Percutaneous revascularization of chronic total coronary artery occlusion is a technical challenge and has a lower success rate than other angioplasty procedures. Identification of predictors of failure could lead to better selection of patients with the greatest possibility of success. In this study, we investigate the multidetector computed tomography features associated with failure of percutaneous treatment for chronic total coronary occlusion.
MethodsThis is a prospective, single-center study of 69 consecutive patients with chronic total occlusion in whom multidetector computed tomography study was performed before percutaneous coronary revascularization.
ResultsSeventy-seven lesions were analyzed. The mean length of the occlusion was 19.9 (14.3) mm and the estimated duration of occlusion was 47 (62) months. The only angiographic factor independently predictive of failure was a severe curve between the plaque and the proximal patent vessel (odds ratio 3.8, 95% confidence interval, 1.2-12; P=.02). On multidetector computed tomography, the only factor predictive of failure was an arc of calcium affecting more than 50% of the vessel circumference in the proximal (P=.04) and middle (P=.03) third of the occlusion.
ConclusionsMultidetector computed tomography identified a variable that cannot be measured by angiography that can predict failure in percutaneous revascularization of chronic total coronary occlusions. In selected cases, this parameter could be useful for preprocedure screening.
Keywords
.
IntroductionChronic total coronary occlusion (CTO) is defined as a complete interruption of coronary artery flow lasting more than 3 months. The duration of the occlusion is established by evidence on a previous coronary angiography study, a history of myocardial infarction in territory corresponding to the occluded vessel, or a change in the anginal pattern. In all other cases, the duration is considered uncertain.1
The objective of CTO recanalization is mitigation of angina and improvement of left ventricular function, with recovery of hypocontractile ischemic areas.2, 3 The prevalence of CTO in the general population is unknown, although it is found in 31% of patients with coronary disease referred for angiography.4, 5
Although CTO is a common condition, percutaneous revascularization is attempted in less than 10% of cases.1, 6 Despite the fact that complex cases can be treated,7 only 2.9% of angioplasties performed in Spain in 2008 were for CTO.8
The technique used is complex, and despite the increasing experience of operators and the development of new devices the success rate is low.9 This fact, together with the cost of the procedure,2, 10 high rates of restenosis and contrast nephropathy,11 and associated radiation exposure,12 may explain the limited use of this treatment.4
Multidetector computed tomography (MDCT) coronary angiography has emerged as a noninvasive technique that can evaluate the structure and composition of an occluded vessel.13, 14, 15
The aim of this study is to determine whether MDCT, together with an analysis of angiographic variables, enables identification of the morphologic characteristics of CTO associated with failure of percutaneous recanalization.
MethodsThis is a prospective descriptive study, conducted in a single center. We included patients referred for coronary angiography from February to November 2006 in whom a CTO was documented with a distal vascular bed of sufficient diameter to accommodate a stent. Ischemia and/or viability of the underlying myocardium was required. The exclusion criteria are shown in Table 1. After the diagnostic coronary angiography and before percutaneous transluminal angioplasty of the occluded vessel, noninvasive MDCT coronary angiography was carried out. All patients signed an informed consent for participation, and the study was approved by the ethics committee of the center. Two experts who were unaware of the patients’ coronary anatomy analyzed the MDCT studies and subsequently reviewed them with the interventional cardiologists.
Table 1. Exclusion Criteria.
