In line with the policy on clinical practice guidelines established by the Spanish Society of Cardiology (Sociedad Española de Cardiología [SEC]),1 this document discusses the most salient, novel and controversial features of the guidelines on diabetes, prediabetes and cardiovascular disease (CVD) issued jointly by the European Society of Cardiology (ESC) and the European Association for the Study of Diabetes (EASD). At the initiative of the Clinical Guidelines Committee of the SEC, the Vascular Risk and Cardiac Rehabilitation Section selected a group of experts to analyze the document published by the ESC and translated to Spanish for Revista Española de Cardiología.2 Both the authors and the reviewers have declared their conflicts of interest, which are listed at the end of this article.
This is the second time (the first guidelines were published in 20 07)3 that the ESC and EASD have come together to issue recommendations on the management of diabetes mellitus (DM), prediabetes, and CVD. This update is justified by the time elapsed since the publication of the first guidelines; since then, cardiologists have increasingly perceived the need to become well-versed in DM, and major advances have been made in glucose-lowering drugs; moreover, important results of clinical trials that were ongoing when the previous guidelines were drafted have now been published.
The authors of the current guidelines have included 546 references (vs 711 in the previous document), of which 331 are new publications (since 2007). The document contains 83 recommendations: 51 class I, 20 IIa, 6 IIb and 6 III; 36 are made with level of evidence A, 27 B and 20 C. Although most of these recommendations seem to be based on studies and registries, with few being based on expert opinion (level C), many sections contain no recommendations. The authors of the guidelines have identified 29 gaps in knowledge; however, after carefully reading the document, the authors of the present article have identified more gaps.
INTRODUCTIONThe global prevalence of DM is increasing; in 2011, 360 million persons had diabetes, of which 95% have type 2 DM (T2DM). In 2030, there will be approximately 552 million persons with diabetes, although only half will be aware of their disease. Moreover, 300 million persons will be at risk of developing diabetes, including those with impaired fasting glucose (IFG), impaired glucose tolerance (IGT), gestational DM and euglycemic insulin resistance. In 2011, it was estimated that 600 million adults had DM, but that only 50% were diagnosed. Even more alarming are the data from the Di@bet.es study,4 carried out in Spain, indicating that the prevalence of known DM was as high as 7.8% (3 million inhabitants) and that of unknown diabetes was 6% (approximately 2.3 million inhabitants). Given the extremely high percentage of diabetic patients that will develop CVD and the influence of DM on its prognosis, it is essential to have information on how the comprehensive management of these patients is being conducted at the present time.
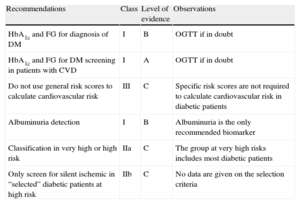
SALIENT AND NOVEL CONTRIBUTIONSThe authors of the present article have identified several topics of interest; the most important are summarized in 2 tables, with their class of recommendation, level of evidence, and some observations.
Main Features of the Diagnosis of Diabetes Mellitus and Cardiovascular Risk Stratification
| Recommendations | Class | Level of evidence | Observations |
| HbA1c and FG for diagnosis of DM | I | B | OGTT if in doubt |
| HbA1c and FG for DM screening in patients with CVD | I | A | OGTT if in doubt |
| Do not use general risk scores to calculate cardiovascular risk | III | C | Specific risk scores are not required to calculate cardiovascular risk in diabetic patients |
| Albuminuria detection | I | B | Albuminuria is the only recommended biomarker |
| Classification in very high or high risk | IIa | C | The group at very high risks includes most diabetic patients |
| Only screen for silent ischemic in “selected” diabetic patients at high risk | IIb | C | No data are given on the selection criteria |
CVD, cardiovascular disease; DM, diabetes mellitus; FG, fasting glucose; HbA1c: glycated hemoglobin; OGTT, oral glucose tolerance test.
