Keywords
INTRODUCTION
Heart failure is the final outcome in a number of heart diseases. The incidence and prevalence of heart failure are increasing not only because the population is aging but also due to lower mortality rates associated with improved treatment of most heart diseases leading to heart failure, especially ischemic heart disease.1 Advances in the treatment of heart failure, both pharmacological and non-pharmacological, have lowered associated death and disease, at least according to data obtained from clinical trials.2-5 However, these important improvements have not been reflected in those studies and registries which analyze a more general population of patients with heart failure, in whom the rates of death and readmission remain high.6-9 In an attempt to resolve these problems, new organizational strategies for the care of patients with heart failure have been developed, such as interventional and education programs and specific heart failure clinics or units.10-12 Four years ago the Working Group on Heart Failure, Heart Transplantation and Other Therapeutic Alternatives of the Spanish Society of Cardiology set up a registry of heart failure units, the BADAPIC Registry (an acronym for "Base de Datos de Pacientes con Insuficiencia Cardíaca"--database of patients with heart failure). This paper presents the initial results of this registry.
PATIENTS AND METHODS
The BADAPIC Registry is the official registry of the Working Group on Heart Failure, Heart Transplantation and Other Therapeutic Alternatives of the Spanish Society of Cardiology. The registry, set up in 2000 by the Working Group on Heart Failure, is voluntary and so far includes the participation of 62 centers from all over Spain that have specific heart failure units or clinics. The organization and structure of these units vary greatly; each center is free to organize itself in accordance with its health care possibilities. The only requirement for participation in the registry is the existence of a specific office for patients with heart failure and the inclusion of all the patients seen in a common database, which was designed and developed by the Working Group on Heart Failure of the Spanish Society of Cardiology and agreed by consensus of all the participating centers. This database includes more than 100 variables dealing with the main demographic, clinical and analytical characteristics, as well as functional tests, pharmacological and non-pharmacological therapy, and the evolution of the patient. Since the start of the registry in 2002, the data have been collected annually at the end of the year. The data presented here correspond to those collected at the end of 2000, 2001, and 2002. At the end of the year each center provides the data corresponding to all the patients included for the first time in their heart failure clinic or unit as well as updated data (the latest revision) for each patient already included in the BADAPIC database. This first report of the BADAPIC Registry corresponds, therefore, to 2000-2002 and includes the data on 3909 patients from 62 heart failure units or clinics throughout Spain. The participating centers and researchers are shown in Annex 1.
Characteristics of the Participating Units
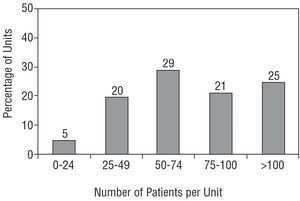
Of the 62 hospitals, 14 (22%) are community hospitals and 48 (78%), general hospitals; 21% of the patients were from the community hospitals and 79% from the general hospitals. Only 10 (16%) of the participating hospitals have a heart transplantation program. Although most units are integrated in cardiology services or areas, eight (13% of the total) depend on the internal medicine service. Figure 1 shows the distribution of the units according to the number of patients included, which ranged from 15-135 per unit. Five percent of the units included at least 25 patients, and 65% included more than 50 patients. Regarding the structural and functional characteristics of the participating units, 18 (29%) have a full-time trained nurse, 8 (13%) have common protocols with their primary care areas with established criteria and referral route, but only 3 (5%) have home health care programs. Half the units, 31, have facilities for their patients to consult them over the telephone or provide free access to the unit without the prior need for an appointment. Most of the units (52, 84%) only have cardiologists, from 1-3 per unit, with internists, geriatricians, psychologists, and social care workers collaborating in the remaining 10 units.
Figure 1. Distribution of the units participating in the BADAPIC Registry according to the number of patients included from each unit.
