In line with the policy on clinical practice guidelines established by the Executive Committee of the Spanish Society of Cardiology (Sociedad Española de Cardiología [SEC]),1 the present article aims to discuss the most salient and novel features of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) guidelines for the management of arterial hypertension (HT) published in 2013.2 These guidelines update the recommendations published in 20073 and their reappraisal by the ESH in 20094 and incorporate the new evidence on HT that has emerged since then. These guidelines are aimed at all clinicians involved in the management of HT (primary care physicians, cardiologists, nephrologists, endocrinologists, internists, etc).
2METHODSThe Clinical Practice Guidelines Committee of the SEC established a task force composed of cardiologists and specialists in internal medicine, who were experts in the various aspects of HT covered by the ESC/ESH guidelines. The members of this working group were proposed by the Vascular Risk and Cardiac Rehabilitation Section of the SEC, with the general aim of reviewing the evidence and recommendations provided by the ESC/ESH document.2 All members of the task force were asked to analyze the guidelines, based on a basic questionnaire that included the following areas: a) analysis of the methodology; b) novel or salient contributions for clinical practice; c)analysis of the most positive and most debatable features of these novel contributions; d)unresolved issues, and e)conclusions and implications for clinical practice in Spain. On the basis of these experts’ comments, a consensus document was drafted, which was approved by all the members of the task force. The document was then sent for review to another group of experts, also proposed by the Vascular Risk and Cardiac Rehabilitation Section, and their comments were included in the final document.
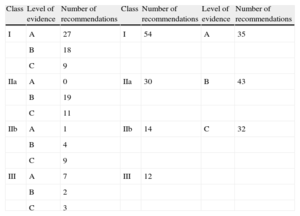
3GENERAL COMMENTS AND ANALYSIS OF THE METHODOLOGYFrom the methodological point of view, the main difference between the 20 07 and 2013 versions is that, in the latter, the r ecommendations with their corr esponding classes of recommendation (I, IIa, IIb, and III) and levels of evidence (A, B, and C) are presented in tables, whereas in the former, the evidence was discussed in the text, with lists of statements and very few tables. The 2013 guidelines contain a total of 110 recommendations, fewer than other ESC guidelines published in the last few years on various diseases, which aids clarity. As shown in Table 1, the proportion of recommendations with level C evidence (expert consensus, without data from randomized studies or meta-analyses) is low in the 2013 HT guidelines, representing only 29% of the total compared with, for example, 50% in recent guidelines on dyslipidemia and atrial fibrillation.5,6 Most recommendations are supported by level B (39%) or A (32%) evidence, based on clinical trials or meta-analyses. Almost half of the recommendations are class I (unanimous consensus, with no controversies). A high grade of evidence is therefore available for the management of HT, thus enhancing the value of the document.
Recommendations of the 2013 European Guidelines on the Management of Arterial Hypertension by Class of Recommendation and Level of Evidence
| Class | Level of evidence | Number of recommendations | Class | Number of recommendations | Level of evidence | Number of recommendations |
| I | A | 27 | I | 54 | A | 35 |
| B | 18 | |||||
| C | 9 | |||||
| IIa | A | 0 | IIa | 30 | B | 43 |
| B | 19 | |||||
| C | 11 | |||||
| IIb | A | 1 | IIb | 14 | C | 32 |
| B | 4 | |||||
| C | 9 | |||||
| III | A | 7 | III | 12 | ||
| B | 2 | |||||
| C | 3 |
The guidelines are structured in several sections (epidemiological aspects, diagnostic evaluation, organ damage assessment, treatment approach, treatment strategies, treatment strategies in special conditions, resistant HT, treatment of associated risk factors, and follow-up and HT disease management), whose most novel, salient, and debatable aspects are reviewed below.
4SALIENT OR NOVEL CONTRIBUTIONS: CRITICAL APPRAISALThe most important or novel contributions identified by the task force are listed in Table 2.
