Keywords
INTRODUCTION
Heart failure (HF) is one of the most important cardiovascular health problems in Europe. Epidemiologic study data indicate a high prevalence and HF is currently one of the most frequent causes of hospitalization in patients >75 years.1-5
Despite publication of the European Society of Cardiology (ESC) revised Guidelines for the diagnosis and treatment of chronic HF in 2001,5 results of recent studies6-12 suggest many patients do not receive adequate treatment. This is especially noticeable in the prescription of angiotensin converting enzyme (ACE) inhibitors and beta-blockers to improve symptoms and prognosis. Ambulatory management of HF involves a population of unselected patients who may differ from those enrolled in major clinical trials13,14 but little information is available about this context. This is particularly interesting because in recent years, despite the appearance of drug treatments that reduce mortality from HF and greater access to diagnostic procedures and therapies, improvements observed in clinical trials do not seem to have led to better prognosis in the general population.15
The present study was designed to identify baseline characteristics and patterns of diagnosis and treatment of outpatients diagnosed with HF. Recent epidemiologic studies have referred to the quality of treatment of patients discharged with HF in Europe.16,17 However, we would hope to gain more precise knowledge of the characteristics of management of these patients to enable us to identify specific aspects of outpatient clinical practice that can be improved and initiate appropriate measures.
MATERIAL AND METHODS
The present study was conceived of and initiated by the Council for Cardiology Practice of the European Society of Cardiology, which has led a follow-up of the clinical characteristics and therapeutic management of outpatients with HF. The Council represents over 5000 cardiologists in private practice or outpatient cardiology clinics. The study involved 465 cardiologists in France, Germany, and Spain. Data was drawn from cardiologists' opinions submitted in a specially designed questionnaire thru which they specified the characteristics of all patients with HF examined on a single day: April 26, 2001. The study sample was chosen as follows: in France questionnaires were sent to 400 Council members by fax and e-mail; in Germany questionnaires were sent to 500 members by fax; and in Spain pharmaceutical company representatives distributed questionnaires to 250 cardiologists belonging to the Section for Outpatient Cardiology. Participants received no financial reward for responding to the survey.
To facilitate the process, we designed a simple patient data collection sheet including the following sections:
1. Demography: nationality, gender, age, height, weight
2. Diagnosis: date of diagnosis of HF, date of first symptoms, who made the diagnosis (cardiologist, general practitioner, hospital, other), how primary diagnosis of HF was made (several options possible): symptoms, signs, electrocardiogram (ECG), chest x-ray, echocardiogram, angiography, other techniques.
3. Etiology of HF: ischemic heart disease, hypertension, dilated cardiomyopathy, valvular heart disease, other, unknown.
4. Clinical data: New York Heart Association (NYHA) functional class at clinic, presence of risk factors (smoking, hypertension, hypercholesterolemia, diabetes), existence of atrial fibrillation, left branch bundle block; during the previous 12 months, did patients visit their doctors because of HF? Were they hospitalized? Were they admitted to an intensive care unit (ICU)? Who took charge of day-to-day management of the patient? (cardiologist, general practitioner, nurse, other).
5. Treatment: current drug regimen (explaining non-prescription of diuretics, ACE inhibitors or beta-blockers, if applicable).
Statistical Analysis
Quantitative variables are expressed as mean ± standard deviation and we compare means between groups by analysis of variance. Categorical variables are described as percentages and comparisons between groups are made with the Chi-squared test. We calculate 95% confidence intervals (CI) for the main results.
RESULTS
Some 465 cardiologists participated in the study: France 165 (35%), Germany 123 (26%), and Spain 177 (39%). Survey response rates were France 41%, Germany 24%, and Spain 70% (P<.01). A total of 1252 patients were studied. The distribution of patients by country was, France 282 (22%), Germany 472 (38%), and Spain 500 (40%). The number of patients per cardiologist by country was France 1.7, Germany 3.8, and Spain 2.8.
Demographic Characteristics
Men accounted for 62.1% of the total patient population and the distribution by country was France 66.1%, Germany 66.5%, and Spain 55.6% (P=.0001).
The mean age of the sample was 68.3±12.1 years, with differences in the distribution by country: France 71.2 years (95% CI, 69.6-72.9), Germany 65.3 years (95% CI, 64.2-66.4), and Spain 69.3 years (95% CI, 68.3-70.3) (P<.0001).
