Keywords
INTRODUCTION
Atrial septal defect (ASD) is a chronic model of volume overload of the right chambers of the heart.
Right ventricular function is difficult to examine with conventional Doppler echocardiography because of the insufficient development of adequate, reliable mathematical models to reconstruct its complex geometric shape.1 The use of pulsed tissue Doppler, a commonly used new ultrasound technique, allows mitral and tricuspid annular motion to be studied and has enhanced the noninvasive examination of right and left ventricular systolic and diastolic function.2-5 Eidem et al6 established the reference values for velocities obtained by pulsed tissue Doppler in a healthy pediatric population. In addition to indexes obtained by tissue Doppler, new indexes derived from color M-mode echocardiography appear to be useful for noninvasive examination of left ventricular diastolic function in children.7
Because ventricular dysfunction (whether right or left, systolic or diastolic) plays an important role in the morbidity and mortality of many patients with congenital heart diseases, the measurement of dysfunction using noninvasive techniques is essential. The purpose of the present study was to determine if a large shunt in the interatrial septum affects ventricular function, as observed by reliable echocardiographic indexes increasingly used in current practice.
METHODS
Between January 2003 and March 2006, 158 children who came to the Cardiology Department of Hospital Pediátrico Dr Humberto Notti were included in this prospective study. The subjects were divided into 2 groups. Group 1 included 111 patients (68 girls and 43 boys; mean age, 6.5 years; range, 22 months to 15 years) with ostium secundum ASD and documented volume overload of the right chambers. All patients were in sinus rhythm at the time of diagnosis, none had clinical heart failure, and the estimated pulmonary pressure was less than 75% of the systemic pressure. The study excluded patients younger than 2 years of age, patients with estimated pulmonary pressure 375% of systemic pressure, and patients with ostium primum ASD and venous sinus, because these conditions are usually associated with mitral cleft and partial anomaly of pulmonary venous return, respectively. Patients with other concomitant heart diseases (pulmonary valve stenosis, ventricular septal defect, persistent ductus, mitral regurgitation, etc) were also excluded. Group 2 was composed of 49 children (24 girls and 26 boys; mean age, 7.5 years; range, 21 months to 14.3 years) with a normal cardiovascular examination (functional murmur) and sinus rhythm. These patients had been referred for color Doppler ultrasound due to chest pain, syncope, radiologic cardiomegaly, or suspected left ventricular hypertrophy on electrocardiography, but had a normal echocardiographic study. Patients with ASD who met the above criteria were selected consecutively, as were the children of similar age in the control group.
All patients underwent 2-dimensional echocardiographic study, color Doppler ultrasound, and pulsed tissue Doppler (Hewlett Packard SONOS 2500 unit with 4/2.5/2 MHz transducers) in supine decubitus and left lateral decubitus without sedation. The studies were video-recorded for subsequent analysis. Images were recorded at a rate of 100 mm/s and continuous 1-channel electrocardiographic monitoring was used throughout the study.
The right ventricular end-diastolic diameter7 (RVEDD) was measured in centimeters and corrected for body surface area. Left ventricular dimensions were measured using the conventional approach: the left ventricular enddiastolic diameter was measured at the start of the QRS complex and the end-systolic diameter, in late systole at the time of maximum contraction of the left ventricular posterior wall.8 Left ventricular systolic function was assessed by the ejection fraction (EF) and the shortening fraction (SF) obtained by M-mode.9
The pulmonary flow index compared with systemic flow (Qp/Qs) was also determined using standard techniques.10
The mitral velocities obtained by spectral pulsed Doppler (peak E wave and A wave velocities) were measured in meters per second. E wave deceleration time was measured in milliseconds as was the isovolumic relaxation time of the left ventricular outflow tract measured by spectral Doppler.11 The color M-mode mitral flow propagation velocity (Vp) was also determined as a diastolic function index independent of ventricular load.12,13
The myocardial velocities were measured by pulsed tissue Doppler in an apical 4-chamber view from 3 locations: lateral mitral annulus, interventricular septum, and lateral tricuspid annulus. The pulsed tissue Doppler measurements for each of these myocardial segments included the peak systolic annular velocity (SM wave and ST wave), the peak early diastolic mitral annular velocity recorded in the lateral portion (EML wave) and septal portion (EMS wave), the peak early diastolic tricuspid annular velocity (ET wave) and peak late diastolic mitral and tricuspid annular velocity (AM and AT waves).14 The E/A, E/EML, and E/Vp indexes were calculated from these measurements.
