To the Editor,
We report the case of a male aged 19, a native of Equatorial Guinea with typhoid and malaria as the only relevant history. He arrived in Spain 18 months earlier and since then has had dyspnoea, chills, joint pain, fatigue and palpitations. For this reason, he came to the emergency room of our hospital and was admitted to cardiology for study.
The patient was tachycardic and had an elevated jugular venous pressure. Auscultation revealed a third tone, a pansystolic III/IV murmur in the right sternal border and hypoventilation in both lung bases. He presented 6 cm pulsatile hepatomegaly and bilateral pitting oedema to the roots of both thighs.
Tests were normal. The electrocardiogram showed a common atrial flutter with a ventricular response of 100 beats/min. Chest radiography revealed cardiomegaly at the expense of right cavities and bilateral pleural effusion.
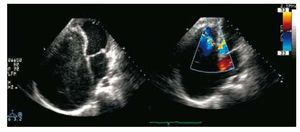
An echocardiogram was performed which showed a striking dilation of the right atrium and obliteration of the apex and inlet tract of the right ventricle with severe infundibular dilation. The tricuspid valve was in its normal position, but with thickening and retraction of its leaflets (Figure 1A). Colour Doppler showed severe tricuspid regurgitation (Figure 1B). The left cavities were normal.
Figure 1. A: echocardiogram (apical); aneurysmal dilatation of the right atrium, with spontaneous echo contrast, obliteration of the apex and right ventricle input tract with severe infundibular dilatation and tricuspid valve in normal position with thickened and retracted leaflets. B: Doppler. Severe tricuspid regurgitation.
A catheterisation was conducted, which revealed increased right ventricular pressure (34/21 mm Hg, with dip-plateau morphology) and the right atrium (18 mm Hg). The right ventriculography confirmed the obliteration of the apex and body of the right ventricle, severe tricuspid regurgitation and aneurysmal dilatation of the right atrium. Coronary arteries were normal.
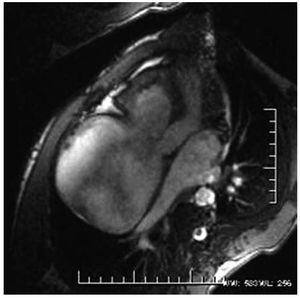
Cardiac magnetic resonance confirmed the findings described by the above techniques and showed enhancement at the apex of the right ventricle, compatible with fibrotic tissue (Figure 2).
Figure 2. Cardiac magnetic resonance: aneurysmal dilatation of the right atrium and right ventricle outflow tract. Highlight in the right ventricular apex, compatible with fibrotic tissue.
Given these findings, we considered the following diagnostic possibilities:
1. Ebstein's disease: does not meet the echocardiographic diagnostic criteria, since there is not a 2 cm displacement of the tricuspid septal leaflet with respect to the mitral.
2. Agenesis of the right ventricle: requires right-left shunt with cyanosis, and clinical manifestations appear in the neonatal period.
3. Loeffler's disease: is more typical in temperate countries, and usually has a more acute presentation and with eosinophilia.
4. Tropical endomyocardial fibrosis: manifests as a restrictive cardiomyopathy with obliteration of the entry tract and the apex of one or both ventricles.
Our patient meets most of the clinical, echocardiographic and angiographic criteria for diagnosis of tropical endomyocardial fibrosis or Davies' disease.
At the time of diagnosis, the patient was in functional class III, New York Heart Association (NYHA). With medical treatment (diuretics, beta blockers, anticoagulants, ACE inhibitors and aldosterone inhibitors), there was a significant clinical improvement, with reversion of the atrial flutter to sinus rhythm, so it was decided to instigate an initial conservative management and leave other therapeutic options open in case there was a deterioration in functional capacity.
Tropical endomyocardial fibrosis is a restrictive cardiomyopathy of unknown aetiology, endemic to tropical and subtropical countries. Patients are usually young, the onset of the disease and its clinical manifestations are insidious, and its prognosis is poor.
The first published reference to this disease is attributed to A.W. Williams, who published his findings on two patients in Uganda who died of congestive heart failure due to large patches of fibrosis affecting the ventricular walls. J. Davies was the first to study this condition in 1948 and recognise its endemic nature.
The most common-affectation is biventricular (50%), followed by left univentricular in 40% of cases and right univentricular in 10%.1
The diagnosis is based on clinical, echocardiographic and angiographic findings. More recently, cardiac MRI2 has been used to confirm the diagnosis and for follow-up after medical and/or surgical treatment.
The clinical course depends on the functional level, the severity of the fibrosis and degree of regurgitation. Patients in class III or IV have a 50% 2-year mortality, and death occurs from progressive heart failure or sudden death. Predictive mortality factors in a series of 145 patients3 were the presence of cyanosis, NYHA functional class III-IV and diastolic pressure of the right atrium >20 mm Hg.
Although surgical mortality can be high (15%-20%), in a published series monitored over 7 years,4 overall survival at 17 years was 55%. That is, surgery (endocardial decortication with valve repair or replacement)5 should be recommended to patients in advanced functional levels, to improve their survival and functional class.
One year after being discharged from hospital, our patient has had periodic checks and is in NYHA functional class II and in sinus rhythm, with good adherence to treatment.