The average height of patients was 167.9±9.4 cm; average weight was 76.2±14.5 kg, and average body mass index was 27.0±4.5, with no differences between countries.
Diagnosis
First diagnosis of HF was made during the previous year in 28.3% of patients, 2 years earlier in 20.4%, 3 years earlier in 14%; and ≥4 years earlier in the remaining 37.3%.
First symptoms of HF were experienced during the previous year in 27.9% of patients, 2 years earlier in 18.5%, 3 years earlier in 14.5% and ≥4 years earlier in the rest.
The overall average delay between the appearance of the first symptoms and diagnosis was 0.61±1.8 years.
In most cases (56.5%), diagnosis was made by the outpatient clinic cardiologist (France 63.7%, Germany 54.3%, Spain 54.5%). Diagnosis was made in-hospital in 32% of patients (France 26.4%, Germany 32.2%, Spain 35%), by the general practitioner at clinic in 9.2% (France 8.3%, Germany 10.3%, Spain 8.6%), and in other situations in 2.3%. We found significant differences between countries (P=.02).
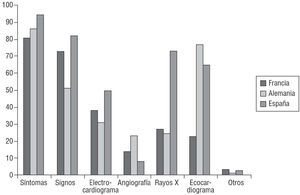
Primary diagnosis of HF was made on the basis of(several options possible) symptoms in 88.6% of patients (France 81.4%, Germany 87.3%, Spain 94%), signs in 68.1% (France 72.8%, Germany 50.8%, Spain 81.8%), echocardiogram in 59.8% (France 22.5%, Germany 76.6%, Spain 64.8%), x-ray in 44.5% (France 27.1%, Germany 24.3%, Spain 73.4%), ECG in 40% (France 37.5%, Germany 31.3%, Spain 49.8%), conventional invasive cardiac angiography in 15% (France 14.3%, Germany 23%, Spain 8%) and other imaging methods in 2%. We found significant differences between countries for all variables: symptoms (P<.0001), signs (P<.0001), echocardiogram (P<.0001), x-ray (P<.0001), ECG (P<.0001), angiography (P<.0001) (Figure 1).
Figure 1. Method employed in primary diagnosis of heart failure in percentages. Angio indicates angiography; ECG, electrocardiogram; Eco, echocardio- gram.
Clinical Characteristics
During the previous 12 months, 78% of patients were seen at least once because of HF: France 68% (95% CI, 62%-74%), Germany 86.2% (95% CI, 83%-90%), and Spain 75.6% (95% CI, 72%-79%). We found differences between countries (P<.0001).
The mean number of visits during the previous 12 months was: France 3.1, Germany 5.2, and Spain 2.7 (P<.0001).
The mean percentage of patients with at least one hospitalization during the previous 12 months was 36.2%. The distribution by countries showed no differences (P=NS): France 37.5% (95% CI, 32%-44%), Germany 35.7% (95% CI, 32%-40%), Spain 36.1% (95% CI, 33%-40%).
The mean number of hospitalizations per country in the previous 12 months was: Germany 1.7 followed by France 1.5, and Spain 1.5 (P=NS). The accumulative mean number of days of hospitalization was: 17.9, 13.2, and 10.7 days respectively (P<.0001). The global percentage of patients admitted to an ICU during the previous 12 months was 12.4%: France 26.5% (95% CI, 20%-33%); Germany 14.1% (95% CI, 11%-17%), Spain 5.8% (95% CI, 3%-7%). We found differences in the distribution by country (P<.0001).
The mean number of days of hospitalization in an ICU by countries was: Germany 5.1 days, followed by France 4.4, and Spain 4.4 (P=NS).
Outpatient Management
The physician in charge of outpatient management was: cardiologist 46.2% (France 63.9%, Germany 29.4%, Spain 52.3% [P<.0001]); general practitioner 31.9%. Management was the joint responsibility of a cardiologist and a general practitioner in 16.6% of patients. The distribution of normal daily outpatient management by a cardiologist (alone or with other physicians) by country was: France 78.2% (95% CI, 73%-82%); Germany 57.6% (95% CI, 52%-61%), Spain 61.6% (95% CI, 58%-66%). The distribution of normal daily outpatient management by a general practitioner (alone or with a cardiologist) was: France 31.8% (95% CI, 27%-38%); Germany 65.5% (95% CI, 61%-70%), Spain 44% (95% CI, 40%-48%) and differences were again significant (P<.0001). Endocrinologists, internists and nephrologists also managed these patients (3.8%).