| Woman of childbearing age or pregnant |
| Participation in another clinical research protocol |
| Allergy to iodinated contrast material, aspirin, or clopidogrel |
| Severe systemic disease or life expectancy less than 1 year |
| High risk for hemorrhage/high bleeding risk: |
| • Bleeding diathesis |
| • Gastrointestinal disease involving bleeding or a risk of bleeding, recently diagnosed, of unknown cause, or untreated |
| • Genitourinary tract disease |
| • Respiratory tract disease: hemoptysis in study, pulmonary neoplasm pending treatment |
| Impossible to follow prolonged dual antiplatelet therapy |
| Platelet deficit or renal failure (creatinine >2 or clearance <30 mL/min) |
| Lack of adequate vascular access |
| Oral anticoagulant treatment |
A 64-detector Toshiba Aquilion® system (Toshiba Corporation, Medical Systems Company, Tokyo, Japan) was used for all studies. Fast acquisition without contrast enhancement was performed to quantify coronary artery calcifications, and continuous helicoidal acquisition was carried out for noninvasive coronary angiography. Patients received 60 to 90mL of iobitridol. Using a bolus tracking technique, acquisition started when a threshold of 140 Hounsfield units (HU) was reached in the aortic root. Various segmental volumes were retrospectively reconstructed using 0.4 to 0.5mm slices and temporal resolution of 80ms to 120ms. Intravenous metoprolol was administered to achieve heart rates of <70bpm. Studies in atrial fibrillation were not excluded. Postprocessing was performed with Vitrea® 2 software (Vital images, Plymouth, Minnesota, United States). Tools involving 2-dimensional and 3-dimensional techniques were available, including maximum intensity projection and volume rendering.16
The study of plaque composition is based on the differing attenuation capacity of tissues according to their composition. The degree of attenuation is expressed in HU. From findings obtained in post mortem studies, cut-offs have been determined to define the various components: predominantly lipid, ≤60 HU; mixed plaques, 61-119 HU; and calcified plaques, ≥120 HU.17
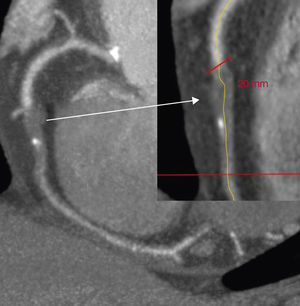
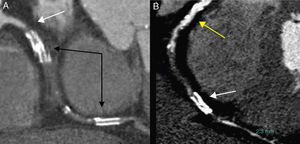
The following were analyzed by MDCT: location of the occlusion; size of the occluded-diseased segment (Figure 1); HU of the occluded segment, divided into thirds (proximal, middle, and distal); calcium distribution in the occluded segment in quadrants (affecting 0%, 25%, 50%, 75% or 100% of the vessel cross-section in each third) (Figure 2); presence of branches at the proximal and distal ends of the CTO, morphology of the origin, angulation of the occlusion, proximal and distal diameter of the vessel, and presence of ipsilateral intracoronary collateral circulation and intercoronary collateral circulation.
Figure 1. Measuring the length of the occlusion.
Figure 2. Quantifying calcium in the proximal, middle, and distal thirds. A: chronic total coronary occlusion with mild calcification, proximal (99 HU), middle (156 HU), and distal (127 HU). B: chronic total coronary occlusion with severe calcification, proximal (247 HU), middle (409 HU), and distal (212 HU). HU, Hounsfield units.
Revascularization TechniqueThe reperfusion strategy was individualized. In patients with multivessel disease who were optimal candidates for surgery, reperfusion was initiated through the occluded vessel and patients were referred for surgery if the technique failed. In patients who were poor candidates for surgery, revascularization was initiated through the patent vessels. The time interval between procedures was approximately 1 month to minimize the risk of contrast-induced nephropathy and excessive X-ray exposure.
An anterograde access was performed, using guide wires specially designed for CTO angioplasty. The sequence of device use, type of device, and manipulation technique were left to the operator's discretion.
To minimize procedure-associated risk,18 the intervention was halted when >300mL of contrast was needed, duration was >90min, or fluoroscopy time was >30min without having crossed the occlusion with any guide wire.
The following were evaluated: location and length of the occlusion, severity of calcification of the occlusion and of the vessel (null, mild, moderate, severe), presence of branches near the CTO proximal and distal ends, morphology of the origin and angulation of the occlusion, reference diameter, and quality and origin of collateral vessels.
