Patients with heart failure and similar left ventricular systolic dysfunction have differing exercise capacity. The aim of this study was to identify echocardiographic predictors of exercise capacity in patients with heart failure and systolic dysfunction.
MethodsWe included 150 patients with class II (70%) or III (30%) heart failure with left ventricular ejection fraction below 40%. Six-minute walking test and cardiac color Doppler-echo, including tissue Doppler of mitral and tricuspid rings, were performed. Moderate and severe mitral regurgitation were considered as significant. Two groups were divided according to the median walking distance (290 m): Group 1, < 290 m and Group 2, ≥290 m.
ResultsMitral regurgitation was detected in 112 patients (75%), which was significant in 40 (27%). Group 1 showed more significant mitral regurgitation (35 vs 18%), increased left atrium area (27±1 vs 24±1cm2), mitral E amplitude (88±5 vs 72±3cm/s) and systolic pulmonary pressure (37±1 vs 32±1mmHg, all P<.05). By logistic regression analysis, only the presence of significant mitral regurgitation was independently associated with less walked distance (odds ratio: 3.44 95% confidence interval 1.02-11.66, P<.05). By multiple linear regression, the only independent predictor of walked distance was left atrium area (r=0.25, beta coefficient: −6.52±2, P<.01).
ConclusionsIn patients with class II-III heart failure and left ventricular systolic dysfunction, the main echocardiographic predictors of exercise capacity are related to the presence of significant mitral regurgitation.
Keywords
.
INTRODUCTIONA common challenge in cardiology is: “How can a patient with low ejection fraction (EF) of the left ventricle can exercise without symptoms, while another with equal or better EF is severely symptomatic and unable to even lower activity?” For years, cardiologists have tried to solve this puzzle.1, 2 Several explanations have been offered, such as the preserved diastolic function, adequate peripheral vasodilatory capacity, or right ventricular function.3, 4.
Recently, the presence of mitral regurgitation (MR) has been described as an important factor, associated with reduced tolerance, in exercise capacity in heart failure.5, 6.
In addition to the direct measurement of oxygen (O2) consumption, a technically demanding and expensive study,7 to assess exercise tolerance in heart failure, the 6-minute walking test has become popular in recent years. This test is simple, cheap, reliable, repeatable, and can be performed in almost all patients.8, 9.
The aim of this study was to identify echocardiographic variables associated with a low distance walked in the 6-minute walking test in patients with heart failure and systolic dysfunction.
METHODSWe selected 151 patients with clinically stable chronic heart failure within the last 3 months and systolic dysfunction, defined as EF≤40%, from the MIMICA study (designed to evaluate the relationship of inflammation and metabolic parameters with EF and functional capacity in heart failure, results previously published).10 All patients had an available medical record, physical examination, ECG, biochemistry tests, bioelectrical impedance test to determine body composition, color Doppler echocardiogram, and 6-minute walking test. This analysis explores the relationship of echocardiographic parameters with exercise capacity in 150 patients (1 patient was excluded due to a poor acoustic window).
Echocardiographic ProtocolIn all patients, transthoracic cardiac color Doppler studies were performed by the same 2 trained operators (RG and MT) using Philips I-33 equipment with 2nd harmonic imaging and tissue Doppler. We excluded patients with inadequate chest, aortic valve disease, or significant arrhythmia. We measured left ventricle EF with biplane Simpson method and tissue Doppler was recorded at the mitral and tricuspid rings, measuring the peak systolic velocity (second systolic peak or S2), early diastolic (E’) and late (A’), electromechanical delay in each segment (from the Q wave to the onset of S) and pre-ejection period of both ventricles (Q wave to onset of ejection in aortic and pulmonary pulsed Doppler).
To estimate the severity of MR qualitative and quantitative parameters were used, according to the guidelines of the American Society of Echocardiography.11 Significant MR included moderate and severe degrees.
6-Minute Walking TestThe test was performed within 7 days. Two trained operators (JM and AA) measured distance walked in 6min. According to the median distance walked, 2 groups were defined: Group 1, < 290 m and Group 2, ≥290 m.
Statistical AnalysisContinuous variables were expressed as mean ± standard error and they were analyzed by t-test (normal distribution). Categorical variables are shown as percentages and they were analysed by chi-square test. To predict low or high distance walked, a logistic regression model was fitted with variables that achieved P<.10. P values were considered as significant at P<.05.
Multiple linear regression was also assessed by the association of baseline echocardiographic variables with the distance walked in meters, expressed as a continuous variable. Statistical analysis was performed using STATA 10.