Etiology of Heart Failure
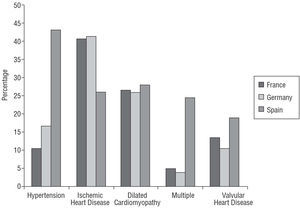
The principle causes of HF (alone or in combination) were: hypertension 26.1% (France 10.7% [95% CI, 7%-14%], Germany 16.7% [95% CI, 13%-20%], Spain 43.6% [95% CI, 39%-48%]; P<.0001); ischemic heart disease 35% (France 40.7% [95% CI, 35%-47%], Germany 41.3% [95% CI, 37%-46%], Spain 26% [95% CI, 23%-30%]; P<.0001); dilated cardiomyopathy 26.9% (P=NS); valvular heart disease 14.5% (P=NS); arrhythmia 0.2% (P=NS); chronic obstructive pulmonary disease (COPD) 0.15% (P=NS); multiple 12.3% (France 5% [95% CI, 3%-7%], Germany 3.8% [95% CI, 2%-6%], Spain 24.4% [95% CI, 21%-28%]; P<.0001). The distribution by countries is shown in Figure 2.
Fig. 2. Principal reported cause of heart failure (alone or in combination) distributed by country: hypertension, P<.0001; ischemic heart disease, P<.0001; multiple, P<.0001.
On average, 66.4% of the population had a history of myocardial infarction although we found no differences between countries (France 63.7%, Germany 69.5%, Spain 65%, P=NS).
We found 10.3% of patients were in NYHA functional class I (France 13%, Germany 9%, Spain 10%); 52% in class II (France 59%, Germany 46%, Spain 53%); 28.2% in class III (France 23%, Germany 38%, Spain 21%), and 2.2% in class IV (France 2%, Germany 3%, Spain 1%). We identified differences in the distribution by country (P=.0002).
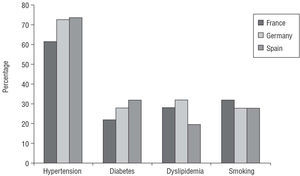
Cardiovascular risk factors present in the study population were: arterial hypertension 71.2% (France 62.6%, Germany 73%, Spain 73.8%); diabetes 28.8% (France 22%, Germany 28.4%, Spain 32.5%); hypercholesterolemia 26.3% (France 27.7%, Germany 32.3%, Spain 20.2%) and smoking 28.9% (France 32%, Germany 27.9%, Spain 28.3%). Differences existed between countries for hypertension (P=.008), diabetes (P=.02), and hypercholesterolemia (P=.0004), but not for smoking (P=NS) (Figure 3). The average number of risk factors per patient by country was: France 1.44, Germany 1.62, and Spain 1.55 (P=.008).
Figure 3. Cardiovascular risk factors in the study population.
Atrial fibrillation was found in 36% of patients (France 33.7%, Germany 28.8%, Spain 44.1% [P<.0001]).
Left branch bundle block was identified by ECG in 23% of patients (France 24.3%, Germany 23.2%, Spain 21.9% [P=NS]).
Treatment
The mean number of drugs prescribed per patient was: France 4.4, Germany 4.6, and Spain 4.3 (P=.008).
The number of drugs by NYHA functional class in the total population was: class I 3.9, class II 4.4, class III 4.7, and class IV 5.0 (P<.0001).
The relationship between mean number of prescriptions and the physician in charge of patient management was: cardiologist 4.5, cardiologist and general practitioner 4.8, general practitioner 4.3, and other 4.0 (P=.001).
We were informed of some 5478 prescriptions in 1198 patients (data was not available for 9 patients in France, 11 in Germany, and 4 in Spain).
The percentage of patients receiving drugs from each of the different groups is shown in Table 1.
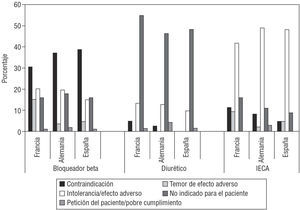
Non-Prescription of Diuretics
Diuretics were not prescribed to 236 (19.7 %) of the 1198 patients. There were no significant differences between countries. Spironolactone, prescribed for 23 of these 236 patients, was not classified as a diuretic. The principal reason given for non-prescription of Spironolactone was "not indicated for this patient." When non-prescription was due to intolerance/adverse effects, the principal reason specified was "hypotension."