Statistical Analysis
All values are expressed as mean (SD). The normal distribution of the continuous cardinal variable was confirmed or rejected according to the Kolmogorov-Smirnov test. The differences between the 2 groups were then compared using the Student t test or 2-tailed Mann-Whitney test for nonpaired analysis, as applicable.
The c2 test was used to detect any differences for the dichotomous variable sex.
RESULTS
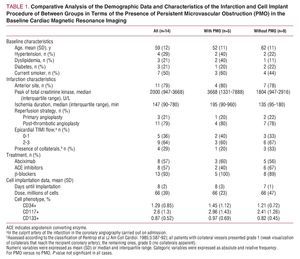
There were no statistically significant differences between the groups with regard to sex or age (group 1, 6.53 [3.92] years, vs group 2, 6.2 [2.68] years), although there were differences in body surface area (0.81 [0.27] m2 in group 1 vs 0.94 [0.33] m2 in the control group), which was significantly lower in the ASD group (Table 1).
The right ventricular end-diastolic diameter corrected by body surface area was significantly larger in the patients in group 1 (2.88 [0.99] vs 1.89 [0.67] cm; P<.0001), whereas the left ventricular end-diastolic diameter was smaller in group 1 than in the control group (3.74 [0.87] vs 4.4 [0.62] cm; P<.001) (Table 2).
Shunting estimated by the Qp/Qs ratio was significantly higher in group 1 than group 2 (1.74 [0.52] and 0.96 [0.15]; P<.0001).
No significant differences were found between group 1 and group 2 in EF (66.82% [8.8%] vs 69.86% [8.63%]; P=.1478) or left ventricular SF (36.69% [7.1%] vs 38.97% [7.6%]; P=.1972) (Table 2).
In terms of pulsed tissue Doppler velocities, the systolic mitral annular velocity at the lateral level (SM wave) was also similar in both groups (13.5 [9.53] vs 14.33 [14.1] cm/s; P=.4584), although the systolic lateral tricuspid annular velocity (ST wave) was significantly higher in the group with ASD (16.32 [2.7] vs 14.95 [3.59] cm/s; P=.0216) (Table 3, Figure 1).
Figure 1. Tissue Doppler images of the lateral edge of the tricuspid annulus showing ET (early diastolic), AT (late diastolic), and S (systolic) waves. A: patient from the control group. B: patient with ASD. Note the significant increase in late diastolic (AT) and systolic (ST) wave velocity.
The left ventricular diastolic function was assessed by analyzing the mitral spectral Doppler (E wave and A wave; E/A ratio and E wave deceleration time). No significant differences were observed between the 2 groups, except for the isovolumic relaxation time, which was significantly longer in group 1 compared with group 2 (51.31 [12.78] vs 43.65 [9.74] ms; P<.001) (Table 4).
The diastolic function was also assessed by color M-mode Doppler flow propagation velocity (Vp) and E/Vp ratio, with no significant differences found between the 2 groups (Table 5).
The early diastolic velocity in both the septal (EMS wave) and lateral (EML wave) portions of the mitral annulus was significantly lower in group 1 than group 2 (13.7 [5.58] vs 15.03 [2.73] cm/s, and 18.18 [5.3] vs 21.69 [4.22] cm/s, respectively; P<.001) (Table 6). There were no significant differences in early diastolic tricuspid annular velocity between the 2 groups (18.13 [5.29] vs 17.12 [4.05] cm/s; P=.1971), although the late diastolic tricuspid annular velocity was significantly higher in the group with ASD (14.79 [10.42] vs 11.15 [4.1] cm/s; P<.001) (Table 6).
The E/EML ratio obtained at the lateral portion of the mitral annulus was significantly higher in group 1 than group 2 (5.77 [2.45] vs 4.81 [1.35]; P=.1972) (Table 6).
DISCUSSION
Atrial septal defect represents a clinical model of chronic volume overload of the right ventricle. The study of this heart disease has always focused on the consequences of interatrial shunting for the right chambers and the pulmonary vascular tree. Furthermore, interatrial shunting decreases the left ventricular preload15 by decreasing ventricular filling, which could affect some of the indexes considered for assessment of ventricular function.
Left and right ventricular systolic and diastolic function abnormalities have been described in patients with congenital heart diseases. Ventricular dysfunction can affect the results obtained from therapeutic interventions and the medium- to long-term prognosis in these patients.