Most Salient or Novel Aspects in the Guidelines
| 1. Epidemiology and total cardiovascular risk | • Incorporation of the SCORE model to estimate total cardiovascular risk |
| • Importance of risk-modifying factors; asymptomatic organ damage is added as a risk modifier | |
| • Removal of metabolic syndrome as a risk modifier | |
| 2. Diagnostic assessment | • Changes in the classical dual-axis risk stratification table |
| • Greater importance of out-of-office BP values | |
| • Recommendation not to use wrist sphygmomanometers | |
| 3. Organ damage assessment | • Table of recommendations to be followed to assess organ damage |
| 4. Treatment approach and treatment strategies | • Simplification of BP targets (<140/90 mmHg in almost all conditions, with some exceptions: diabetes mellitus, older patients) |
| • The idea “the lower, the better” has been discarded | |
| 5. Treatment strategies | • Importance of lifestyle modifications |
| • Drugs: all drug classes can be used as first-line therapy (without ranking in order of preference) | |
| • Aliskiren is not included (due to the lack of trials on morbidity and mortality) | |
| 6. Special conditions | • BP thresholds indicating the need to start treatment and targets in most special groups have been reviewed |
| 7. Resistant arterial hypertension | • Longer section than in the previous version |
| • Alternatives to drug treatment (carotid sinus stimulation, renal denervation) | |
| • Splerenone as an alternative to spironolactone in primary aldosteronism | |
| 8. Comprehensive treatment and follow-up | • Cost-effectiveness of organ damage monitoring with antihypertensive therapy (ECG, proteinuria) |
| • Schedule of follow-up visits: when and by whom | |
| • Role of multidisciplinary HT units |
BP: blood pressure; ECG, electrocardiography; HT: hypertension.
The 2013 guidelines make no major changes concerning the epidemiology of HT. The classification adopted in the 2003 and 2007 versions is retained;3 this classification defines HT as systolic blood pressure (BP) >140mmHg and diastolic BP > 90mmHg, except in children and adolescents, in whom the classification continues to be based on BP percentages for age and sex. Unlike American guidelines, the ESC/ESH guidelines maintain their stance against the concept of prehypertension.
One of the main novelties in cardiovascular risk assessment is the incorporation of the SCORE model, following the ESC guidelines on dyslipidemia5 and cardiovascular prevention.7 This risk should be modulated by the existence of risk-modifying factors (sedentariness, obesity, social deprivation, belonging to an ethnic minority, carbohydrate metabolism abnormalities, elevated triglyceride concentrations or low concentrations of high-density lipoprotein cholesterol, and a family history of premature cardiovascular disease), because risk in persons with these factors may be higher than indicated by the SCORE model. In addition, the guidelines include the presence of asymptomatic organ damage (whose definitions have been updated, as discussed below) as a new risk modifier.
Controversially, 2 distinct–although possibly complementary– systems for risk stratification are proposed in these guidelines: one based on the table of BP values and additional risk factors and another based on the SCORE model. The guidelines do not specify when to use one system or the other, although possibly both should be employed.
4.2Diagnostic EvaluationThe guidelines continue to assign prime importance to risk stratification based on a dual-axis table that presents risk as a function of BP values, risk factors, and comorbidities (diabetes mellitus, target organ involvement, and established cardiovascular disease). Some changes have been made to this table, although they are slight (elimination of the column with normal BP values and addition of a new row with classical risk factors). Metabolic syndrome has b een eliminate d as a risk modif ier and the descriptor “symptomatic” has been added to cardiovascular disease. A criticism of this table, which requires careful analysis of each patient and his or her comorbidities, is that it assigns the greatest weight in treatment decision-making to BP values and very little influence to level of risk.