Inclusion Criteria and Definition of the Variables
The diagnostic criteria for heart failure and the definition of the terms and variables to be included in the database were agreed by all the participating units and drawn up in a common written protocol and in the BADAPIC database. The diagnosis of heart failure was made according to the criteria of the Working Group on Heart Failure of the Spanish Society of Cardiology13 and, with effect from 2001, the criteria of the European Society of Cardiology,14 after agreement of all the participating researchers. The units included the data related to the first visit to the heart failure clinic by each patient diagnosed with heart failure, as well as the annual follow-up data. The database does not include patients who were diagnosed with heart failure in each hospital but not studied by the heart failure unit or patients who were referred to the units for study and in whom heart failure was excluded. The protocols for the diagnosis and treatment of the patients, as well as the methods of exclusion of other diseases causing symptoms indicative of heart failure, were decided by each unit.
The normal criteria were used for the definition of the clinical, pathophysiological, and etiological variables included in the database, such as high blood pressure, diabetes mellitus, and dyslipidemia (Tables 1 and 2). The presence of ischemic heart disease was defined by the presence of clinical, electrocardiographic, or angiographic data suggestive of ischemia or myocardial necrosis. The etiology of heart failure was established in each case by the researcher in charge at each center. Although more than one etiological cause may have been present in the same patient, the researcher selected the cause considered to be the most important in that particular patient. Valvular disease was considered to be important and causative of the heart failure when echocardiography or cardiac catheterization showed the presence of stenosis, or at least moderate valvular insufficiency. High blood pressure was established as the cause of heart failure when no data suggested ischemic heart disease or any other clinically important cardiac disorder. Idiopathic dilated cardiomyopathy was diagnosed when the left ventricle was dilated and the ejection fraction was below 45%, in the absence of other cardiac disorders. Heart failure with preserved systolic function was diagnosed when the ejection fraction was equal to or higher than 45% and with depressed systolic function when the ejection fraction was below 45% (whatever the etiology).
The protocol established that a patient was considered to have had a complementary test (Table 3) when the test was undertaken during the initial visit to the heart failure unit, or during the previous 6 months if the researcher in charge considered that no important clinical changes had taken place during this period. In the case of repeat tests, the result included in the database was that of the last test performed during the relevant time period. The data regarding pharmacological treatment shown in Tables 4, 5, and 6 are those of the treatment planned after the initial visit.
Patient Observation
The frequency of the revisions depended on the clinical judgment of each participating physician, although the follow-up data (changes in treatment and clinical events) were provided annually by each center. The follow-up data analyzed included mortality, admissions for heart failure, acute myocardial infarction, coronary revascularization, valvular surgery, or heart transplant. Analyses were made, according to the methods and tests mentioned in the section on statistical study, of the likelihood of survival, admission due to heart failure and survival free of important cardiac events (those cited previously); this latter variable referred to the first important cardiac event suffered by a patient.
Statistical Study
The descriptive analysis was made using percentages for the distribution of frequencies and the mean ±1 standard deviation for quantitative variables. Comparison of the differences between the various subgroups of patients was made using the *2 test for qualitative variables and the Student t test for quantitative variables. The probability of survival and events during the follow-up was calculated by the Kaplan-Meier test, using Mantel's log rank test to compare the survival curves between subgroups.
RESULTS
Demography
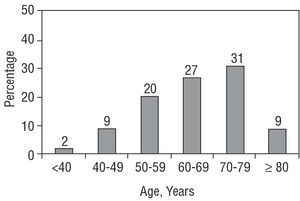
As mentioned, the registry included data for 3909 patients between 2000 and 2002 from 62 heart failure units or clinics throughout Spain (Annex). The age of the patients was 66±12 years. Figure 2 shows the distribution of the patients according to the different age groups. The most common age group was the decade from 70-79 years, with 9% (359 patients) aged 80 years or older; the percentage of patients younger than 50 years of age was very low (11%, 430 patients). Sixty-seven percent of the patients (2619) were men and 33% (1290) were women. The referral to the heart failure clinic or unit was made mainly by cardiologists (72% of all the patients, 2382 cases), although 5% (195) were referred from primary care and 23% (1332) from the internal medicine service or other specialties.
Figure 2. Distribution according to the age of the patients included in the BADAPIC Registry.
