Keywords
INTRODUCTION
Despite major advances in cardiac imaging, electrocardiography (ECG) is still the most accessible and cheapest means to assess patients with symptoms of acute myocardial ischemia. The ECG findings form an essential part of the decision-making process, particularly in relation to reperfusion therapy. In acute coronary syndrome (ACS), the number of electrocardiographic leads with ST-segment deviation (either elevation or depression) is a marker of the extent of ischema.1 Acute obstruction of the left main coronary artery (LMCA) causes severe hemodynamic deterioration and often leads to the death of the patient.2 Predicting acute obstruction of the LMCA is essential for prognosis and for choosing the appropriate therapeutic strategy.
Different studies have been done to assess the usefulness of ECG and validated diagnostic criteria have been established, such as ST-elevation in lead aVR3-5 and extensive endocardial injury.3,4 Yamaji et al5 compared the ECG findings for LMCA, left anterior descending artery (LAD), and right coronary artery (RCA) obstruction. The authors concluded that greater ST-elevation in lead aVR than in lead V1 predicts LMCA obstruction. However, it has been pointed out that the study did not include patients with obstruction of the circumflex artery (CxA) or 3-vessel disease.6,7
In ACS, it is relatively common to observe changes in the ECG that are compatible with LMCA disease but that are subsequently not confirmed by angiography. In view of these observations and with the aim of investigating new criteria for predicting LMCA obstruction, we conducted a study of 57 consecutive patients with ECG findings indicative of LMCA disease. The value of ST-segment and QRS vector analysis for predicting LMCA obstruction was assessed.
METHODS
Patients
Between April 2004 and January 2006, 840 patients were admitted to our department with ACS. In 51% (427 patients), a coronary angiogram was performed during their stay in hospital. Retrospectively, 57 of these patients who had ECG findings suggestive of LMCA disease were included. The characteristic findings in the ECG were ST-elevation in lead aVR3-5 and ST-depression in at least 6 leads.3,4 Patients with a history of myocardial infarction, valve disease, cardiomyopathy, or left bundle branch block were excluded.
Diagnosis of acute myocardial infarction was established by chest pain, ECG changes, and serum enzymes. The clinical and angiographic characteristics of the patients with LMCA disease are summarized in Table 1.
Electrocardiography
The 12-lead ECGs were recorded on admission prior to any therapeutic intervention. ST changes and the ST and QRS vectors in the frontal plane were analyzed. The Bailey 6-axis system was divided into 4 quadrants (Figure 1), and patients were included in each quadrant in accordance with the vector analysis of the ST segment and QRS complex.
Figure 1. Six-axis system divided into quadrants A, B, C, and D.
Given that electrical activity is 3-dimensional, a vector analysis of the ST-segment was also done in the horizontal plane. The precordial lead in the transitional zone where the ST segment remained isoelectric was identified, and the ST vector was located perpendicular to this zone.8 When the transitional zone was between lead V1 and V2, the horizontal ST vector was located parallel to the frontal plane.
The ST-segment deviations were assessed at 60 ms from the junction of the QRS complex. A change in the QRS axis between 1º and 90º (quadrant B) was considered as a left shift. Anterior hemiblock was diagnosed in accordance with the criteria of Rosembaum.9
Coronary Angiography
Coronary angiography was performed in all patients; the procedure was done within 24 hours in 50 patients and in the first 3 days for the remaining 7. Significant coronary stenosis was classed as a decrease in luminal diameter of 75% or more. The lesion was defined as causal when it was completely occlusive or showed severe stenosis with evidence of local dissection, residual thrombus, or ulcerated plaque. The lesion was assessed by 2 cardiologists who were unaware of the electrocardiographic findings. Collateral circulation was assessed according to the classification of Rentrop et al.10
Patients were divided into 2 groups: group 1 included 20 patients with severe LMCA lesion and group 2 included 37 patients without LMCA disease. The electrocardiographic findings for the 2 groups were compared.