RESULTSMR was detected in 112 patients (75%): mild in 72 (48%), moderate in 30 (20%), and severe in 10 (7%). Mean walked distance was 290±138 m.
Baseline characteristics of the patients are presented in Table 1. They were predominantly middle-aged men with good functional class. Mean ejection fraction was low. A high percentage was treated with beta blockers, renin-angiotensin system blockers and diuretics.
Table 1. Baseline Characteristics of the Patients.
| Variable | Value |
| Age (years) | 63±11 |
| Men (%) | 84 |
| Coronary etiology (%) | 53 |
| Functional class I-II | 71 |
| Blood pressure (%) | 53 |
| Diabetes mellitus (%) | 25 |
| Atrial fibrillation (%) | 15 |
| Heart beat (beats/min) | 72±13 |
| Systolic blood pressure (mmHg) | 111±19 |
| Ejection fraction | 28±7 |
| 6-minute walking test (m) | 290±137 |
| Creatinine clearance (ml/min) | 58±18 |
| NT-proBNP (pg/ml) * | 1000 (468-2005) |
| Beta-blockers (%) | 91 |
| Angiotensin antagonists (%) | 80 |
| Diuretics (%) | 79 |
* Median and [interquartile range] due to asymmetric distribution.
Table 2 shows echocardiographic variables in Groups 1 and 2. Cavity diameters were similar, but left atrial area was greater (27±1cm2 vs 24±1cm2, P<.05) and EF was lower (27±1% vs 29±1%, P=.05) in Group 1. Ventricular volumes tended to be higher among those who walked less, without reaching statistical significance.
Table 2. Echocardiographic Variables and 6-Minute Walking Distance.
| Variable | Group 1 (n=76) | Group 2 (n=74) | P |
| LVDD (mm) | 65±1 | 63±1 | .40 |
| LVSD (mm) | 53±2 | 53±2 | .90 |
| LAD (mm) | 44±1 | 44±1 | .55 |
| LAA (cm2) | 24±1 | 27±1 | .05 |
| EDV (ml) | 181±9 | 192±8 | .36 |
| ESV (ml) | 133±8 | 142±7 | .35 |
| LVEF (%) | 29±1 | 27±1 | .05 |
| Moderate-severe MR | 18.4% | 35.1% | .02 |
EDV, end-diastolic volume; ESV, end-systolic volume; LAA, left atrial area; LAD, left atrial antero-posterior diameter; LVDD, left ventricular diastolic diameter; LVEF, left ventricular ejection fraction; LVSD, left ventricular systolic diameter; MR, mitral regurgitation.
Table 3 shows the results of Doppler echocardiography in both groups. Patients who walked less had higher systolic pulmonary pressure and rapid filling velocity of anterograde mitral flow. No differences were observed in E/A or E/E’ ratios.
Table 3. Relationship Between Doppler Echocardiography Variables and 6-Minute Walking Distance.
| Variable | Group 1 (n=76) | Group 2 (n=74) | P |
| SPP (mmHg) | 32±1 | 37±1 | .01 |
| Mitral E (cm/s) | 72±3 | 88±5 | .01 |
| Mitral A (cm/s) | 63±4 | 64±4 | .88 |
| E/A ratio | 1.8±0.2 | 2.1±0.3 | .42 |
| DT | 187±10 | 174±1 | .40 |
| peP | 138±10 | 128±7 | .40 |
| E/E’ ratio | 12±1 | 14±1 | .22 |
DT, mitral E wave deceleration time; peP, pre-ejection period; SPP, systolic pulmonary pressure.
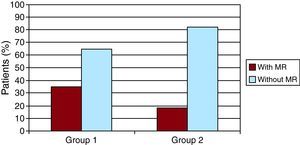
Figure 1 graphs the distance walked in the presence of significant MR. The percentage of patients with MR is twice as high among those with less distance walked (18% vs 36%, χ2=5.4, P=.02).
Figure 1. Relationship between significant mitral regurgitation and 6-minute walking distance. MR, mitral regurgitation.
In the logistic regression analysis, only the presence of significant MR was independently associated with less distance walked (odds ratio [OR]: 3.44 95% confidence interval [CI] 1.02-11.66, P<.05) (Table 4). In multiple linear regressions, the only independent predictor of distance walked was left atrial area (r=0.25, beta coefficient: −6.52±2, P<.01) (Table 5).