Cardiovascular History
Table 1 shows the prevalence of the main cardiological findings during the initial workup, in the overall group and according to the sex of the patient. Notably, 54% (2111) of the patients had high blood pressure and 48% (1013) of these patients had not had their blood pressure controlled during the previous 6 months; this percentage of poor blood pressure control fell to 8% (312 cases) 6 months after the initial visit to the heart failure unit. A history of hyperlipidemia was present in 35% (1368) of the patients and diabetes in 30% (1173). Forty percent (1563) of the patients had a history of ischemic heart disease, 29% (1134) had had a previous myocardial infarction and 14% (547) had undergone coronary revascularization surgery. As seen in Table 1, no differences were detected between men and women in the percentage patients with hyperlipidemia, valvular disease, prior valvular operations, or prior admissions for heart failure. Diabetes mellitus and high blood pressure were significantly more common in women, whereas a history of ischemic heart disease, myocardial infarction, or coronary revascularization were more common in men (Table 1).
Most patients had a long history of heart failure. Only 26% (1016) of the patients had a history of symptoms of heart failure shorter than 1 year, whereas 45% (1498) of the patients had a symptomatic history of heart failure longer than 3 years. Sixty-eight percent (2658) of the patients had been admitted at least once for heart failure and almost half the patients had been admitted two or more times for heart failure. The etiology of the heart failure (Table 2) was ischemic in 41% (1603) patients, hypertensive in 19% (744), idiopathic or alcoholic dilated cardiomyopathy in 17% (644), valvular in 17% (644), and other in 6% (including acute myocarditis, arrhythmias, congenital heart disease, restrictive , and hypertrophic cardiomyopathy, and other specific etiologies). An ischemic cause was significantly the most common etiology in men and hypertension in women, with few differences in the other causes (Table 2). Nine percent of the patients (352 cases) had important anemia, with hemoglobin levels below 10 g/dL, and 15% (586) had chronic renal failure (serum creatinine >1.5 mg/dL).
Characteristics of the Heart Failure at the Visit to the Heart Failure Unit Resulting in Inclusion in the Registry
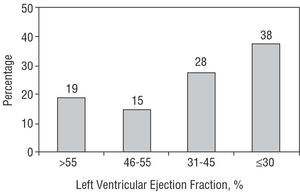
Approximately half the patients were in functional class I or II and the other half in class III or IV at the time of inclusion in the registry (Table 2). Significantly more women had a more advanced functional class, III or IV (Table 2). The cardiac rhythm on the electrocardiogram was predominantly sinus (65%, 2541 patients) in both men and women. The left ventricular ejection fraction (LVEF) was known (measured during the initial visit to the heart failure unit or during the previous 6 months) in 90% of the patients (3518 cases), with no differences between men and women (Table 3). The mean LVEF was 28±14%, 25±13% in the men and 41±14% in the women, P<.001. The distribution of the LVEF is shown in Figure 3: 66% of the patients (2322 cases) had a LVEF <45%, whereas the remaining 34% had heart failure with preserved systolic function, with LVEF >45%.
Figure 3. Distribution of the values of the left ventricular ejection fraction in our patients.
Tests Undertaken During the Initial Visit
Table 3 shows the tests undertaken during the initial visit or during the previous 6 months. Doppler echocardiogram was performed in 3205 (82%) patients, a radioisotope study in 547 (14%) patients, ergometry in 547 (14%) patients, Holter in (18%) 704 patients and cardiac and coronary catheterization in 1290 (33%) patients. Other tests, such as endomyocardial biopsy or electrophysiological studies, were very uncommon. The percentages of Doppler echocardiograms, radioisotope studies, and Holter tests were similar in men and women, whereas ergometry and cardiac catheterization were more common in men (Table 3).
