A 72-year-old woman was referred for exertional dyspnea, cough, and peripheral edema. The patient had undergone mitral-tricuspid reparative surgery (annuloplasty and quadrangular posterior leaflet resection and De Vega annuloplasty, respectively) 22 years prior.
An echocardiogram at that time revealed degenerative mitral regurgitation and normal left atrium (LA).
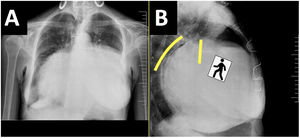
Chest radiography showed a massive enlargement of the cardiac silhouette and tracheal displacement on anteroposterior view; lateral view revealed a typical “walking man” sign due to posterior displacement of the left main bronchus (figure 1A,B, lines).
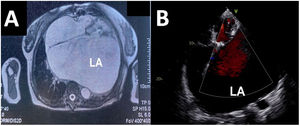
Magnetic resonance imaging showed a 218-cm3 LA displacing the other cardiac chambers (figure 2A). The right atrium was 54cm.3
A transthoracic echocardiogram revealed good biventricular function, no dilation, 14 × 14cm LA, moderate-to-severe mitral regurgitation with mild stenosis, severe tricuspid regurgitation, and systolic pulmonary pressure of 39mmHg (figure 2B).
The patient underwent mitral valve replacement, tricuspid annuloplasty and septal leaflet tear closure, LA reduction by wall plication, and left appendage closure (figure 3A). Length of hospital stay was 15 days. Echocardiography and radiography at discharge showed substantial LA reduction (figure 3B,C) but tissue fragility did not allow more extensive reduction.
Giant LA is rare (0.3%). This entity usually occurs in long-standing rheumatic mitral disease and is anecdotal in degenerative regurgitation. The definition varies and includes anomalies of the atrial wall and chronic volume/pressure overload.
Our case is unique because giant LA developed years after mitral repair for degenerative regurgitation and with relatively moderate valvular disease.
The patient provided written informed consent, which is available for review.
FUNDINGThe authors state they received no funding.
AUTHORS’ CONTRIBUTIONSA. Affronti: idea, drafting, editing. E. Quintana: supervision. M. Castellà: supervision.
CONFLICTS OF INTERESTThe authors have no conflicts of interest to disclose.
The authors would like to thank Dr. María Ascaso for her contribution in providing intraoperative images of this case.