Non-Prescription of ACE Inhibitors
Angiotensin converting enzyme inhibitors were not prescribed to 334 (27.9%) of the 1198 patients. There were no differences between countries. The principal reason given for non-prescription was "intolerance/adverse effects" and this was primarily justified as being due to cough, worsening of renal function and hypotension. Kidney failure was the only contraindication given to justify non-prescription of ACE inhibitors.
Non-Prescription of Beta-Blockers
Beta-blockers were not prescribed to 629 (52.3%) of 1198 patients. We found differences between countries: France 63.8%, Spain 53%, and Germany 33.6% (P=.001). The principal reason given for non-prescription was "contraindication." Bradycardia, COPD and asthma were the principal reasons given when non-prescription was justified as due to contraindication or intolerance/adverse effects. Percentages of patients by country and motive for non-prescription are shown in Figure 4.
Figure 4. Percentage of patients by country according to justification of non-prescription.
DISCUSSION
Characteristics of Participating Cardiologists
This study analyzes the attitudes of cardiologists in private practice and outpatient clinics in 3 countries towards the characteristics, diagnosis, and treatment of outpatients with HF. The diffusion and collection of data was carried out in each country following the accepted national procedures for this type of study. In Spain, the questionnaire was delivered and collected personally, which favored a greater level of participation. However, we should recall that the study focused on a single day which may have meant some cardiologists did not participate because they did not attend patients with HF on the day in question.
Survey response rates differ greatly: Spain 70%, France 41%, and Germany 24%. Similarly, the population of cardiologists who completed the study may have differed from that of the general population of cardiologists as in Spain most respondents practice only in outpatient cardiology.
Characteristics of the Patients
Men dominate the patient population in the 3 countries studied in a proportion slightly above that of recent surveys.16-18 Average age (68.3 years) is slightly below that of the aforementioned surveys (mean: 71 or 70 years). We should point out that both the Euro Heart Failure Survey and IMPROVEMENT included a significant number of patients from eastern Europe and given that there is almost ten years difference in age between the study made in the East and that carried out in western Europe, the patients in our study (in west Europe) are considerably younger and there is a high prevalence of men among them. It is noteworthy that the age of patients in Germany (65.3 years) was lower than in the other 2 countries in our study (71.2 and 69.3 years), which may hide a selection bias in the sample.
Diagnosis of Heart Failure
We observed a probable deficiency in the evaluation of cardiac function as only 59.8% of patients were indicated for echocardiogram as the method of primary diagnosis of HF and, moreover, we found differences between countries. This data may reflect a low level of fulfillment of European Society of Cardiology recommendations,5 although it does not reflect the real percentage of patients who underwent echocardiography for HF because, as commented above, this data refers to the method of primary diagnosis of HF and not to whether or not echocardiography was performed. This could explain the low percentage of echocardiograms reported in France (22.5%).
Clinical Management
This study confirms the fact that HF stands out as one of the pathologies that consume a vast amount of medical resources. The mean number of outpatient visits in the previous 12 months, percentage of hospitalizations and number of days of hospitalization in a conventional ward or in an ICU all stand out. Our data confirm that HF is an illness that entails a high health care cost. There is a striking difference between the mean number of outpatient visits during the previous 12 months by country (5.2 in Germany, 3.1 in France, and 2.7 in Spain), which does not seem to prevent subsequent admissions as admission rates in the 3 countries are similar. In the light of these data, we would suggest that greater outpatient control in the previous 12 months did not prevent hospital admissions.
Etiology of Heart Failure
Ischemic heart disease is the most important etiology in France and Germany but in Spain hypertension is the principal cause. In spite of this, the rate of patients with a history of myocardial infarction is very similar. Therefore, additional analysis is needed to determine whether this is a false interpretation of the etiology of HF. This result may be influenced by the fact that in Spain a greater rate of patients with more than 1 etiology has been reported.