Statistical Analysis
Data were analyzed with the SPSS software package, version 13.0 (SPSS Inc., Chicago, Illinois, USA). The continuous variables were expressed as mean (SD). Changes in ECG for the 2 groups were compared using the χ2 test or the Fisher exact test if necessary. Relative risks, sensitivity, specificity, and positive and negative predictive values were calculated for each categoric variable diagnostic of LMCA obstruction. The continuous variables were analyzed using the area under the receiver operating characteristics (ROC) curves. The ECG variables independently associated with LMCA lesion were assessed by stepwise logistic regression analysis.
The area under the ROC curve of the logistic regression model was calculated. For all estimates, 95% confidence intervals were calculated. A P value less than .05 was considered significant.
RESULTS
Coronary Angiography
Patients were divided into 2 groups: group 1 included 20 patients with severe LMCA lesions (12 men and 8 women; age 64 [14] years, range 34-85 years). Group 2 included 37 patients with severe LMCA lesions (26 men and 11 women; age, 65 [12] years; range, 35-88 years), with no LMCA lesion (19 with CxA lesion, 10 with LAD lesion, 5 with RCA lesion, and 3 with 3-vessel disease).
ST-Segment Changes
ST depression in leads II, III, and aVF was observed in 100% (20/20), 60% (12/20), and 95% (19/20), respectively, of the patients with LMCA lesion (group 1) and in 51% (19/37), 35% (13/37), and 49% (18/37), respectively, of patients with no LMCA lesion (group 2) (P<.001; P=.009; and P<.001, respectively). ST elevation >2 mm in lead aVR was observed only in patients with LMCA lesion (sensitivity, 30%). ST-elevation or isoelectric findings were observed in leads V1 and V2 in 100% and 75% of the patients in group 1, respectively, compared to 60% and 14% of those in group 2 (P=.001 and P<.001, respectively); 3 patients with LMCA obstruction showed more significant changes in lead II with an ST depression of 4 mm.
ST-Segment Vector
The values for sensitivity, specificity, and predictive values are shown in Table 2. An ST vector directed towards quadrant A in the frontal plane was observed in 100% (20/20) of the patients with LMCA disease and in 21.6% (8/37) of those without LMCA disease (P<.001). In the horizontal plane, the horizontal or parallel ST vector was observed in 95% (19/20) of the patients in group 1 and 8% (3/37) of those in group 2 (P<.001).
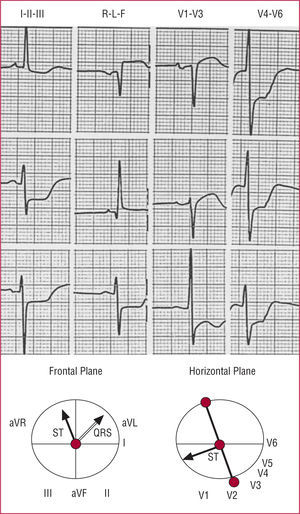
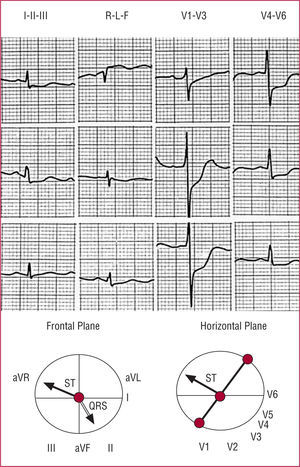
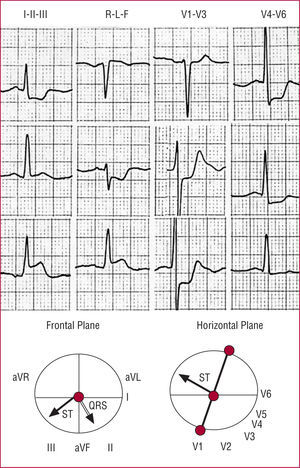
An ST vector directed towards quadrant A and in an anterior and parallel direction in the horizontal plane was observed in 95% (19/20) of the patients of group 1 (Figure 2), but in none (0/8) of those in group 2 (P<.001) (Figure 3). This finding allowed us to distinguish between patients with LMCA disease and those without, with a specificity of 100%; 7 of the 8 patients with ST vector directed towards quadrant A and with posterior direction had CxA obstruction (Figure 3); the other patient had 3-vessel disease with 100% CxA obstruction. None of the patients in group 1 had an ST vector in quadrants B, C, or D, compared with 78.4% (29/37) of the group 2 (P<.001) (quadrant B, n=9; quadrant D, n=20) (Figures 3 and 4).