Table 4. Multiple Logistic Regression: Predictors of Reduced 6-Minute Walking Distance.
| Variable | OR | CI 95% | P |
| Moderate-severe MR | 3.44 | 1.02-11.66 | <.05 |
| LA area | 1.06 | 0.97-1.16 | NS |
| SPP | 1.03 | 1.00-1.06 | NS |
| E/E’ ratio | 1.01 | 0.96-1.06 | NS |
CI, confidence interval; LA, left atrium; MR, mitral regurgitation; NS, no significant; OR, odds ratio; SPP, systolic pulmonary pressure.
Table 5. Multiple Linear Regression: Predictors of 6-Minute Walking Distance.
| Variable | Beta coefficient | CI 95% | P |
| LA area | −6.45 | −10.82 to −2.07 | <.05 |
| SPP | −1.84 | −4.20 to 0.51 | NS |
| E/E’ ratio | −2.11 | −5.07 to 0.84 | NS |
CI, confidence interval; LA, left atrium; NS, no significant; SPP, systolic pulmonary pressure.
Finally, the presence of significant MR was the only independent echocardiographic predictor of mortality at 2 years (hazard ratio 6.46, 95% CI 2.3-18.1, P<.01) in this series.
DISCUSSIONThe different functional capacity in patients with heart failure and similar chronic ventricular dysfunction is a long-standing dilemma in clinical cardiology.12, 13 The results of this study suggest that the presence of significant MR could play a leading role in this scenario: it was the only independent echocardiographic predictor of low distance walked. In our view, the association between a reduction in the distance walked in the 6minutes test and the presence of significant MR is a novel finding of this study.For a long time, the presence of MR was considered an epiphenomenon of dilated cardiomyopathy. In recent years we have learned that it is not always the case. While most patients with dilated cardiomyopathy have some degree of MR, moderate to severe degrees are not as frequent.14 Incidence of functional MR is increasing, in parallel with growing coronary artery disease worldwide.15 The presence of moderate to severe MR adds an unfavorable prognostic factor in these patients.16, 17 Some of them seem to benefit from surgical correction.18, 19 The noncorrection of MR in patients undergoing coronary artery bypass surgery seems to overshadow the long-term prognosis.20, 21, 22, 23.
Corroborating these data, in the present study significant MR was the only independent echocardiographic mortality predictor at 2 years.
It is known that the presence of MR in ergometer tests can reduce maximal O2 consumption in cardiopulmonary exercise testing.6 Beyond the controversy of which is better,24 both the measurement of O2 consumption treadmill test and 6-minute walking test are commonly used to assess functional capacity in heart failure patients.
Given the plethora of literature on the benefits of tissue Doppler, especially the E/E’ ratio, to predict functional capacity,25, 26, 27 it is a little surprising that in this case there are significant differences, even in bivariate analysis. There were no differences between more and less walked distance in other tissue Doppler parameters and measured periods (pre-ejection of both ventricles and electromechanical delay).
Consistent with these findings, other variables with significant differences were associated with the presence of MR, such as left atrial area, mitral E-wave and systolic pulmonary pressure. The only exception was the EF, with borderline significance.
The left atrial area deserves a separate paragraph. It was the only significant independent variable in multiple linear regression analysis. In other words, it was the best quantitative variable associated with the distance walked in meters.
The left atrial area seems to better estimate atrial size than the antero-posterior diameter, and volume is probably even better than the area, as has been proposed. Why is atrial size related to exercise capacity? In addition to MR, other factors must influence this relationship. Thus, it has been reported that left atrial function is a predictor of exercise capacity in patients without contractile dysfunction.28 Atrial peptides related to compliance and atrial pressure appear to play a role in this regard.29, 30.
Several limitations can be noted in this study. MR was not quantified systematically. However, we wanted to respect the qualitative and quantitative method that is commonly used in clinical practice. While significant, the logistic regression CI for the MR is wide. However, the predictive power of the distance walked was very consistent as an independent variable in several models tested.
We did not perform direct measurements of O2 consumption or calculate left atrial volume: both would seem to be important for future research.
CONCLUSIONSIn patients with heart failure and systolic dysfunction, the detection of significant MR was associated with lower walked distance in the 6-minute walking test. Other variables related to MR, such as left atrial area, E wave amplitude of mitral inflow, and pulmonary systolic pressure, were the only echocardiographic predictor of walked distance. MR can be a determinant of functional capacity in patients with heart failure and systolic dysfunction.
CONFLICTS OF INTERESTNone declared.
Received 9 March 2011
Accepted 4 June 2011
Corresponding author: Blanco Encalada 1543, 1427 Buenos Aires, Argentina. mstrivi@icba-cardiovascular.com.ar