To the Editor,
Pheochromocytomas are tumours producing catecholamines, released mainly by secreting chromaffin cells originating from embryonic neurectodermal cells. Extra-adrenal tumours are also called paragangliomas, and there are 2 types. The first are chemodectomas, which are negative chromaffin tumours originating in the parasympathetic chain that are often not functioning in their intrapericardial location.1 The second are positive chromaffin pheochromocytoma from the sympathetic nervous system. Although these tumours are a cause of hypertension in the general population, their surgical removal may cure this. Its incidence in the general population is between 0.001% and 0.01%.2 Thoracic paragangliomas comprise only 1%-2% of cases of pheochromocytomas and are normally located in the posterior mediastinum.3 Intracardiac or intrapericardial pheochromocytomas are extremely rare, with no more than 50 reported cases. They are usually located in the left atrium, although they have been found in the right atrium, the atrial septum or, as in our case, at the level of the aortic root in front of the left atrium and in the immediate vicinity of the coronary ostia,4,5 in which case they may be painful.6 The diagnosis and exact location of the tumour is crucial for planning surgery.
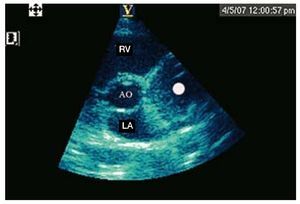
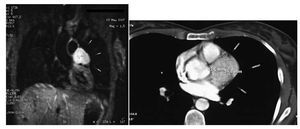
We report the case of a 38-year-old woman, previously operated on for breast fibroadenoma which was the only incident in her background, who attended the emergency department for a respiratory infection. Her chest x showed she had an impaired cardiac silhouette. The physical, laboratory and electrocardiogram examinations were normal. The echocardiogram (Figure 1) showed a mass of 4 cm in diameter below the pulmonary artery and at the level of the interventricular sulcus from the left atrium to the aorta (marked with a dot on the figure). A chest computed tomography (CT) was performed (Figure 2), which showed a heterogeneous lesion of 4´4 cm at the level of the heart, above the left ventricle and connected to the pericardium. The possibilities of pericardial mass were considered (teratoma, mesothelioma lipoma or melanin tumour). Magnetic resonance imaging (Figure 2) confirmed these findings, as well as showing that it was hyperintense with contrast, with signs of vascularisation. The patient underwent thoracic surgery with resection of the intrapericardial mass and pulmonary artery enlargement with a pericardial patch. Positron emission tomography (PET) was performed, which showed no other lesions. The pathology report revealed that the mass corresponded to a paraganglioma, which was considered benign by the extension study. A year later the patient is still asymptomatic with normal catecholamine analytical results.
Figure 1. Echocardiogram showing a point indicating a mass of 4 cm in diameter below the level of the pulmonary artery and interventricular sulcus.
Figure 2. Chest computed tomography showing a heterogeneous lesion of 4×4 cm at the level of the heart, above the left ventricle and in connection with the pericardium; and a magnetic resonance image confirming these findings. Note the hyperintense signal that captures contrast, with signs of vascularisation.
This tumour is extremely rare. The absence of symptoms and signs indicating pheochromocytoma or other cardiac symptoms makes it difficult to diagnose. Seventy-five percent of patients have abnormal chest x-rays, as in our case. Although sensitivity is low for intrapericardial tumours. Metaiodobenzylguanidine scintigraphy, chest CT and MRI scans are essential for diagnosis and location. In our case, PET-CT was performed, of which we unfortunately have no record. In magnetic resonance images, paragangliomas are highly vascular tumours and the capacity of this technique for the diagnosis and anatomic characterisation of the tumour is greater than CT, as there is more tissue contrast even without administering contrast drugs.7
This, therefore, is the technique of choice. In our patient, catecholamine determinations were negative and no symptoms indicating tumour secretory activity had been noticed. All intrapericardial paragangliomas require resection.