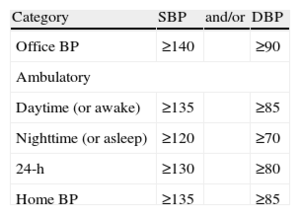
There are important novelties in BP measurement. Emphasis is placed on home BP monitoring (HBPM) and 24-h ambulatory BP monitoring (ABPM) because studies8 have indicated that these measurements are better correlated with organ damage and are more effective in estimating cardiovascular morbidity and mortality than office BP measurement. Compared with the 2007 version, the new document contains more specific definitions on the thresholds for diagnosing HT based on office measurements, HBPM and ABPM (Table 3), which is useful. Moreover, the 2013 guidelines specify how home measurement should b e carrie d out: wrist devices are not recommended, due to their lack of accuracy, and BP measurements should be taken at the same times (morning and night) on 7 consecutive days; values recorded on the first day should be excluded, with calculation of the average of the remaining measurements. Instructions are also given on how to carry out ABPM. With this type of measurement, the most important point is that, despite the variety of measurements and calculations, the main prognostic factor is the mean 24-h BP value. This implies a simplification, possibly not universally accepted, of its interpretation. However, no clinical trial to date has demonstrated a reduction in the incidence of cardiovascular complications with this type of measurement. Notably, the guidelines make no mention of the recent recommendation in the NICE (National Institute for Health and Clinical Excellence) guidelines of the need to confirm diagnosis of HT with ABPM in all patients.
Thresholds for Hypertension With Distinct Types of Blood Pressure Measurement
| Category | SBP | and/or | DBP |
| Office BP | ≥140 | ≥90 | |
| Ambulatory | |||
| Daytime (or awake) | ≥135 | ≥85 | |
| Nighttime (or asleep) | ≥120 | ≥70 | |
| 24-h | ≥130 | ≥80 | |
| Home BP | ≥135 | ≥85 | |
BP: blood pressure; DBP: diastolic blood pressure; SBP: systolic blood pressure.
In view of these changes, “masked” HT–that is, the form not detected in the office setting–has gained importance, because it is now known that this form carries an identical risk to that of persistent HT. Concerning exercise HT, most studies indicate that it predicts the development of HT at rest, but its prognostic value remains uncertain.
4.3Organ Damage AssessmentThis section is little changed from previous versions. The most significant new incorporations are listed below:
- •
Heart: a slight modification has been made to the Sokolov-Lyon index for left ventricular hypertrophy (>35mm; previously, 38mm) and RaVL has been added as a criterion of hypertrophy (>1.1mV). Emphasis is placed on the early detection of atrial fibrillation. With no clear jus tif ication, c hang es ha v e b een made t o the echocardiographic criteria for hypertrophy (mass >95 and >115g/m2 in women and men, respectively) and to pulse wave velocity (from 12 to 10 m/s). In ischemia assessment, the method of quantifying coronary reserve flow has been added as a prognostic factor.
- •
Arteries: intima-media thickness and the ankle-brachial index are the techniques considered to provide information on patients at intermediate risk. The intima-media thickness cut-off of 0.9mm has been retained for all patients (when it should possibly be higher in older patients to avoid overestimating risk in this population).
- •
Kidney: the es timate d glomerular f iltration ra te and microalbuminuria are emphasized, as these techniques are widely available and are cost-effective.
- •
Hypertensive retinopathy: the usefulness of hypertensive retinopathy assessment through direct ophthalmoscopy/fundoscopy is questioned, due to high interobserver variability in grade I and grade II retinopathy.
- •
Brain damage: new additions are microbleeds as significant lesions and the ability of magnetic resonance imaging to detect silent cerebrovascular lesions, which are more frequent than cardiac and renal subclinical damage, although there are no data to support the routine use of this imaging modality.
