (intervention, no intervention), hospital (1, 2, 3, 4, 5, 6), and baseline value of knowledge score or self-care score, as appropriate.
Model 2 was adjusted as model 1 and additionally for New York Heart Association grade (I-II, III-IV), left ventricular ejection fraction (< 45, ≥ 45%), atrial fibrillation (yes, no), serum hemoglobin (mg/dL), serum creatinine (mg/dL), depression (no, mild, severe), Charlson index (continuous), Katz index (continuous), Mini-mental State Examination (< 22, ≥ 22), hospitalization for heart failure in last year (yes, no).
Model 3 was adjusted as model 2 and additionally for education (unable to read or no formal studies, less than primary, primary or higher studies).
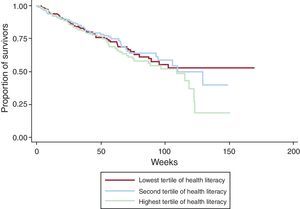
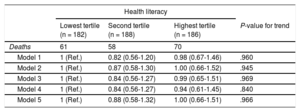
During the 12 months of follow-up, there were 189 deaths. At baseline, HL did not show an association with all-cause mortality (Figure). Compared with patients in the lowest tertile of HL, the HR (95%CI) of mortality was 0.84 (0.56-1.27) in the second tertile, and 0.99 (0.65-1.51) in the highest tertile, P-trend = .969. The results also held after adjustment for baseline scores of HF knowledge and HF self-care (Table 3). Table 2 of the supplementary material shows that the main results (model 3) did not vary across strata of patients defined by clinical variables.
Hazard Ratios (95% Confidence Interval) of 12-month All-cause Mortality, According to Tertiles of Baseline Health Literacy
| Health literacy | ||||
|---|---|---|---|---|
| Lowest tertile (n = 182) | Second tertile (n = 188) | Highest tertile (n = 186) | P-value for trend | |
| Deaths | 61 | 58 | 70 | |
| Model 1 | 1 (Ref.) | 0.82 (0.56-1.20) | 0.98 (0.67-1.46) | .960 |
| Model 2 | 1 (Ref.) | 0.87 (0.58-1.30) | 1.00 (0.66-1.52) | .945 |
| Model 3 | 1 (Ref.) | 0.84 (0.56-1.27) | 0.99 (0.65-1.51) | .969 |
| Model 4 | 1 (Ref.) | 0.84 (0.56-1.27) | 0.94 (0.61-1.45) | .840 |
| Model 5 | 1 (Ref.) | 0.88 (0.58-1.32) | 1.00 (0.66-1.51) | .966 |
Model 1 was adjusted for age (< 85, ≥ 85 years), sex (male, female), treatment group (intervention, no intervention) and hospital (1, 2, 3, 4, 5, 6).
Model 2 was adjusted as model 1 and additionally for New York Heart Association grade (I-II, III-IV), left ventricular ejection fraction (< 45, ≥ 45%), atrial fibrillation (yes, no), serum hemoglobin (mg/dL), serum creatinine (mg/dL), depression (no, mild, severe), Charlson index (continuous), Katz index (continuous), Mini-Mental State Examination (< 22, ≥ 22), hospitalization for heart failure in last year (yes, no),
Model 3 was adjusted as model 2 and additionally for education (unable to read or no formal education, less than primary, primary education or higher).
Model 4 was adjusted as model 3 and additionally for heart failure knowledge score.
Model 5 was adjusted as model 4 and additionally for heart failure self-care score.
In this prospective study of very old patients with high comorbidity admitted for HF to 6 Spanish hospitals, a higher HL was associated with greater HF knowledge at 6 months post-discharge; however, no association was found between HL and HF self-care at 6 months post-discharge or all-cause mortality during a 12-month follow-up.
Our results are in line with those of previous studies on the association between HL and disease knowledge in patients with HF. Specifically, we are aware of 5 studies reporting that high HL is linked to better HF knowledge.22–26 All these studies assessed HL with the Short Test of Functional Health Literacy in Adults, a widely used test to identify patients who have poor HL and require more intensive educational, counseling, and caregiver interventions.27 Our study extends knowledge in this field because it is the only work with a prospective design, because the mean age of the study participants was about 20 years older than that in previous research,22–26 and because HL was ascertained with the SAHLSA-50.
Previous research on HL and self-care in patients with HF has yielded inconclusive results. While several studies have reported that high HL is associated with better self-care,22,28,29 others have found no significant association,23,25,26 and 1 study has even reported an inverse association.30 Of note is that in baseline cross-sectional analyses (Table 1), we also observed a slightly inverse association between HL and self-care behaviors. However, in longitudinal analyses with adjustment for many confounders including baseline self-care score, we found no association between HL and self-care. Our results are difficult to compare with those in the literature, because published studies had a cross-sectional design, included much younger patients, and measured HL and, sometimes, self-care with questionnaires different to ours.
