We present the case of a 47 year old patient with a history of bicuspid aortic valve disease, severe symptomatic stenosis and dilation of the ascending aorta who underwent an aortic root reconstruction using the Bentall procedure.
Two years after surgery, asymptomatic until then, the patient experienced general discomfort with progressive dyspnea, orthopnea and atypical chest pain for 1 month. The evolution was slow, gradually evolving to dyspnea on minimal effort. An electrocardiogram (ECG) revealed diffuse subendocardial injury and increased biomarkers (troponin I 31.6 ng/mL; creatine kinase-MB 147 IU/L) and the patient was referred to our center for an emergency coronary angiogram.
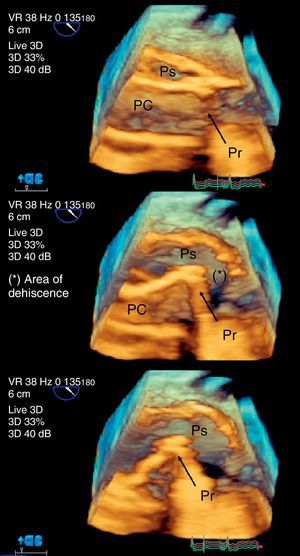
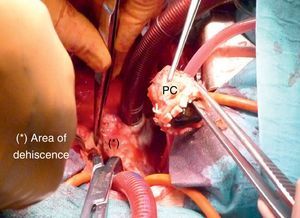
Our initial examination found the following: the patient was generally unstable, hypotensive (90/60mmHg) and tachycardia, no fever, dyspnea at rest, grade 3/6 aortic systolic murmur radiating to the carotids, ECG showing ST depression in V3-V6 and leukocytosis (29 000/µL). A transthoracic echocardiogram was performed, revealing abnormal movement of the prosthetic ring (Pr) suggesting dehiscence with grade III/IV periprosthetic aortic regurgitation. The study was completed with a real-time 3-dimensional transoesophageal echocardiography. We observed complete prosthetic valve dehiscence (Fig. 1) and a periprosthetic cavity at the level of the aortic root, corresponding to a pseudoaneurysm (Ps) with an internal flow and systolic collapse of the prosthetic conduit (PC) (Fig. 2). Emergent surgery was performed, which confirmed the echocardiographic findings (Fig. 3). The aortic valve conduit was replaced. Blood cultures were positive for Enteroccus faecalis, and the patient therefore completed 6 weeks of antibiotic treatment with ampicillin and streptomycin. Postoperative progress was good with no complications.
.