Greater em phasis is assigne d to the pre dictive role of electrocardiography (ECG), echocardiography, coronary computed tomography, and the ankle-brachial index, and cerebral magnetic resonance has been included for the first time. All hypertensive individuals should undergo an ECG, renal function evaluation, and microalbuminuria assessment (class I recommendation) and, if ischemic heart disease is suspected, a test for ischemia should be performed. This section could have been simplified by avoiding the addition of obvious statements such as the need to request a test for ischemia or Holter ECG when ischemia or arrhythmia is suspected, respectively, and by better definition of which patients (eg, those at moderate risk) should be investigated for arterial damage.
4.4Treatment Approach and Treatment StrategiesThere is a major change to this section, prompted more by the need to rework previous data than by new contradictory evidence. Because of its practical implications, the simplification of BP targets is striking. The 2007 guidelines3 recommended distinct– although highly “intensive”–targets for several clinical conditions. These targets have been conflated in the current guidelines: the recommended target is <140/90mmHg for almost all patients, with some e xcep tions, whic h ar e specif ie d b elo w. This simplification seems to be appropriate, because patients with values >140/90mmHg are undoubtedly at higher risk of ischemic heart disease, heart failure, and stroke. The reason for this change is that the paradigm of “the lower the better” seems to have been discarded in favor of the “J shaped” relationships between diastolic and systolic BP values and HT-related cardiovascular complications. There are 2 main exceptions. A diastolic BP value<85mmHg is recommended in diabetes mellitus. In older patients, systolic BP values between 140 and 150mmHg are considered acceptable, although–depending on the individual's physical and mental health status and treatment tolerance–attempts can be made to achieve the usual target (<140mmHg).
The other major topic of this section is when and how to start treatment. The well-known dual-axis table (with risk on the y-axis and BP values on the x-axis) is the same as in the 2007 version, except for the addition of BP targets in each box (even though the target is always the same: <140/90mmHg). The decision to start treatment, and its type and intensity, continue to be based on total risk, determined by office BP values and by the presence of other cardiovascular risk factors, asymptomatic organ damage, diabetes mellitus, any clinically manifest cardiovascular disease, or chronic kidney disease. In our opinion, this recommendation is appropriate. The guidelines continue to advocate treatment of low-risk grade 1 HP, although there are few scientific data to support this stance.
As mentioned in “Diagnostic Evaluation”, the emphasis on the usefulness of ABPM can also be considered a departure from the previous version, although the authors of the guidelines have not gone so far as to question office measurements as the gold standard for the diagnosis of HT, possibly due to the scarcity of studies on outcomes with this new parameter. At least the guidelines point out that the 2 determinations are not equivalent and should be used complementarily.
4.5Treatment StrategiesThis section is divided into 2 subsections: lifestyle modifications and pharmacological therapy.
- •
The guidelines stress that the management of HT should be based on lif es ty le modif ications, with no dela y in the s t art of pharmacological therapy. New recommendations are provided on diet, the most important being the following: the need for public health policies to reduce the salt content of food, with the participation of governments, the food industry, and the general public; advice on the Mediterranean diet, with fruit and vegetable intake daily and fish consumption at least twice weekly; data indicating that soya milk seems to reduce BP more than skimmed milk and that there is no definitive evidence to advocate or warn against coffee drinking in hypertensive individuals. Due to the vasoconstrictor effect of tobacco, the guidelines stress the need for complete abstinence.