In the analysis of the results, the following definitions were used:
• Successful crossing of CTO with the guide wire: the guide wire is advanced in the true lumen to the distal bed of the occluded vessel.
• Procedure success: normal flow in the treated vessel, with <30% residual stenosis and no angiographic complications.
We decided to focus the results on the variable “failure to advance the guide wire” across the lesion, since this is the most common cause of failed revascularization described in the literature19 and possibly the one most closely linked to the anatomic characteristics of the plaque.
Statistical AnalysisIn the description of baseline data, the mean ± standard deviation (range) was used for continuous variables and the number (%) for categorical values. The angiographic and MDCT characteristics of lesions in failed procedures were compared with those in successful procedures. Continuous variables with a normal distribution were compared with the Student t test for independent samples and those with a non-normal distribution with the nonparametric Mann-Whitney U test. Categorical variables were compared with the chi-square test, or with the Fisher exact test when the expected frequency in any cell on the contingency table was <5.
Subsequently, the potential predictors of procedure failure were analyzed by calculating the odds ratio (OR) with logistic regression models. Two models were initially developed to determine which angiographic variables and which MDCT variables were potential predictors of procedure failure; that is, those that showed statistical significance (P<.2) in the bivariate analysis. Forward and backward stepwise selection was used to choose the variables associated with the event of interest.
Because of the small number of events, only 2 statistically significant variables were selected, one angiographic variable and one MDCT variable. Starting with the initially selected variables, the model was refined by entering other variables considered relevant and that could be a source of confusion because their introduction in the model might vary the magnitude of the association to a clinically relevant degree. Specifically, the following were forced in the model as adjusting variables: tapering shape, presence of a distal branch, and unknown duration of the occlusion.
ResultsOver the period of study, 875 angioplasties (82 CTOs; success rate, 62%) were performed in our center. A total of 216 cases of CTO were diagnosed, and 143 cases were excluded from the study protocol because patients did not meet the inclusion criteria or because another treatment was considered more appropriate. The main reason for exclusion was referral for surgery (36%). Among the 73 remaining patients, 2 died before treatment and 2 others withdrew from the protocol. Thus, the study population was comprised of 69 patients, with a mean age of 63 years (SD 9) and 84% were men. The patients’ clinical characteristics are shown in Table 2. Almost half the sample had experienced a previous myocardial infarction, which was in an inferior location in 62%.
Table 2. Clinical Characteristics.
| Patients | 69 |
| Age, years | 63.4±9.6 |
| Women | 11 (16) |
| Weight, kg | 79.9±14 |
| Height, cm | 166±7 |
| NYHA functional class | |
| I | 7 (10) |
| II | 48 (70) |
| III-IV | 14 (20) |
| HT | 54 (78) |
| DLP | 53 (77) |
| Diabetes mellitus | 26 (38) |
| Smoking | 48 (69) |
| History of STEMI | 29 (42) |
| NSTEMI | 4 (14) |
| Previous coronary surgery | 10 (14) |
| Previous angioplasty | 24 (35) |
| Peripheral vascular disease | 13 (19) |
| Stroke | 2 (3) |
| Carotid disease | 1 (1) |
DLP, dyslipidemia; HT, hypertension; NSTEMI, non-ST segment elevation acute myocardial infarction; NYHA, New York Heart Association; STEMI, ST segment elevation acute myocardial infarction.
Data are expressed as no. (%) or mean±standard deviation.
Seventy-seven CTOs were treated. In 62% of patients, the other vessels apart from the occluded one showed no stenosis, whereas the remaining patients had multivessel disease. In 84% of patients, 1 vessel was occluded and in the remaining patients, 2 vessels. The age of the occlusion could be inferred in 71% of the sample and yielded a mean of 47 months (SD 62; range 3-300). The mean left ventricular ejection fraction was 67% (SD 13%). The right coronary territory was clearly predominant (55%). The diameter of the reference vessel was 2.6mm (SD 0.6) and the length of the occlusion, 19.9mm (SD 14.3, range 6-69).