Cardiovascular Risk Factors
In Spain, we found comparatively higher rates of patients with hypertension (43.1%) and patients with diabetes (46.9%). These 2 factors are probable etiologic predispositions that influence the progressive deterioration of ventricular function. Diabetes is a risk factor for ischemic heart disease and often coexists with hypertension. In Anglo-Saxon countries, in the last decades, the comparative importance of coronary heart disease as a cause of HF has increased while that of hypertension has declined.19,20
Drug Treatment
In our study the mean number of drugs prescribed was in the range 4.3-4.6, which is similar to recent studies. In the Euro Heart Survey, 70.6% of patients were taking ≥3 drugs and 44.6% were taking ≥4 drugs for HF.16,17 The number of drugs prescribed increases in proportion to NYHA classification.
Diuretics are the most widely used drugs in this study, which coincides with earlier surveys.21-24 Spironolactone was prescribed in 23%-34% of patients, as was suggested in the RALES study.25 Given that this study dates from 2001, no mention is made of the use of eplerenone. The use of angiotensin II receptor antagonists (ARA-II) was low (12.7%-16.1%) but slightly above that reported in the Euro Heart Failure Survey (4.5%)16,17 and the IMPROVEMENT program18 (maximum ~9%). The ESC guidelines for treatment do not recommend its use as first choice treatment. Treatment with digitalis was used for 31.7%-52.4%, a similar proportion to that reported in the Euro Heart Failure Survey (35.7%).16,17 The DIG study showed that digoxin only reduced the rate of hospitalizations in patients in sinus rhythm although it continued to play a role in patients in atrial fibrillation.26
Earlier studies suggest that recommendations of therapeutic drug treatment of HF are not followed sufficiently closely in clinical practice.21-23 The present study shows that treatment with ACE inhibitors and beta-blockers is more common than that described in earlier studies but that these drugs continue to be under used.
In our study population, ACE inhibitors (72.1%) were prescribed more than in earlier studies.27-29 In the recently published Euro Heart Failure Survey,16,17 of 11 304 patients in 115 hospitals in 24 countries, ACE inhibitor prescription averaged 61.8% (range, 40%-85.1%). The IMPROVEMENT of Heart Failure program18 provided data on management of HF in primary care and reported that 60% of 11 062 patients in 14 European countries were prescribed ACE inhibitors. Similar rates have been found in recent studies in Australia and France. In the Australian study,24 only 58.1% of patients received ACE inhibitors. In the French study,22 of 600 outpatients in private practice, the rate was 54%, slightly lower than the results of our study (71.6%). In the EPICAL study, of patients hospitalized with left ventricular dysfunction, 75% received ACE inhibitors.30
Data from clinical trials31,32 and the ESC guidelines5 recommend the use of beta-blockers in HF. According to data from published studies, this drug group is clearly under-prescribed even in patients with documented low ejection fraction. Various factors may explain this: underestimation of the morbidity and mortality of the syndrome, underestimation of the scale of the benefit, fear of potential adverse reactions, clinical profile of the patient, etiology of HF, specialty of treating physician and the pathophysiology of HF. The principal reason given in our study for non-administration of beta-blockers was "contraindication." Bradycardia, COPD, and asthma are the principal reasons cited when non-prescription is justified for contraindication or intolerance/adverse effects. In our study, beta-blockers were prescribed for 47.7% of patients. This is greater than in recent, wide-ranging surveys. In 2003, the Euro Heart Failure Survey16,17 reported 36.9% prescription (10%-65.8%). In 2002, the IMPROVEMENT program18 reported a 30% rate. In the recent French22 and Australian24 surveys, prescription rates were 11% and 12%, respectively. In 1999, the EPICAL study30 of hospitalization data for patients with severe HF due to systolic ventricular dysfunction reported a 5% rate. We should point out the substantial variations found in the rate of prescription of ACE inhibitors and beta-blockers in the different studies. Variation between countries, and even between centers in the same country, is also considerable.
Limitations of the Study
Implicit problems exist in the very design of this study that generate different response rates in the 3 countries. Consequently, differences between countries should be analyzed with caution as they may be evidence of a bias in the selection of cardiologists and patients.
The questionnaire used to gather data may itself be deficient in some sections: the criteria for ischemic heart disease as an etiology of HF are not defined even when the percentage of patients with prior myocardial infarction was the same; dosage of drugs prescribed is not mentioned, nor is a distinction made between different causes of hospitalization.
Correspondence: Dra. M.J. Salvador Taboada.
Institut Universitari Dexeus. Servicio de Cardiología.
Pg. Bonanova, 69, 1.o. 08017 Barcelona. España.
E-mail: mjsalvador@idexeus.es