To the Editor,
Disconnection of the pulmonary artery (PA) is unusual. First described in 1868,1 it is generally associated with other cardiovascular malformations.
We present the case of a newborn boy diagnosed in the immediate neonatal period with type III esophagal atresia. The preoperatory echocardiography revealed a left aortic arch, absence of connection of the right pulmonary artery (RPA) with the trunk of the PA, and presence of persistent ductus arteriosus (PDA) in the normal position. Moreover, we observed an anomalous vessel originating in the first supraaortic trunk and descending to the RPA. Cardiac catheterization confirmed RPA discontinuity and a vascular stump at the base of the innominate trunk (Figure 1). Treatment began with prostaglandin E1 (PGE1) given we suspected the presence of ductal tissue in the aforementioned vessel and later confirmed collateral systemic-pulmonary permeability from the base of the innominate trunk, connected with the RPA (Figure 2). We maintained PGE1 perfusion and, once the digestive malformation had been corrected, performed corrective surgery to resection the ductal tissue and reconstruct the RPA with an API flap and pulmonary trunk, widening with a patch of trunk and RPA and direct connection of the RPA to the trunk of the PA. Five months later, the patient presented severe stenosis of the RPA with 1 mm critical diameter. We performed predilatation with a 4´20 mm balloon catheter, inflated to 8 atm, and subsequent implantation of a previously assembled 5´18 mm stent in a 5 mm balloon. Angiographic results were good and right ventricular (RV) pressure diminished from 100% to 75% with respect to systemic pressure. At 2 years, the patient required overdilatation of the stent with a 9´20 mm balloon catheter and inflation to 14 atm, with significant angiographic improvement and RV pressure 50% of systemic pressure.
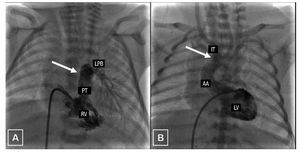
Figure 1. Angiographic images. A: note the right ventricle (RV), pulmonary trunk (PT), and left pulmonary branch (LPB), with the absence of a right branch (indicated by an arrow). B: visualization of left ventricle (LV), ascending aorta (AA), and innominate trunk (IT). The presence of a vascular stump at the level of the base of IT is indicated.
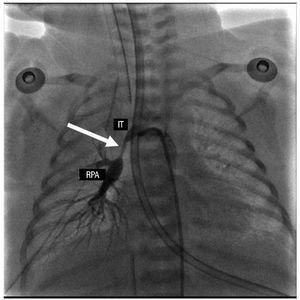
Figure 2. Angiography showing the repermeabilization of the collateral that communicates the innominate trunk (IT) with the right pulmonary artery (RPA) after treatment with prostaglandin E1.
The disconnection of a PA associated with a double ductal system is an exceptionally rare congenital cardiomyopathy. It usually coexists with other cardiovascular malformations2 (above all when the branch affected is the API), fundamentally tetralogy of Fallot, common arterioso trunk, and septal defects. The discontinuity of a pulmonary branch without other cardiac anomalies is generally located contralateral to the aortic arch and is more frequently found in APD.3 A double ductal system is usually found with a right aortic arch4 and is associated in more than 50% of patients5 with nonconfluent pulmonary arteries, as in the case we present. Between 12% and 30%3 of patients affected by isolated agenesia of a PA (in reality, a proximal affection, with permeable pulmonary vascularization) will remain asymptomatic. In their clinical course,3 the rest will present recurrent pneumonias (38%; attributed to alveolar hypocapnia inducing bronchoconstriction, alteration of mucociliary clearance and inadequate response to inflammatory mediators), haemoptysis (20%; due to excessive collateral circulation), pulmonary hypertension (PHT) (20%-25%; of controversial etiology) and scoliosis (as a consequence of homolateral pulmonary hyperplasia leading to a diminution of hemithorax volume). Initially, diagnosis is suspected from radiologic findings (absence of hilar shadow, diminution of vascular marks and hemidiaphragm elevation of the affected side, with homolateral mediastinal deviation) and echocardiographic findings; anatomic evaluation can include catheterization or magnetic resonance imaging. Early corrective surgery should be performed to avoid the complications described, permit normal development of the pulmonary vascular bed and, thus, prevent the onset of PHT. However, these patients frequently require reintervention,6 as in the case we present. We would stress the value of continuous PGE1 perfusion, widely known to be used in cyanogenic congenital cardiomyopathy depending on the ductus and which, in this case, served to repermeabilize the ductal structure located between the innominate trunk and the RPA and permitted us to maintain adequate perfusion to the right lung until corrective surgery could be performed.