Figure 2. Characteristic electrocardiogram of a patient with left main coronary artery obstruction. The ST vector is located in quadrant A (-100º) in the frontal plane and is anterior in the horizontal plane. QRS vector with anterior hemiblock (-45º).
Figure 3. Electrocardiogram of a patient with circumflex artery obstruction. The ST vector is directed towards quadrant A (150º) in the frontal plane but is posterior in the horizontal plane. QRS Vector = +70°.
Figure 4.Electrocardiogram of a patient with right coronary artery obstruction. The ST vector is directed towards quadrant D (+150º) in the frontal plane and is posterior in the horizontal plane. QRS Vector = +65°.
QRS-Complex Vector
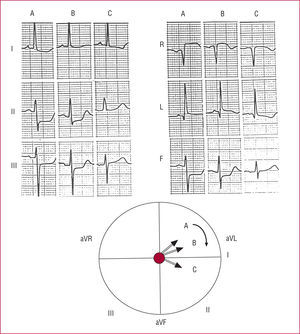
The values for sensitivity, specificity, and predictive values are shown in Table 2. The left-shifted QRS vector (quadrant B) was observed in 90% (18/20) of the patients with LMCA lesion (between 10º and 65º) and in 29.7% (11/37) of those without LMCA disease (between 10º and 70º) (P<.01). Left shift ≥-30º of the QRS vector, with anterior hemiblock, was found in 75% (15/20) of the patients of group 1 (Figure 3) and 5.4% (2/37) of those of group 2 (both with LAD lesions) (P<.001). Transient left shift of the QRS vector was observed in 62.3% (9/13) of the patients with LMCA lesions who survived the acute episode, coinciding with the ischemic changes in the ECG. Figure 5 shows the changes in the QRS vector in a patient with LMCA obstruction. An ST vector with no left shift was found in only 10% (2/20) of the patients in group 1, compared to 70.3% (26/37) of the patients of group 2 (P<.001) (Figures 3 and 4).
Figure 5. Changes in the QRS vector of the patient of Figure 3. A (acute phase): left shift of the QRS vector (45º). B and C (after revascularization and resolution of the ischemia): progressive decrease in left shift with the QRS vector directed towards 15º and +5º, respectively.
ST Vector and QRS-Complex Vector
The values for sensitivity, specificity, and predictive values are shown in Table 2. An ST vector directed towards quadrant B with left shift of the QRS vector was observed in 90% (18/20) of the patients in group 1 compared to 8.1% (3/37) of those in group 2 (P<.001). An ST vector directed towards quadrant A with left shift of the QRS vector≥-30º and anterior hemiblock was observed in 75% (15/20) of the patients in group 1 and in none of the patients in group 2 (P<.001). This finding was a specific diagnostic marker of LMCA obstruction (Figure 2).
Multivariate Analysis
The variables that best classified the patients with and without LMCA disease were left shift of the QRS vector by ≥-30º and an anterior or parallel ST vector in the horizontal plane (Table 3).
Algorithm
An algorithm was drawn up by integrating the ECG data. The findings of the vector analysis of the ST segment and the QRS complex allowed the LMCA obstruction to be identified in 100% of the patients. Figure 6 summarizes the diagnostic steps.
Figure 6. Algorithm for diagnosis of left main coronary artery (LMCA) obstruction. Vector analysis of the ST segment in the frontal plane (vector directed between 90º and 180º) and the horizontal plane (anterior or parallel direction), and analysis of the QRS vector (anterior hemiblock). Diagnosis of the LMCA obstruction can be established in all patients. Two different paths can be followed, depending on whether or not anterior hemiblock is present. LMCAdis indicates left main coronary artery disease.
DISCUSSION
In patients with ACS, it is essential to identify LMCA obstruction as early as possible to allow appropriate therapy to be applied.
This study was conducted to assess the value of ECG vector analysis in the diagnosis of LMCA obstruction. The identification of new electrocardiographic criteria for predicting LMCA disease could contribute to a more accurate prognoses.