Most CTOs were classified as having no calcifications or mild calcifications (64%). The remaining angiographic characteristics are shown in Table 3.
Table 3. Angiographic Characteristics and Predictors of Successful Revascularization.
| Total (77 lesions) | Guide wire success (n=53) | Guide wire failure (n=24) | p | |
| Occluded vessels | .900 | |||
| 1 | 61 | 42 (79) | 19 (79) | |
| 2 | 16 | 11 (21) | 5 (21) | |
| Diseased vessels | .200 | |||
| 1 | 43 | 33 (62,5) | 10 (42) | |
| 2 | 23 | 14 (26) | 9 (37) | |
| 3 | 11 | 6 (11,5) | 5 (21) | |
| EF ventriculography | 61 (15) | 60 (11) | .700 | |
| Duration occlusion, months | 47±62 (3-300) | 46±71 | 51±35 | .030 |
| Duration occlusion unknown | 13 (24) | 9 (37) | .200 | |
| Diameter, mm | 2.65±0.60 (1.37-4.75) | 2.6±0.5 | 2.7±0.8 | .800 |
| Length CTO, mm | 19.9±14.3 (4.8-69.3) | 18.8±12 | 23.1±19 | .700 |
| Calcium lesion >1 | 28 (36) | 17 (32) | 11 (46) | .200 |
| Calcium lesion 3-4 | 12 (15) | 7 (13) | 5 (21) | .500 |
| Calcium vessel >1 | 25 (32) | 14 (26) | 11 (46) | .090 |
| Calcium vessel >2 | 8 (10) | 3 (6) | 5 (21) | .090 |
| Curve >45° | 28 (36) | 14 (26) | 14 (58) | .007 |
| Tapering | 52 (67) | 39 (73) | 13 (54) | .090 |
| Proximal branch | 43 (56) | 28 (53) | 15 (62) | .400 |
| Distal branch | 30 (39) | 17 (32) | 13 (54) | .060 |
| Ostia | 10 (13) | 6 (11) | 4 (17) | .400 |
| Bifurcation | 23 (30) | 15 (28) | 8 (33) | .600 |
| Restenosis | 8 (10) | 8 (15) | 0 | .050 |
| Good quality collaterals | 24 (71) | 16 (69) | 8 (72) | 1 |
| Rentrop 3 | 33 (43) | 23 (44) | 10 (42) | .050 |
CTO, chronic total coronary occlusion; EF, ejection fraction.
Calcium lesion: 0, none; 1, mild; 2, moderate; 3, severe (persistent vessel wall opacification visible in more than one view, affecting the entire vessel lumen in more than one view).
Marked curve: angle of more than 90° between the proximal patent vessel and the occlusion.
Proximal branch/distal branch: branches originating within 3mm of the proximal or distal ends of the CTO.
Good quality collaterals: when the distal vessel opacifies with contrast material to a density similar to the proximal vessel.
Rentrop classification: 0, no filling; 1, filling of side branches alone; 2, partial filling of epicardial vessel; 3, complete filling of epicardial vessel.
Data are expressed as no. (%) or mean±standard deviation (range).
In 4 occlusions, MDCT information was not available. In another 5, complete data could not be analyzed because of the quality of the study (4 because of deficient distal filling and 1 due to motion artifacts). For the analysis of calcium deposition, lesions treated previously by stent implantation were excluded (Figure 3) because metal has an appearance and density similar to calcium, which could lead to erroneous conclusions in the analysis.
Figure 3. Occluded coronary arteries with previously implanted stent. A: right coronary, middle and distal stent; high-density image (black arrows), occlusion of the artery immediately proximal to the first stent (white arrow). B: total chronic coronary occlusion difficult to evaluate because of an intense proximal calcification (yellow arrow) of the vessel, middle occlusion, and distal stent (white arrow).