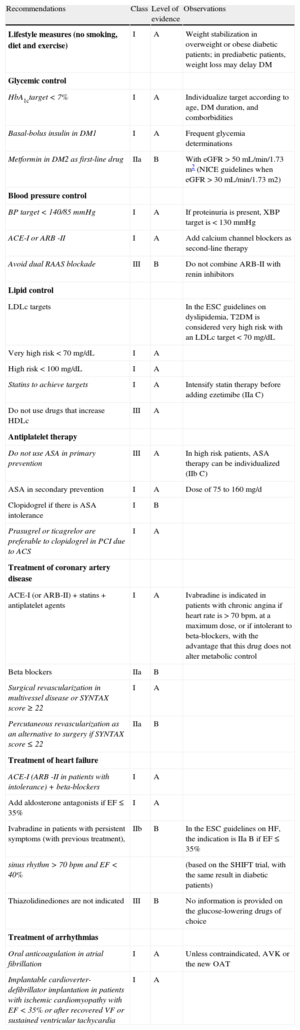
Main Treatment Features. Therapeutic Targets, Lifestyle, and Drugs
| Recommendations | Class | Level of evidence | Observations |
| Lifestyle measures (no smoking, diet and exercise) | I | A | Weight stabilization in overweight or obese diabetic patients; in prediabetic patients, weight loss may delay DM |
| Glycemic control | |||
| HbA1ctarget < 7% | I | A | Individualize target according to age, DM duration, and comborbidities |
| Basal-bolus insulin in DM1 | I | A | Frequent glycemia determinations |
| Metformin in DM2 as first-line drug | IIa | B | With eGFR > 50 mL/min/1.73 m2 (NICE guidelines when eGFR > 30 mL/min/1.73 m2) |
| Blood pressure control | |||
| BP target < 140/85 mmHg | I | A | If proteinuria is present, XBP target is < 130 mmHg |
| ACE-I or ARB -II | I | A | Add calcium channel blockers as second-line therapy |
| Avoid dual RAAS blockade | III | B | Do not combine ARB-II with renin inhibitors |
| Lipid control | |||
| LDLc targets | In the ESC guidelines on dyslipidemia, T2DM is considered very high risk with an LDLc target < 70 mg/dL | ||
| Very high risk < 70 mg/dL | I | A | |
| High risk < 100 mg/dL | I | A | |
| Statins to achieve targets | I | A | Intensify statin therapy before adding ezetimibe (IIa C) |
| Do not use drugs that increase HDLc | III | A | |
| Antiplatelet therapy | |||
| Do not use ASA in primary prevention | III | A | In high risk patients, ASA therapy can be individualized (IIb C) |
| ASA in secondary prevention | I | A | Dose of 75 to 160 mg/d |
| Clopidogrel if there is ASA intolerance | I | B | |
| Prasugrel or ticagrelor are preferable to clopidogrel in PCI due to ACS | I | A | |
| Treatment of coronary artery disease | |||
| ACE-I (or ARB-II) + statins + antiplatelet agents | I | A | Ivabradine is indicated in patients with chronic angina if heart rate is > 70 bpm, at a maximum dose, or if intolerant to beta-blockers, with the advantage that this drug does not alter metabolic control |
| Beta blockers | IIa | B | |
| Surgical revascularization in multivessel disease or SYNTAX score ≥ 22 | I | A | |
| Percutaneous revascularization as an alternative to surgery if SYNTAX score ≤ 22 | IIa | B | |
| Treatment of heart failure | |||
| ACE-I (ARB -II in patients with intolerance) + beta-blockers | I | A | |
| Add aldosterone antagonists if EF ≤ 35% | I | A | |
| Ivabradine in patients with persistent symptoms (with previous treatment), | IIb | B | In the ESC guidelines on HF, the indication is IIa B if EF ≤ 35% |
| sinus rhythm > 70 bpm and EF < 40% | (based on the SHIFT trial, with the same result in diabetic patients) | ||
| Thiazolidinediones are not indicated | III | B | No information is provided on the glucose-lowering drugs of choice |
| Treatment of arrhythmias | |||
| Oral anticoagulation in atrial fibrillation | I | A | Unless contraindicated, AVK or the new OAT |
| Implantable cardioverter-defibrillator implantation in patients with ischemic cardiomyopathy with EF < 35% or after recovered VF or sustained ventricular tachycardia | I | A |
ASA, acetylsalicylic acid; ACE-I, angiotensin converting-enzyme inhibitors; ACS, acute coronary syndrome; ARB-II, angiotensin-II receptor blockers; AVK, antivitamin K agents; BP, blood pressure; eGFR, estimated glomerular filtration rate; ESC, European Society of Cardiology; EF: ejection fraction; HbA1c, glycated hemoglobin; HDLc: high-density lipoprotein cholesterol; HF, heart failure; LDLc: low-density lipoprotein cholesterol; OAT, oral anticoagulant therapy; T1DM: type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; PCI, percutaneous coronary intervention; RAAS, renin-angiotensin-aldosterone system; SBP, systolic blood pressure, VF, ventricular fibrillation.