Validated electrocardiographic criteria have been established, such as extensive subendocardial lesion3,4,6 for diagnosis of LMCA disease. Yamaji et al5 concluded that greater ST elevation in lead aVR than in lead V1 had a sensitivity of 81% and a specificity of 80% for diagnosis of LMCA disease: however, as has been pointed out, the study did not include patients with CxA disease or 3-vessel disease.6,7
As far as we are aware, this is the first study based on the concept of spatial vector electrocardiography proposed by Grant,11 who used vector analysis of the ST segment and QRS complex for diagnosis of LMCA obstruction.
ST Vector and ST Elevation in Lead aVR
Subendocardial lesion resulting from LMCA obstruction induces an extensive current, represented by the ST vector, which is directed away from the area of the subendocardiac lesion.8 In our study, the ST vector shifted upwards and to the right, between 90º and 180º (that is, towards quadrant A) in all patients with LCMA obstruction. The result is ST elevation in lead aVR and ST depression in lead II. Therefore, LCMA obstruction is ruled out by an ST vector outside quadrant A. In the horizontal plane, the ST vector was anterior or parallel in 95% (19/20) of the patients with LMCA obstruction, with an anterior angle always less than or equal to 30º. This leads to ST elevation in lead aVR and ST depression in lead V2-V3 through lead V6.
Eight patients with no LMCA involvement also had an ST vector in quadrant A, and the CxA obstruction was the cause in all cases. Unlike obstruction of the LMCA, CxA obstruction always gives rise to an ST vector in a posterior direction, thereby distinguishing CxA obstruction from LMCA obstruction.
All patients in group 2 with CxA obstruction and ST elevation in lead aVR had a posterior ST vector in the horizontal plane and none of the patients had ST elevation in lead V1. In accordance with these findings, ST elevation in lead aVR in patients with CxA obstruction can be attributed to severe transmural ischemia at the posterior basal segment, as described by Gorgels et al,6 who reported an upwards shift in the ST vector in the frontal plane and a posterior shift in the horizontal plane.
ST elevation in lead aVR in patients with proximal LAD obstruction and LMCA obstruction has been attributed to transmural ischemia of the basal segment of the ventricular septum due to occlusion of the first septal branch of the LAD.5,12 The muscular predominance in this basal part of the septum would lead to an upwards shift in the ST vector in the frontal plane and ST elevation in leads aVR and aVL and ST depression in the lower leads.13
In the study by Yamiji et al,5 greater ST elevation in lead aVR than in lead VI would distinguish between patients in the LMCA group and those in the LAD group. We also found greater ST elevation in lead aVR than in lead V1, but we could not validate this finding as only 3 patients in group 2 had LAD obstruction. In LMCA obstruction, posterior ischemia associated with CxA disease counteracts the anterior ischemic forces secondary to LAD. This leads to ST depression in lead V1, as has already been mentioned.5 To explain ST elevation in lead aVR in patients with RCA obstruction, septal branches of the RCA have been proposed as the cause of the ischemia.5
Generalized subendocardial lesion is normally observed in cases of 3-vessel disease, LMCA obstruction, and in other pathologic conditions.8 ST elevation in lead aVR has been observed in 3-vessel disease,4 LAD disease,12,14-16 and RCA obstruction.5 So far, no prior study has reported ST elevation in CxA obstruction.
This study shows that ST elevation in lead aVR in association with extensive ST depression can be observed in patients with LMCA disease, 3-vessel disease, and isolated disease of the LAD, RCA, and CxA. In fact, in our study, CxA obstruction was the most frequent type of obstruction in group 2, with 51.3% (19/37) of the patients affected.
This study also showed that, in LMCA obstruction, diffuse endocardial lesion generates an ST vector pointing upwards and to the right (between 90º and 180º) and an anterior or parallel vector in the horizontal plane. Of all the other coronary arteries, only CxA obstruction can have an ST vector in quadrant A, but unlike LMCA disease, the ST vector with CxA obstruction is always posterior in the horizontal plane.