Calcium density was greater in the proximal third of the occlusion (219 HU, SD 195) than in the distal third (152 HU, SD 102). In addition, more extensive calcium infiltration was seen in the proximal than in the distal third (calcium occupation 50%-75% of the lumen arc in 30% vs 16% of vessels, respectively). The MDCT characteristics of the CTOs studied are shown in Table 4.
Table 4. Multidetector Computed Tomography Characteristics of Total Coronary Occlusions and Predictors of Revascularization Failure.
| Valid patients | Total (n=73) | Guide wire success (n=51) | Guide wire failure (n=22) | P | |
| Reference diameter, mm | 72 | 3.6±0.8 | 3.5±0.7 | 3.8±0.9 | .20 |
| Length of occlusion, mm | 68 | 22.6±16.6 (3-90) | 22±17.2 | 24±15.5 | .40 |
| Length of lesion, mm | 66 | 44.2±24.8 (7-100) | 42.5±25 | 48.4±24 | .40 |
| Composition of occlusion, HU | |||||
| Proximal | 69 | 219±195 (50-1270) | 194±146 | 280±278 | .10 |
| Middle | 69 | 180±133 (6-933) | 186±153 | 165±64 | .60 |
| Distal | 68 | 152±102 (23-688) | 156±109 | 141±83 | .60 |
| Arc of calcium, proximal | 66 | .04 | |||
| No calcium | 26 (40) | 21 (48) | 5 (23) | ||
| <50% | 30 (45) | 18 (41) | 12 (54) | ||
| >50% | 10 (15) | 5 (11) | 5 (23) | ||
| Arc of calcium, middle | 66 | .03 | |||
| No calcium | 32 (48.5) | 24 (54.5) | 8 (36) | ||
| <50% | 30 (45.5) | 16 (36.5) | 14 (67) | ||
| >50% | 4 (6) | 4 (9) | 0 | ||
| Arc of calcium, distal | 66 | .09 | |||
| No calcium | 31 (47) | 20 (46) | 11 (50) | ||
| <50% | 26 (39) | 19 (43) | 7 (32) | ||
| >50% | 9 (14) | 5 (11) | 4 (18) | ||
| Distal bed, mm | 56 | 2.3±0.5 (1.5-4.1) | 2.3±0.5 | 2.3±0.3 | .40 |
| More than one angle | 72 | 31 (40) | 22 (44) | 9 (41) | 1 |
| Shape of occlusion | 62 | .50 | |||
| Tapering | 28 (45) | 19 (42) | 9 (53) | ||
| Blunt | 34 (55) | 26 (58) | 8 (47) | ||
| Proximal branch | 73 | 47 (64) | 33 (65) | 14 (64) | .90 |
| Distal branch | 70 | 41 (58) | 27 (56) | 14 (64) | .60 |
| Calcium score, HU | 36 | 824±796 | 743±717 | 1040±1013 | .40 |
| p25-p50-p75 | 217-563-1066 | 195-525-1009 (n=27) | 279-650-1870 (n=9) |
HU, Hounsfield units.
Unless otherwise indicated, data are expressed as mean±standard deviation or no. (%).
There was a mean of 1.3 revascularization attempts per patient (SD 0.7, range 1-4), mean duration of the procedure was 73min (SD 64), fluoroscopy time was 42min (SD 19), and 302mL (SD 151) of contrast was used.
The procedure was a complete success in 62% of vessels. The main cause of failure was inability to cross the occlusion with any angioplasty guide wire (80% of all failures) and the second most common cause was inability to dilate the lesion with any balloon catheter (10%).
Complete revascularization (vessels with CTO and vessels with significant lesions) was achieved in 55% of patients. Among all revascularized patients, 94% received drug-eluting stents (2.2 stents/lesion, SD 1.1; longitude with stent 50mm, SD 27).