The main novel feature in the diagnosis of DM is the introduction of glycated hemoglobin A1c (HbA1c) as a valid criterion (HbA1c ≥ 6.5%). Currently, the American Diabetes Association (ADA) and the World Health Organization share the same criteria but differ in their strategy. The ADA recommends fasting glucose (FG) and HbA1c determination, while the World Health Organization recommends FG and, if necessary, an oral glucose tolerance test (OGTT); the recommendation of the ADA is much more feasible, although an important caveat is the lack of diagnostic sensitivity of HbA1c, especially in patients with CVD.5 In contrast, the disadvantages of OGTT are that it involves more complex logistics and lack s reproducibility, while its advantage is its higher diagnostic sensitivity. The guidelines remind us that the definition of DM is based on the glucose level at which diabetic retinopathy occurs, which does not mean that lower levels are innocuous. The document stresses that prediabetic states (IFG plus IGT) increase the risk of CVD and that it is important to identify them. However, the recommended strategy consists of lifestyle changes, which have not generally reduced cardiovascular mortality, although such modifications do delay progression to DM. Because there are no differences in the approach to HbA1c in the prediabetes range (5.7%-6.4%) and IGT, the ADA does not advocate the performance of an OGTT. While this might be true for IGT, it is not true for possible new diagnoses of DM based on the results of OGTT, which would allow initiation of metformin therapy and would modify the thresholds of secondary prevention.
Screening for Diabetes MellitusIn the general population or the population with one or more risk factors and without CVD, the risk of developing DM is calculated through specific tables. If the risk is high, laboratory determinations are performed. When CVD is already established, the guidelines advocate direct determination of FG and HbA1c and the use of OGTT as a complementary test, if necessary. What the guidelines do not provide is a clearly defined strategy for how and when to screen for DM. The 2007 document recommended systematic performance of OGTT in all patients with CVD; however, it has become clear that this recommendation is not feasible and hs not been widely adopted by cardiologists. Although hospital admission would be an opportune moment to perform OGTT, an important consideration is that the results of OGTT could be somewhat falsified by stress hyperglycemia; the guidelines recommend delaying the test for 4 to 5 days after an acute coronary syndrome (ACS), thus supporting the use of OGTT in this scenario. The guidelines reprint a strategy to optimize the indication for OGTT according to a risk model, which may be a practical way to implement the current recommendations. Another possibility is to determine FG and HbA1c before discharge and, depending on the results and other risk factors, to indicate OGTT.5 Equally, this practice could be incorporated in cardiac rehabilitation and secondary prevention programs, independently of the healthcare level in which they are performed.