Berger et al16 found an early decrease in right ventricular end-diastolic volume after closure of the ASD with a device or by surgery. Gomez et al15 have described immediate changes in some echocardiographic indexes of left ventricular diastolic function in patients with ASD after closure by device, but attributed them to acute abnormalities of the left ventricular loading conditions produced by the closure. However, right and left ventricular systolic and diastolic function in patients with significant interatrial shunts compared with normal has not been sufficiently emphasized.
Conventional Doppler echocardiography is a simple, noninvasive approach used to measure various ventricular function indexes, currently enhanced by new technical modalities, such as measurement of myocardial velocities by tissue Doppler and left ventricular diastolic flow propagation velocity (Vp) by color M-mode Doppler echocardiography.
Weight development is below normal in patients with ASD17; our patients had a significantly smaller body surface area than the control group (P<.05). This would be linked with the hemodynamic repercussion generated by the atrial shunt, which results in volume overload of the right chambers and increased pulmonary venous flow to the detriment of systemic arterial flow, as was seen in our ASD patients. The right ventricular end-diastolic diameter and Qp/Qs ratio were both significantly higher in the ASD group than the control group, similar to the findings of other reports.17,18
The right ventricle has a spatial configuration, myocardial fiber architecture, and filling characteristics that differ from those of the left ventricle19 and has been compared to a piston, with a large capacity to offset the volume loads.20 Right ventricular function is difficult to measure using traditional echocardiographic methods because the mathematical equations are inadequate to reconstruct its complex geometric shape. However, tissue Doppler is an alternative approach to measuring the ventricular systolic and diastolic function of the right ventricle. Tricuspid annular velocity measurements obtained by tissue Doppler in an apical 4-chamber view appear to be highly reproducible.21 Eidem et al6 and Frommelt et al1 established the normal values in healthy children and affirmed that right ventricular systolic and diastolic function may be estimated noninvasively by spectral tissue Doppler of the tricuspid annular motion.
The measurement of tricuspid annular velocities by tissue Doppler reflects the changes in myocardial fiber length along the longitudinal plane, which is the main mechanism of right ventricular function.22 According to the Frank-Starling law, an increase in right ventricular contractility would be expected as a result of the increased myocardial fiber end-diastolic length generated by volume overload. A significant increase in right ventricular systolic function was observed in our ASD patients, when it was assessed by the myocardial velocity obtained by pulsed tissue Doppler at the lateral portion of the tricuspid annulus (ST wave).
The early diastolic tricuspid annular velocity (ET wave) was similar in patients with ASD and in the control group assessed by pulsed tissue Doppler. Because myocardial velocity is linked to right ventricular diastolic function,1 this finding would support the hypothesis that patients with ASD do not present right ventricular diastolic dysfunction. The late diastolic tricuspid annular velocity (AT wave) was significantly higher in patients with ASD. Because this wave correlates with atrial systole,1 the increased velocity seen in patients with ASD would be linked to more energetic right atrial systole, secondary to atrial volume overload.
As to the left ventricle, left ventricular end-diastolic diameter was significantly smaller in our ASD patients than in the control group, in keeping with findings from other authors,23 and would result from a decrease in ventricular preload.15 However, there were no differences in left ventricular systolic function between the 2 groups, assessed in both the circumferential plane (measured by ejection fraction and shortening fraction) and the longitudinal plane (pulsed tissue Doppler SM wave). Systolic myocardial velocity obtained at the lateral portion of the mitral annulus is a measurement of longitudinal left ventricular systolic function24 and correlates to ejection fraction25 and dP/DT ratio.26 Therefore, it could be inferred that ostium secundum ASD does not affect left ventricular systolic function.
Transmitral spectral Doppler has classically been used to assess the diastolic ventricular function. There were no significant differences in the traditional echocardiographic indexes obtained from the mitral spectrum between both groups, such as E/A ratio and the E wave deceleration time, but the isovolumic relaxation time was significantly prolonged. This last parameter is not a marker of diastolic function, however, but instead indicates changes in left ventricular morphology, which is what occurs in patients with ASD due to ventricular interdependence.27
Recently, mitral annular tissue Doppler and color M-mode Doppler have been used as effective echocardiographic tools to assess left ventricular diastolic function.