Pharmacological Therapy
The pharmacological treatment recommended after the initial visit to the heart failure unit is shown in Table 4. Eighty-six percent of the patients took diuretics, 37% digoxin, 71% angiotensin-converting enzyme (ACE) inhibitors, 16% angiotensin II receptor antagonists (ARA-II), 32% spironolactone, 59% beta-blockers, 28% nitrates, 37% anticoagulation agents, 41% anti-platelet aggregating agents, and 31% statins (the absolute values are given in Table 4). Other drugs, such as antiarrhythmic agents and calcium antagonists, were much less commonly used. ACE inhibitors, beta-blockers, nitrates, anti-platelet aggregating agents and statins were used more by men than women, whereas no differences in use according to gender were seen with diuretics, digoxin, ARA-II, spironolactone, calcium antagonists, or anti-coagulating agents (Table 4). Table 4 also shows the drugs most used within the major groups of pharmacological agents; carvedilol was the most commonly prescribed drug among the beta-blockers, enalapril among the ACE inhibitors, losartan among the ARA-II, furosemide among the diuretics, aspirin among the anti-platelet aggregating agents, amiodarone among the anti-arrhythmic agents, and amlodipine among the calcium antagonists. Only very slight variation was seen during the follow-up in the percentages of the pharmacological agents used, and the pharmacological profile at the end of the observation period was similar to that shown in Table 4. The type of pharmacological agent used during the follow-up was only changed in 10% (390) of the patients. Table 5 shows the doses at the end of the follow-up period for the most commonly used drugs; no significant differences were seen between men and women in the doses used. The variation in pharmacological therapy between the different centers was small. The percentage prescription of diuretics ranged from 81%-93%, of digoxin from 33%-46%, of ACE inhibitors from 65%-81%, of ARA-II from 9%-21%, of beta-blockers from 50%-66%, and of spironolactone from 27%-38%.
Table 6 shows the pharmacological treatment received by the patients according to whether their LVEF was above or below 45%. As can be seen, the patients with a depressed ejection fraction, below 45%, received significantly more ACE inhibitors, beta-blockers, and spironolactone than the patients with preserved systolic function. These patients with preserved systolic function used more calcium antagonists, with no significant differences for the other drugs (Table 6).
Morbidity and Mortality During Follow-up
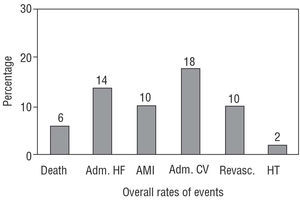
The overall rate of events, after a follow-up period of 13±4 months, is shown in Figure 4. The overall mortality rate was 6% (234 deaths); the cause of death was cardiovascular in 90% (211) of the patients and non-cardiovascular in the remaining 10% (23) of the patients. Among the cardiovascular deaths, this was due to progression of the heart failure in 59% (138) of the deaths, sudden death in 26% (61) and other causes in the remaining 5%. The overall rates of readmission for heart failure, acute myocardial infarction, other cardiovascular admissions, coronary revascularization or heart transplant were very low (Figure 4), and very similar between men and women. Regarding the functional class at the end of the follow-up period, only 23% (899) of the patients were in functional class III or IV (21% of the men and 28% of the women, P=NS).
Figura 4. Overall rates of mortality, admission for heart failure and other cardiovascular events in the whole group of patients (n=3909). Adm. HF indicates admission for heart failure; AMI, acute myocardial infarction; Adm. CV, admission for other cardiovascular reasons; Revasc., coronary revascularization; HT, heart transplant.
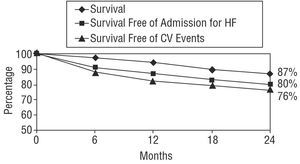
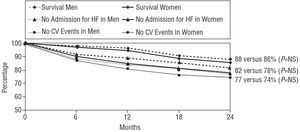
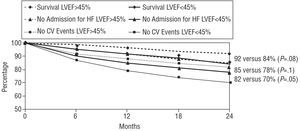
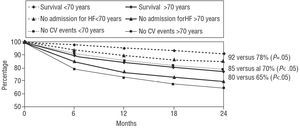
The actuarial probability of survival at 24 months was 87%, the probability of survival without admission for heart failure was 80%, and the probability of event-free survival was 76% (Figure 5). The probabilities of survival were similar for men and women, as can be seen in Figure 6. Regarding the systolic function, the patients with a LVEF above 45% had a non-significant trend towards a greater likelihood of overall survival and survival free of admission for heart failure at 2 years (Figure 7), whereas cardiovascular event-free survival was significantly higher in these patients compared to the patients with a depressed ejection fraction. Finally, as can be seen from Figure 8, the patients who were older than 70 years of age had a significantly lower likelihood of survival at 2 years compared with the younger patients.