- •
In pharmacological therapy, the guidelines reconfirm that the 5 main groups—diuretics (including thiazides, chlorthalidone and indapamide), beta-blockers, calcium antagonists, angiotensin- converting enzyme (ACE) inhibitors, and angiotensin receptor blockers (ARB)–can all be used for the initiation and maintenance of antihypertensive treatment, either as monotherapy or in combination (class I, level of evidence A). There is no general ranking of antihypertensive drugs in order of choice. The guidelines do not support the superiority–noted by some meta-analyses–of chlorthalidone or indapamide over hydrochlorothiazide, due to the lack of randomized trials including head-to-head comparisons among the distinct diuretics. The document also stresses that the results of several meta-analyses have shown no association between cancer and the use of ARB. Aliskiren, the only direct renin inhibitor on the market and the only new antihypertensive drug to appear since the 20 07 version, has not b een incorporate d in the recommendations b eca use data are available onl y on its antihypertensive efficacy and favorable effect on markers of organ damage, while no trial has evaluated its effect on cardiovascular or renal morbidity and mortality in HT. Moreover, a trial in diabetic patients (ALTITUDE), in which aliskiren was administered as an adjunct to an ACE inhibitor or ARB, was stopped because of renal complications, hyperkalemia, and hypotension.9 As in the previous guidelines, the 2013 version recommends initiating treatment with combination therapy in patients at high risk or with higher BP values, although the general recommendation for starting treatment with a combination of drugs is assigned to class IIb. Since 2007, 3 large-scale clinical trials (ACCOMPLISH, ADVANCE and ONTARGET) have been published,10–12 whose results have been added to those of previous trials. The guidelines only discourage the combination of 2 renin-angiotensin system antagonists (an ACE inhibitor with an ARB or one of these together with a direct renin inhibitor) on the basis of the results of the ONTARGET10 and ALTITUDE9 trials; this is the first time that this combination has been explicitly excluded for the treatment of HT. Some–but not all–trials have indicated that a beta- blocke r-diuretic combination is less ef fective in re ducing cardiovascular events than an ARB-diuretic combination or an ACE- inhibitor-calcium antagonist combination, and the ACCOMPLISH trial demonstrated the significant superiority of an ACE inhibitor– calcium antagonist combination over an ACE inhibitor–diuretic combination.12 The current guidelines modify the classical figure in the form of a hexagon or diamond, in which the group “alpha- blockers” is replaced by “other antihypertensives”, composed of alpha-blockers, centrally-acting drugs, and mineralocorticoid receptor antagonists.
This section reviews treatment strategies in specific patient groups, such as older individuals, youth, women, and persons with comorbid conditions. A new development is that this section also includes treatment recommendations for patients with white-coat HT and those with masked HT. In general, lifestyle measures and close follow-up through out-of-office BP monitoring are advocated in white- coat HT, with pharmacological therapy being reserved for those patients with white-coat HT and high risk or target organ damage. In contrast, lifestyle modifications and drug treatment are recommended from the outset in patients with masked HT, because its prognosis is very close to that of in-office and out-of-office HT. Elsewhere in this section, the therapeutic targets in many of the “special situations” are reviewed again, which is somewhat repetitive, given that these targets have previously been specified under the corresponding heading (see “Treatment Approach and Treatment Strategies”). A missing element is some mention of the management of older patients with orthostatic hypotension or older patients receiving nonsteroidal antiinflammatory drugs, who are frequently seen in clinical practice. It might also have been appropriate to include recommendations for patients with syncope, who might be candidates for hypotensor withdrawal. In general, the treatment of HT in these special groups differs little from previous recommendations.
4.7Resistant Arterial HypertensionUnlike the 2007 guidelines and their reappraisal in 2009, the current guidelines contain a section on resistant HT, defined as BP>140/90 despite treatment with 3 or more drugs (including 1 diuretic but not necessarily a mineralocorticoid receptor antagonist) and appropriate lifestyle modifications. The guidelines stress that these patients should be investigated in specialist HT units to exclude causes of “false” resistance. This definition, which is fairly loose, could increase the prevalence of this type of hypertension, run the risk of discouraging physicians from optimizing drug treatment, and lead to excessive use of invasive techniques.