In children, the early diastolic mitral annular myocardial velocity (EM wave) correlates well with the left ventricular pressure-drop time constant (t)7; however, this index would be affected by ventricular preload.28,29 Studies conducted in adult patients found a close correlation between E/EM ratio and pulmonary capillary wedge pressure30 whereas children did not seem to show good correlation between E/M ratio and ventricular enddiastolic pressure.7
In our patients, the early diastolic mitral annular velocity (EMS wave and EML wave) was significantly lower in the ASD group than the control group, probably because of the decrease in left ventricular preload caused by left-to-right atrial shunting. The decrease in left ventricular preload would also explain why the left ventricular enddiastolic diameter was smaller in patients with ASD than in the control group, as has been reported by other authors.23 A decrease in early diastolic myocardial velocity within the mitral annulus also led to a significant increase in E/EML ratio among patients with ASD.
The propagation velocity of early left ventricular diastolic flow (Vp) obtained by color M-mode Doppler echocardiography is a new left ventricular relaxation index that is independent of preload.31 In addition, combining E (from mitral spectral Doppler) with Vp results in another index (E/Vp) that closely correlates to left ventricular end-diastole pressure in children.7
No significant differences in these indexes (Vp and E/Vp) were observed between the ASD patients and the control group and, therefore, it can be inferred that the lower early diastolic mitral annular velocity and increased E/EML ratio in patients with ASD indicates changes in ventricular preload.
Similar values for the left ventricular diastolic function indexes obtained by Doppler echocardiography (not dependent on ventricular preload) in both groups would support the hypothesis that patients with ostium secundum ASD do not present left ventricular diastolic dysfunction during the early years of life.
Clinical Implications
Ventricular dysfunction (whether right or left, systolic or diastolic) plays an important role in the morbidity and mortality of many patients with congenital heart diseases. Thus, it is essential to measure ventricular dysfunction using noninvasive techniques as it determines the long-term success of therapeutic interventions.
The results of this study show that asymptomatic patients with isolated ostium secundum ASD do not have left ventricular dysfunction during childhood and early adolescence and that only right ventricular systolic function increases in response to the volume overload imposed by this heart condition. This "benign" behavior of isolated ASD ostium secundum during the first years of life would explain the excellent results obtained with closure by conventional surgery or device placement.32
Further studies on ventricular function are needed to confirm that the condition is "benign." These should include studies in other patient subgroups, such as symptomatic infants or adults, or efforts to determine the long-term progress of patients who have already undergone surgery.
Limitations of the Study
Due to the complex nature of the mechanisms that determine ventricular function, the reliability of the echocardiographic indexes used may be questionable, particularly in patients with congenital heart disease.
Abnormal septal motility in patients with ASD affects measurement of the left ventricular diameters required to assess ventricular systolic function by EF and SF. Determination of the systolic myocardial velocity of the mitral annulus is another contribution to the study of the left ventricular systolic function and correlates with EF 25 and the dP/DT ratio.26 Although we found no significant differences in our ASD patients compared to the control group in the variables studied for ventricular systolic function, the use of new technologies that allow reliable calculation of actual three-dimensional ventricular volume probably provides more trustworthy data regarding ventricular systolic function in these patients.
The available echocardiographic techniques showed that left ventricular diastolic function was not affected in patients with ASD during childhood. However, additional studies that include new echocardiographic modalities, such as quantitative assessment of segmental myocardial motility, are needed to confirm that this entity does not lead to deterioration of ventricular function.
CONCLUSIONS
Left ventricular systolic function was similar in pediatric patients with ASD and a control group. Left ventricular diastolic function did not appear to be affected in these patients when assessed by independent echocardiographic indexes of ventricular preload.
A significant increase in right ventricular systolic function was observed in patients with ASD, which can be expected as a ventricular response to volume overload caused by the condition (Frank-Starling law). The right ventricular diastolic function was similar to that of the control group and the higher late diastolic myocardial velocity of the tricuspid annulus recorded is probably due to a more energetic right atrial systole caused by atrial volume overload.
ABBREVIATIONS
ASD: atrial septal defect
EF: ejection fraction
LVEDD: left ventricular end-diastolic diameter RVEDD: right ventricular end-diastolic diameter SF: shortening fraction
Vp: color M-mode Doppler flow propagation velocity
Correspondence:
Dr. A.M. Schroh.
Paso de los Andes, 812. (5500) Mendoza. Argentina.
E-mail: amschroh@yahoo.com; schroh@cardiologiainfantil.com
Received August 25, 2007.
Accepted for publication January 22, 2008.