Figure 5. Overall survival curve and curves for survival free of admission for heart failure (HF) and cardiovascular events (CV) (whole group, 3909 patients).
Fig. 6. Overall survival curve and curves for survival free of admission for heart failure (HF) and cardiovascular events (CV), according to sex. No significant differences were seen between men and women in the 3 survival curves.
Fig. 7. Two-year likelihood of survival, survival free of admission for heart failure (HF) and survival free of cardiovascular events (CV), according to whether the left ventricular ejection fraction (LVEF) was lower than or equal to or greater than 45%. Patients with an ejection fraction above 45% had a trend to better overall survival and survival free of admission for HF. Survival free of CV events was significantly greater in these patients, compared with the patients who had an ejection fraction below 45%.
Fig. 8. Two-year likelihood of survival, survival free of admission for heart failure (HF) and survival free of cardiovascular events (CV), according to whether the age was under or over 70 years. The older patients had less probability of actuarial survival.
DISCUSSION
This registry provides a true overall picture of the characteristics and management of heart failure in Spain, within a very well-defined context: patients managed and followed-up in specific heart failure units or clinics. Herein, however, lies its main limitation, as the results can not be extrapolated. The most important characteristics resulting from this registry concern the excellent adaptation of the pharmacological therapy given to that recommended in the heart failure guidelines15 and the low incidence of mortality and cardiovascular events during the follow-up, aspects which may be related not only with each other but also with other factors.
Pharmacological Therapy
Angiotensin-converting enzyme inhibitors were given to more than 70% of the patients, spironolactone to 32% and beta-blockers to almost 60%. These percentages were even higher in the patients with a depressed LVEF: 78% received ACE inhibitors (and 18% ARA-II), 37% received spironolactone, and 65% received beta-blockers (Table 6). The percentage use of ACE inhibitors and beta-blockers in the patients with a LVEF above 45% (55% and 48%, respectively) was significantly lower, but nevertheless still high, probably partly because of the ischemic or hypertensive etiology in many of these patients. In most single-center registries, both in Spain and in other countries,6-8 the percentage of patients treated with ACE inhibitors, and especially those treated with beta-blockers, is much lower, with recent studies showing the percentage use of beta-blockers to be just 5%.6 In the recently published EuroHeart Failure Survey,16 the percentage of patients who received ACE inhibitors or ARA-II was 66% (87% in our registry) and the percentage of patients on beta-blockers was 37% (59% in our study). Some studies in very specialized centers and in a select population of patients have indeed managed to achieve optimal therapy,17 but the study reported herein shows that achieving adequate therapy, similar to that seen in clinical trials,2-5 is possible in a large number of centers and units with a very variable organization and structure. In fact, no significant differences were detected in the pharmacological treatment provided by the different participating centers, be they general or community hospitals, as shown by the low variability between centers in the percentage of patients treated with the different drugs. No important differences seen in the treatment of the various subgroups of patients (men and women, LVEF below or above 45%), except those due to the particular characteristics of each group: a greater use of beta-blockers, anti-platelet aggregating agents and nitrates in men (probably related with the greater prevalence of ischemic heart disease) (Table 4), and greater use of ACE inhibitors, beta-blockers and spironolactone in those patients with a depressed LVEF, which is in agreement with the available evidence15 (Table 4).