For the first time, the guidelines contain alternatives to medical treatment to lower BP in resistant HT. Stimulation of carotid sinus nerves via implanted devices and application of an electrode over the carotid sinus produces ver y marke d and persistent BP reductions with few adverse effects but, because of the restricted number of patients included in studies of this technique, no conclusions can yet be drawn on its effectiveness. Renal artery denervation using radiofrequency produces significant and lasting BP reductions and is given a class IIb indication (although for patients with BP≥160/110mmHg conf irme d by ABPM and diagnosed in a specialized HT unit). The discrepancy in BP values b etween the def inition of resistance and the indication of denervation is due to the inclusion criteria of the clinical trials that support the use of this procedure.13 The guidelines are prudent when evaluating the role of invasive techniques, which is apt considering the small sample sizes in the studies, the absence of data on their long-term efficacy and safety, and the lack of evidence on their impact on morbidity and mortality.
Other notable features of the guidelines are those relating to renovascular hypertension and primary aldosteronism. In renovascular hypertension, there is no evidence to support renal artery angioplasty in atherosclerotic stenosis with well-controlled BP and stable renal function (class III recommendation, level of evidence B). The indication for interventionism in cases of fibromuscular dysplasia seems clearer (class IIa, level of evidence B). In primary aldosteronism, the comment on eplerenone as an alternative to spironolactone in patients who experience adverse effects (gynecomasty and menstrual disturbances) is of interest.
4.8Comprehensive Management and Follow-upThe guidelines recommend comprehensive management of total cardiovascular risk and of the risk factors associated with HT: statins in patients with dyslipidemia to achieve the target established for individual cardiovascular risk and control of diabetes mellitus (glycohemoglobin<7%, accepting that, in patients with very advanced diabetes and in those who are weak, elderly, or have problems of self-management, the target of 7.5%-8% is also r easonable). The curr ent guidelines uphold the 20 0 7 recommendation of using antiplatelet therapy only in secondary prevention but mention that some patient subgroups without cardiovascular disease, such as those with HT and moderate renal dysfunction (glomerular filtration rate<45ml/min/1.73 m2) or very high cardiovascular risk, have benefitted from antiplatelet therapy, so long as the HT is well controlled. Another novel and salient feature is evidence of the cost-effectiveness of organ damage regression with antihypertensive treatment. Regression of left ventricular hypertrophy is the only b enef it that has b een unequivocally demonstrated to reduce cardiovascular complications. The guidelines recommend close follow-up with ECG and laboratory monitoring of proteinuria.
The recommendations on the follow-up of hypertensive patients are reasonable. Once antihypertensive therapy has been started, a control visit should be scheduled at 2 to 4 weeks, and good treatment response or lack of efficacy can be determined at 2 months. Given that BP usually remains stable after 3 to 6 months of treatment, there is no justification for further physician visits, which can be carried out by nurses or through other forms of communication. One visit yearly is advised for patients with white-coat HT or high-normal BP to control total cardiovascular risk. Because of the demonstrated benefit in BP control and in reducing cardiovascular complications, treatment and follow-up should be carried out in multidisciplinary units (primary care physicians, nurses, specialists, nutritionists, etc).
5UNRESOLVED ISSUESIn general, the guidelines provide adequate discussion of most of the important aspects of HT, although they should possibly be shorter and more schematic for ease of reading and practical application. Most of the unresolved issues are discussed in each of their corresponding sections; in most, the cause of the lack of definition is the lack of solid evidence.
The document would benefit from a clearer definition of which of the 2 strategies for stratifying total risk (the table of BP values and associated risk factors or the SCORE model) should be used or specification of which is more important. Also missing are recommendations on the management of older patients with orthostatic hypotension or syncope. The sections on HT and pregnancy and HT and stroke, especially in the acute phase, seem somewhat scanty, and there is a need for a review of specific guidelines on these topics. Once again, there is no mention of physician inertia in advising patients of lifestyle modifications or of patients’ reluctance to make these changes. The guidelines mention treatment steps, drug combinations, and even provide a definition of resistant HT, when what often fails is not the drug therapy. Perhaps it is time to mention specific measures in the guidelines that raise awareness of lifestyle modifications in both health care professionals and in patients and their families. Advantage should be taken of widely disseminated documents such as the guidelines to increase awareness of nonpharmacological measures, which are undoubtedly the most cost-effective of all treatments.