Molecular Basis Of Cardiovascular Disease In Diabetes MellitusThe section devoted to the physiopathology of CVD emphasizes the risk continuum across the spectrum of disorders of glucose metabolism and insulin resistance (IFG, IGT, DM) that ends in CVD and develops progressively over many years, starting with early endothelial dysfunction and inflammatory status which, through various cellular, lipid, inflammatory and thrombotic (more active in diabetic individuals) mechanisms, give rise to atherosclerotic lesions. The acute com plications of these lesions lead to clinical manifestations. This section stresses that macrovascular involvement precedes microvascular complications and is usually present in T2DM some time before diagnosis.
Cardiovascular Risk Assessment In Patients With DysglycemiaA new feature of the guidelines is the simplification of CVD risk stratification in DM and prediabetes. The document acknowledges that not all patients with DM, especially those with T2DM, have the same risk, and consequently not all patients can be indiscriminately assigned an “equivalent coronary risk”. Also stressed is the lack of usefulness of general risk scores and of those specific to the DM population, as shown by evaluation of these scores both individually and in meta-analyses; the guidelines specifically advise against the use of any of the general risk scores and, although no particular stance is adopted toward those designed for the diabetic population, the text suggests that they are unnecessary. The numerous biomarkers and imaging techniques studied provide little additional prognostic value.
The conclusions of the guidelines on CVD risk quantification, based exclusively on expert opinion, is that patients should be classified into 2 well-defined groups: a group at very high risk, which should include not only those who already have some clinical manifestations of CVD, but also those with other risk factors or target organ damage, and a group at high risk, which should include all other diabetic patients. This group would consist of a minority, as indicated by studies such as that by Vinagre et al,6 who evaluated the clinical characteristics and risk factors in more than 280,000 diabetic individuals followed-up in primary care in Catalonia.
The only biomarker that is especially useful for cardiovascular risk assessment in diabetic individuals is albuminuria. Further data, including cost-effectiveness studies, are required to establish the indications for imaging techniques to detect atherosclerosis, such as the ankle-brachial index, detection of coronary plaques, computed tomography coronary angiography, and carotid intima-media thickness.
The paragraph on gaps in knowledge mentions the need for strategies useful for the early detection of CVD in asymptomatic diabetic patients from the cardiological point of view.
Prevention of Cardiovascular Disease In Patients With Diabetes MellitusLifestyleGreater importance is attached to diet, but the updated guidelines are much more flexible and no longer recommend strict proportions of total energy provided by the major macronutrients, stressing instead appropriate energy intake adapted to the requirements of each patient and a diet based on fruits, vegetables, cereals, low-fat protein sources, and limited intake of saturated and trans-saturated fatty acids. The remaining recommendations are classical: quantifying and distributing carbohydrate intake, limiting salt consumption, and increasing fiber intake; there is no justification for antioxidant supplements (vitamins E and C).
An important novelty is that–in light of the PREDIMED trial,7 which demonstrated that the Mediterranean diet is associated with a lower incidence of major cardiovascular events and in which 50% of the participants were diabetic-, the percentage of dietary fat can be increased with vegetable fats, especially from extra virgin olive oil, dried fruits, and fish oils. Despite the energy contribution of these foods, a substudy of the PREDIMED trial7 also reported a reduction in the incidence of DM and metabolic syndrome.
The recommendations on physical exercise and smoking are traditional: aerobic exercise and resistance training should be carried out within a structured program for at least 150 minutes per week, regularly, and over time. Smokers should be offered a smoking cessation program that should include pharmacological support.