Angiography Factors and Multidetector Computed Tomography Factors Associated With Procedure OutcomeThe angiographic features of CTO as related to success (group 1) or failure (group 2) in crossing the occlusion with the angioplasty guide wire are shown in Table 3. The presence of occlusive restenosis of a previously implanted stent was identified as a favorable factor, whereas CTO of longer duration was significantly associated with failure of the technique. The most powerful unfavorable variable in the univariate analysis was the presence of a >45° curve between the patent vessel and the origin of the CTO (P=.007). The MDCT features of the CTOs studied are described in Table 4.
Calcium density in the proximal third of the CTO was greater in group 2 than in group 1, but differences did not reach significance.
Cross-sectional analysis of calcium distribution in the CTO disclosed an association between the arc of calcium in the proximal and middle thirds in group 2. In the proximal segment there was a significant difference in the success rate according to the calcium strata; that is, success was 41% in lesions whose proximal segment had <50% arc of calcium and 11% in those with >50%. Similarly, procedure success was 36% in occlusions whose middle segment had <50% calcium involvement vs 9% for those with >50%.
On multivariate logistic regression analysis (Table 5), the independent negative predictive factor identified for angiography was the presence of a marked curve of the CTO with respect to the patent vessel (OR 3.8; 95% confidence interval [95%CI], 1.2-12; P=.02), whereas for MDCT it was the mean arc of calcium (OR 3.6; 95%CI, 1-12; P=.04). Each of these factors conferred a 3-fold greater possibility of failure of the guide wire to cross the lesion.
Table 5. Multivariate Analysis of Angiographic and Multidetector Computed Tomography Factors Associated With Success of the Revascularization Technique for Total Coronary Occlusions.
| OR (95%CI) | P | |
| Arc of calcium, middle | 3.6 (1-12) | .04 |
| Marked curve | 3.8 (1.2-12) | .02 |
| Tapering * | 0.49 (0.15-1.60) | .20 |
| Distal branch * | 3.1 (0.9-10) | .05 |
| Duration of occlusion unknown * | 2.6 (0.7-9.3) | .10 |
95%CI, 95% confidence interval; OR, odds ratio.
* Included as adjusting variables.
Calcification of CTO has been classically associated with revascularization failure. The presence of calcium at the point of entry of an occlusion hinders penetration with the angioplasty guide wire, and calcification in the body of the lesion can cause the guide wire to deviate toward a subintimal plane.20
Visualization of calcium on angiography depends on several factors, including the characteristics of the X-ray equipment used and various peripheral factors, such as air trapping in the lungs and obesity, among others. Therefore, there is no correlation between the data obtained by angiography and MDCT. Calcium measurement is one of the limitations of angiography: in addition to being a subjective parameter, it is easily underestimated. We found that in some patients, angiography showed little or no calcium density, whereas on MDCT it was seen to be severe. Unfortunately, there are no available parameters to transfer this impression to numbers so that this finding can be quantified.
Use of MDCT is effective for analyzing CTO composition. We documented greater calcium density in the proximal third than in the remainder of the CTO, in keeping with the findings from previous experimental21 and clinical studies.15
It is known22 that MDCT does not have sufficient positive and negative predictive performance to replace angiography in the diagnosis of coronary disease in symptomatic patients. Nonetheless, it is very useful for detecting and analyzing calcium deposition in the coronary vasculature.23, 24
The first report in which MDCT was used in the study of CTO was published by Mollet et al.14 These authors used 16-detector MDCT in 45 patients, and the independent predictive factors of revascularization failure were an occlusion length >15mm, blunt morphology of the proximal CTO, and the presence of severe calcification (calcium density >130 HU affecting >50% of the vessel wall on sagittal slices). In our study, the so-called “classic angiographic factors” of failure were irrelevant. This may be due to the improvements in the material used, particularly the development of guide wires with a greater power of penetration and new techniques for their manipulation.25
Stressing this aspect, a study by Qu et al.26 analyzing 17 CTOs supports the notion that the “classic angiographic factors” are currently not in force and that the only factor associated with revascularization failure is >50% calcification of the vessel, which was seen in 83.3% of failures and 16.7% of successful procedures; P=.05).