6PRACTICAL IMPLICATIONS IN SPAINThe recommendations made in the guidelines can be generally applied in Spain and in daily clinical practice. Possibly, better definition is required of multidisciplinary units, specialized HT units, and the introduction of renal artery denervation. Instead of indiscriminate application of this technique, suitable patients should be evaluated in specialized units, which would help to select those who would truly derive a benefit. Its rational use would also help the health authorities to cover the cost of this procedure within the publicly-funded health system, which is not currently the case in all autonomous communities in Spain, and some agencies for new health technology assessment have rejected its inclusion in the health services portfolio. Although further long-term studies are required and recent publications have detected a smaller BP reduction than that in previous reports, the currently available data indicate that renal denervation can be cost- effective, given the high morbidity and mortality associated with resistant HT.14 Lastly, and given the serious problem of the sustainability of the publicly-funded health system, a shortfall is the absence of estimation of the cost-effectiveness of the distinct recommendations. Given the high prevalence of HT, solid recommendations should be made that would allow resource prioritization.
7CONCLUSIONSThe new ESC-ESH 2013 guidelines on HT are of great interest, clearly present the new evidence, and make specific, practical recommendations mostly based on a high level of evidence, without departing greatly from previous versions. The number of level C recommendations is not high and thus most recommendations are based on solid evidence. The application of the new recommendations should enhance the quality and efficiency of the care of patients with HT. To achieve this, it is essential to achieve consensus among the various scientific societies that also treat HT (nephrology, internal medicine, primary care, etc.) in order to carry out joint dissemination initiatives with a common message. It does not seem rational to have distinct guidelines on the same disease, each supported by a different society, with distinct messages and diagnostic and treatment strategies.
8CONFLICT OF INTERESTSP.M.R.: consultancies, presentations, manuscript preparation (Take da, Daichi-Sankyo, Bayer). F.X.G-M.M.: consultancy, presentations, grants (Daichi-Sankyo, Kowa, Menarini, Servier, Astra- Zeneca, Almiral, Bayer, Boehringer, Esteve, MSD, Novartis, Rovi, Recordati). P.J.M.B.: grants (Daichi-Sankyo SEC). M.S.: presentations, congresses (Boehringer, Bayer, Almiral, Astra-Zeneca, Pfizer-Bristol, Terumo).
Task force of the SEC on the ESC/ESH guidelines for the management of arterial hypertension 2013: Manuel Anguita Sánchez (coordinator), Enrique Galve Basilio (coordinator), Eduardo Alegría Ezquerra, Miguel Camafort Babkowski, Alberto Cordero Fort, Juan Cosín Sales, Lorenzo Fácila Rubio, Pilar Mazón Ramos and José R. Rumoroso Moreno.
Expert reviewers of the ESC/ESH guidelines for the management of arterial hypertension 2013: Xavier Armengol i Castells, Pedro Blanch Gracia, Almudena Castro Conde, Regina Dalmau González- Gallarza, Carmen de Pablo y Zarzosa, Isabel Díaz Buschmann, Francisco X. García-Moll Marimón, Esteban García Porrero, José Guindo Soldevila, Pedro J. Morillas Blasco, Juan Quiles Granado, Adriana Saltijeral Cerezo and Marcelo Sanmartín.
Clinical Practice Guidelines Committee of the SEC: Ángel Alonso-Gómez, Manuel Anguita Sánchez, Ángel Cequier Fillat, Josep Comín Colet, Isabel Díaz-Buschmann, Ignacio Fernández-Lozano, Antonio Fernández Ortiz, José J. Gómez de Diego, Manuel Pan Alvarez- Osorio and Fernando Worner Diz.
Complete list of authors are listed in the Appendix.