In contrast with 2 recent studies,9,10 we did not find an association between HL and all-cause mortality. There could be several explanations for these null results. First, although worse self-care in previous studies did not entirely mediate the association between lower HL and worse clinical outcomes,28 the lack of association between HL and self-care in our study makes it difficult to observe an association between HL and mortality. Second, study participants were very old, suffered from a relatively advanced-stage HF (eg, had at least 1 hospitalization for HF), and had high comorbidity; as a result, these patients had a poor prognosis, and required complex clinical management. Therefore, the potentially beneficial effect of HL would have had to be very large to produce an observable reduction in mortality. Third, 71% of patients had preserved systolic function. Given that there are no proven effective drug treatments for diastolic HF, it is uncertain whether better HF self-care associated with higher HL could lead to lower mortality. Fourth, the free-access health care system in Spain, with frequent consultations with primary care professionals and specialists as well as continuous follow-up by nurses, may have compensated for low HL. In fact, in our study, the HR (95%CI) of mortality for those with no formal education vs those with primary education or higher was 1.05 (0.69-1.61). This suggests that our health care system may contribute to reduce socioeconomic health inequalities, including those related to HL. Future research should confirm our results and systematically identify the mechanisms for the association (or lack of association) between HL and mortality in very old patients hospitalized for HF.
Strengths and LimitationsOur work has several strengths. In contrast with the 2 previous studies on HL and mortality, which were based on retrospective cohorts,9,10 our study had a prospective design. This allowed registration of intermediate variables at the 6-month follow-up (eg, HF knowledge and HF self-care), which enhanced understanding the null association between HL and mortality. In addition, the very old age and the exhaustive follow-up of study participants served to identify a considerable number of deaths and to ensure sufficient statistical precision in the study results. Moreover, the analyses were adjusted for a fair number of potential confounders, including education, left ventricular ejection fraction, comorbidity, and correlates of severity (eg, HF hospitalization in the preceding year, and disability); in addition, the semicrude (model 1) and fully-adjusted (model 3) results were very similar, suggesting that residual confounding, if any, was small.
This study also has some limitations. First, HL is a broad concept and the SHALSA-50 may not capture all its dimensions, in particular, functional components of HL that are most useful for clinical decision-making; this may have contributed to a lack of association between HL and mortality. Second, the analyses were not adjusted for cardiovascular treatments and medication adherence; however, it could be argued that these are mediators of a potential association between HL and mortality and, thus, they should not be adjusted for. Nevertheless, the analyses were adjusted for many clinical characteristics that are correlated with drug treatment and adherence, so that further adjustment for the latter variables would probably not modify the main results. Last, unlike previous studies,9,10 we did not collect data on hospitalizations during follow-up, which could serve to improve understanding of the null association between HL and mortality. However, data on hospitalizations are difficult to interpret; first, because hospitalization depends on the severity of HF decompensation and also on the organization and rules of the health care system in each region and country and, second, because HL has shown an inconsistent association with hospitalization and with mortality in previous studies. For example, Peterson et al.9 reported that low HL was associated with higher all-cause mortality but not hospitalization, and McNaughton et al.10 observed that lower HL was associated with an increased risk of death but found no evident relationship between HL and 90-day rehospitalization or emergency department visits.
CONCLUSIONSIn this prospective study of very old patients with substantial comorbidity who were hospitalized for HF within a free-access high-quality health care system in Spain, we found no association between HL and 12-month all-cause mortality. These null results could be partly due to a lack of association between higher HL and better HF self-care at 6 months post-discharge. Future studies should confirm these results with instruments assessing all dimensions of HL. In addition, they should collect data on knowledge and self-care for diseases that frequently coexist with HF in very old patients, such as atrial fibrillation, diabetes, chronic lung disease, or depression. Finally, given that a substantial percentage of deaths in these patients are due to causes other than cardiovascular disease, the use of cause-specific mortality data will lead to a better understanding of the association between HL and death.
FUNDINGThis work was funded by grants PI09/91064, PI11/640, PI12/1166 and PI14/01044 from the Instituto de Salud Carlos III (Secretary of R+D+I and European Regional Development Fund/European Social Fund).
CONFLICTS OF INTERESTNone declared.
- –
Among patients with HF, HL is associated with better disease knowledge but the impact of HL on self-care is uncertain.
- –
Health literacy has been associated with lower mortality in HF, but the results of previous studies may not be generalizable because the research was conducted with relatively young and highly-educated patients in United States settings.
- –
Among very old patients, with low educational level, admitted for HF in 6 hospitals in Spain, no association was found between HL and 12-month mortality. This could be partly due to a lack of association between higher HL and better self-care in this type of patient.
- –
The role of HL on health outcomes may vary across types of patients and health care systems. The access-free health care system of Spain, with frequent consultations with primary care professionals and specialists as well as continuous follow-up by nurses, may have compensated for low HL.