QRS-Complex Vector
Left shift of the QRS vector by 30º or more with anterior hemiblock was a highly significant variable for predicting LMCA obstruction, with a sensitivity of 75%. When combined with an ST vector in quadrant A, the specificity was as high as 100%. It is possible that some of the patients already had prior hemiblock: however, the prevalence of anterior hemiblock was significantly higher in group 1 than in group 2 (75% and 5.4%, respectively, all with LAD disease). On the other hand, it was observed that anterior hemiblock was often transient and disappeared with resolution of the ischemia (Figure 5). It is somewhat surprising that such a finding has not been mentioned in previous studies of LMCA lesion.
Transient left shift of the QRS vector has been observed during exercise testing in patients with LAD disease.18-20 In the study by Kodama et al,20 24% of the patients with proximal LAD lesion showed a transient left shift of the QRS vector and only 10% (3/29) showed leftward axis shift with anterior hemiblock. This leftwards shift of the QRS vector without evidence of anterior hemiblock ("incomplete" anterior hemiblock) may reflect a progressive conduction defect of the anterior branches of the left bundle given their fan distribution.21 Those authors concluded that transient leftwards shifts of the QRS axis during exercise testing are very indicative of proximal lesion in LAD disease.
In our study, 90% of the patients with LMCA obstruction had a leftwards QRS axis shift, and 75% (17/20) met the criteria for anterior hemiblock. Such a high prevalence is probably due to the severity of the ischemia associated with ACS, with acute necrosis in many patients. Transient conduction defects during exercise testing have been associated with frequency-dependent conduction disturbances,18 especially with myocardial ischemia.18-20 In our study, a transient leftwards shift of the QRS vector was not associated with increased heart rate; it was always associated with ischemic changes in the ECG and the largest leftwards axis shift was found during the acute phase. The magnitude of the shift decreased as the ischemia improved (Figure 5).
Therefore, severe ischemia of the conduction system affecting the anterosuperior left bundle branch seems to be the most reasonable mechanism. The so-called preinfarction block might also play a role. This would affect the delay in activation and conduction of the anterosuperior ischemic areas, and so the terminal forces would act towards the ischemic zone.22
Limitations
The number of patients in our study was small in view of the relatively low prevalence of acute obstructions of the LMCA in patients who are admitted to hospital. The study was retrospective and our findings should be confirmed with a prospective design. The ECGs showing the most pronounced changes during ischemia were chosen. Therefore, our findings might not be reproducible in a situation in which ECG examinations are not often performed. Only patients with ST elevation in lead aVR and ST depression in 6 or more leads were selected, and so the findings of the study are applicable only to this ECG pattern. On the other hand, although it might be that some LMCA obstructions were not detected, this seems unlikely as we did not find any other patient with LMCA obstruction in our hospital records during this period. It was not possible to compare data for patients with LMCA obstruction with those with LAD obstruction, as only 3 patients had an obstructed LAD. Patients with LAD obstruction have ST elevation in precordial leads and rarely (only 3 cases in our series) ST depression in 6 or more leads. On the other hand, the ECG characteristics in LAD obstruction at different levels have been well described and usually do not cause any diagnostic problems.12,14,23 The ST vector is not usually directed towards quadrant A.
CONCLUSIONS
In patients with ACS and diffuse ST depression, vector analysis of the ST segment and QRS complex distinguishes between LMCA obstruction and other coronary lesions. The use of a diagnostic algorithm based on analysis of the ST vector in the frontal plane (vector of 90º to 180º) and in the horizontal plane (anterior or parallel direction) and of the QRS vector (left shift with anterior hemiblock) allows diagnosis of the LMCA obstruction. The possibility of establishing early diagnosis of LMCA obstruction, differentiating this condition from other coronary artery disease is very relevant to clinical practice.
ACKNOWLEDGMENTS
We thank Dr Marta Pulido for her editorial assistance.
ABBREVIATIONS
ACS: acute coronary syndrome
CxA: circumflex artery
LAD: left anterior descending artery
LMCA: left main coronary artery
RCA: right coronary artery
Correspondence: Dr. J.A. Prieto-Solís.
Unidad Coronaria. Hospital Universitario Marqués de Valdecilla.
Avda. de Valdecilla, s/n. 39008 Santander. Cantabria. España.
E-mail: ucopsj@humv.es
Manuscript received April 18, 2007.
Accepted for publication September 24, 2007.