Morbidity and Mortality
Another interesting aspect highlighted by the registry is the low rate of mortality and admission due to heart failure. Although the follow-up period was short, a likelihood of 2-year survival of 87% and a likelihood of admission-free survival of 80% are better than those seen in the main clinical trials on heart failure, even the most recent,2-5 and are much better than those of hospital or population registries.6-9,16 For instance, Permanyer-Miralda et al6 reported a mortality rate of 46% at 18 months in a population of patients admitted for heart failure in 1998. Varela-Román et al9 found a 1-year mortality of 20% in a series of 229 patients admitted in their center due to heart failure.9 Jong et al,8 in a study undertaken in 38 702 patients admitted for the first time with heart failure in Ontario, Canada, reported a 1-year mortality above 30% and a rate of mortality or readmission due to heart failure of around 55% at 1 year. However, the characteristics of these patients differed to those of our patients, since their patients were older (around 75 years of age in the studies of Permanyer-Miralda et al and Jong et al, compared with 66 years of age in our series, which was similar to the 66.7 years in the study by Varela-Román et al). Furthermore, coexisting conditions, which were not studied in our registry, were probably greater in the other registries. Thus, we cannot rule out the possibility of a selection bias due to the characteristics of our registry and the criteria for inclusion of the patients in the heart failure clinics, which resulted in the patients having a lower risk.
Randomized studies which have compared the care provided by heart failure units with that afforded by the usual setting have shown a very significant reduction in admissions for heart failure.11,12 Two randomized studies have recently been published which also showed a significant reduction in mortality,18,19 one of them a multicenter study in Spain.19 The Swedish study, with heart failure units based on specialized nursing care, reduced 1-year mortality from 37% in the group receiving the usual care to 13% in the group managed in the heart failure unit (P=.005).18 The 1-year survival of this series was 87%, slightly lower than that of the BADAPIC Registry (94% at 1 year and 87% at 2 years), although the mean age of the patients in the Swedish study was much higher, 77 years. The methodology of the Spanish multicenter study, PRICE,19 was more similar to that of the BADAPIC registry, with heart failure units based on cardiologists, and a mean patient age of 69 years. Survival in the patients managed by heart failure units in the PRICE study was 90% at 1 year and 83% at 2 years, figures which are slightly lower than those of the BADAPIC registry. However, the PRICE study only included patients with heart failure who were discharged from hospital and who therefore have a worse prognosis than the patients in the BADAPIC registry, almost half of whom were outpatients with no recent admission. Despite these small differences between the 2 studies of randomized intervention and the observational BADAPIC study, the annual rates of mortality are between 5%-10% in all 3 studies, much lower than the annual mortality rates of 20%-30% in the previously mentioned population registries,6-9,16 and similar to those of clinical trials.2-5 Care of patients with heart failure in specialized clinics or units therefore seems to improve the prognosis of these patients.
IMPLICATIONS AND LIMITATIONS
Firstly, the results indicate that production in Spain of a registry dealing with such a common and widespread problem as heart failure, with the participation of numerous centers, is feasible. The findings reported suggest that the diagnostic standards and recommended treatments can be achieved in patients with heart failure by means of the use of specific heart failure units or clinics. This observation does not imply that all patients with heart failure should be seen in this type of center. Collaboration should be encouraged among the different levels of care (specialized units, general clinics, primary care), with the participation of different personnel, including physicians and nursing staff.20 This collaboration would result in better care for many patients with heart failure, which should be our ultimate aim. The main limitation of this registry, its observational and non-controlled character, introduces a possible selection bias when evaluating the results concerning the low rates of mortality and morbidity. Nevertheless, the results of randomized interventional studies with specific heart failure clinics support the idea that this type of care can improve the prognosis for patients with heart failure.
ACKNOWLEDGEMENTS
The Working Group on Heart Failure, Heart Transplantation and Other Therapeutic Alternatives wishes to thank Dr Eduardo de Teresa Galván, president of the Working Group on Heart Failure of the Spanish Society of Cardiology at the time of the inception and establishment of the registry project, for his inestimable collaboration and help in the design of the project and the elaboration of the database. The Group also acknowledges Roche Pharma, and especially Isidro Lázaro and María José Ramírez, for their contribution, help and constant dedication to this project. Finally, we also wish to thank the true protagonists and authors of this registry, all the main researchers, for their collaboration and without whose daily work and effort this registry would not have been possible.
*The researchers and hospitals participating in the BADAPIC Registry are shown in the Annex.
Correspondence: Dr. M. Anguita Sánchez.
Damasco, 2, 2.o 9. 14004 Córdoba. España.
E-mail: manuelp.anguita.sspa@juntadeandalucia.es