Later on, Cho et al.27 analyzed the regional calcium score (area of calcification×weighted maximal CT attenuation: [1, 130-190 HU; 2, 200-299 HU; 3, 300-399 HU, and 4, >400 HU]), total calcium score, regional calcium volume (number of vessels with attenuation >130 HU/vessel volume) and the percentage of calcification of the vessel section (percentage of calcified area/vessel area at the site of maximum calcification). Although all the parameters studied were significantly associated with technical failure, upon multivariate analysis the only factor showing a high positive predictive power was the amount of calcification in the vessel section. Our findings corroborate this data; the only factor significantly associated with revascularization failure was the presence of calcium affecting more than 50% of the vessel circumference in the proximal and middle thirds of the CTO.
Ehara et al.28 reported the results of the first study investigating MDCT in CTO in which revascularization was carried out by experts in this field; that is, specialists with a previous experience of more than 100 cases. The authors included 110 lesions and identified 3 independent predictive factors of guide wire failure to cross the lesion: presence of a marked curve at the CTO with respect to the native vessel (57% of successful procedures vs 95% failures, P<.0001), negative remodeling at the proximal end of the CTO (44% of successful procedures vs 88% of failures, P=.0005), and severe calcification, defined by high-density plaques (>500 HU) affecting nearly 360° of the vessel circumference (71% of successful procedures vs 88% of failures, P=.0356). In the present study, we were unable to adequately assess the presence of a curve between the native vessel and the CTO on MDCT, but on angiography this was the only independent factor predictive of failure, which concurs with the findings of Ehara et al.28
The study of Hsu et al.,29 performed in 82 CTOs, evaluated the calcification length ratio, defined as the length of calcification with density >130 HU/occlusion length. An expert performed the procedures and the successful revascularization rate was 80.5%. A calcification length ratio >0.5 was found in 77.8% of technical failures and 50% of procedure failures (P<.001).
As compared to previous efforts, our study has two advantages. First, it focuses the areas of interest on two segments of the CTO, the proximal and middle thirds, which makes sense in pathophysiologic terms. Second, it simplifies the CT analysis and reduces the time needed to interpret the study. The evaluation involves taking a simple cross-sectional slice at the levels indicated above and measuring the percentage of the vessel arc affected by calcification.
Although MDCT is an effective tool, its use implies exposure to radiation and contrast material30; therefore, and with a view to the results of our study, we do not believe it should be routinely applied in all patients with CTO. Its use should be limited to particularly complex cases (very long or tortuous occlusions, with severe calcification) and previous failures in which the precise reason is uncertain. In individual cases, the data from this study can help to decide on a change in the type of material to use or the most appropriate revascularization strategy.
LimitationsThe main limitation of this study is the small sample size and limited number of events (n=23), which may have hindered detection of potentially relevant predictors of failure. In addition, it made calibration of the model difficult and limited the number of variables that could be included to avoid problems derived from excessive adjusting.
Although the angioplasties were performed by only two operators, both were at the beginning of their learning curve in the treatment of this type of lesion; thus, only anterograde revascularization was used. The results may improve if the retrograde technique is used.
ConclusionsIn patients with CTO, a more than 50% arc of calcification in the proximal and middle thirds of the occlusion seen on MDCT is predictive of revascularization failure. In highly selected cases, MDCT study could be a useful tool prior to revascularization.
Conflicts of interestNone declared.
Acknowledgments
This study was supported by funding from Fundació La Marató de TV3 (record number, 082130).
Received 12 July 2011
Accepted 2 November 2011
Corresponding author: Secretaría de Cardiología, Hospital Clínic, Villarroel 170, escalera 3, 6.a planta, 08036 Barcelona, Spain. 27700vmy@comb.cat