Glucose ControlAfter stressing that CVD is best prevented in diabetic individuals by tight control of all cardiovascular risk factors (CVRF), the guidelines attempt to provide answers to 2 highly important questions:
- •
Glycemic targets to prevent cardiovascular complications. The continuous relationship between blood glycemic levels and microvascular complications, with no discernible threshold, despite the clear benefit of an HbA1c level < 7.5%, is less clear for macrovascular complications. Despite the strong association between glycemia and macrovascular complications, the studies that have evaluated the effect of tight glycemic control have reported discrepant results in the prevention of cardiovascular events. Thus, some studies concluded that that lowering HbA1c by 1% in the medium-term reduced the relative risk of fatal infarctions by 15%, with no effect on the risk of stroke or all-cause mortality. The benefit was greater in patients with more recent onset of DM, those with the best glycemic control, and those without CVD. In contrast, some data show that glycemic control in the long term is important to reduce macrovascular complications: prolonged follow-ups are required to demonstrate a benefit and early glycemic control is important to prevent irreversible lesions. It is clear that, to prevent microvascular complications, the target should be HbA1c < 7%. It is more difficult to define the target to prevent macrovascular complications, especially in the presence of established CVD. Glycemic targets should be individually tailored: for patients with a recent diagnosis, young persons and those without comorbidities, HbA1c should be between 6% and 6.5%; for the remainder, HbA1c should be < 7%, although this target may be less stringent (7.5%-8%) in elderly patients and those with multiple comorbidities. In all groups, a priority is to prevent hypoglycemic episodes and any other secondary effects.
- •
Choice of glucose-lowering agents. This section discusses very basic concepts, such as the use of a basal-bolus insulin regimen in type 1 DM (T1DM) or metformin as the treatment of choice in T2DM, in the absence of contraindications (glomerular filtration rate < 50 mL/min), without resolving our doubts in clinical practice. The HbA1c obtained with any of these therapeutic options is between 0.5% and 1%, depending mainly on DM duration and the initial HbA1c value. Currently, numerous studies are being conducted to determine the cardiovascular safety profile of the new glucose-lowering agents. The results of SAVOR8 and EXAMINE,9 which evaluated the DPP-4 inhibitors, saxagliptin and alogliptin, respectively, have been presented at a recent ESC congress: although these trials included patients with distinct profiles, there were no differences in mortality or ischemic cardiovascular complications; however, the percentage of admissions for heart failure (HF) was higher in the SAVOR trial.
The specific blood pressure (BP) target for patients with DM has alw a y s ar ouse d contr o v ersy, gi v en that some pr e vious recommendations proposed more stringent control for this group (< 130/80 mmHg) in the absence of conclusive clinical evidence. The current guidelines review the available evidence and recommend BP < 140/85 mmHg, like the 2013 ESC guidelines for arterial hypertension (AHT)10 for diabetic patients.
There are no novelties in pharmacological therapy, except the recommendation not to jointly administer angiotensin-II receptor blockers (ARB-II) and direct renin inhibitors (aliskiren), because this combination has no benefit and has even been shown to increase severe complications. Angiotensin-II receptor blockers and angiotensin-conve rting enzyme inhibitors (ACE-I) are the pharmacological strategy of choice and the guidelines recommend their combination with dihydropyridine calcium channel blockers when more drugs are needed to achieve targets. Neither beta-blockers nor thiazides are mentioned in first-line therapy, due to their potential diabetogenic effect in patients with metabolic syndrome, although there is no evidence of a negative effect in patients with established DM.
DyslipidemiaInsulin resistance in T2DM leads to lower serum levels of highdensity lipoprotein cholesterol (HDLc) and higher triglyceride levels; even though low-density lipoprotein cholesterol (LDLc) values may not be high, it is the small, dense LDL particles that are particularly atherogenic. The therapeutic targets are LDLc < 70 mg/dL in very high risk DM patients (the majority) and < 100 mg/dL for those at high risk.
Statin use is a major therapeutic strategy, despite the risk of de novo DM with high doses, since this risk is balanced against the reduction in cardiovascular complications and mortality. The addition of ezetimibe is recommended only after enhancing treatment with statins, although there is still no evidence of its benefit on morbidity and mortality. The latest studies on fibrates have demonstrated that they reduce the incidence of cardiovascular complications in diabetic patients (with high triglyceride levels and low HCLc values) but do not reduce cardiovascular mortality. The drugs specifically designed to raise HDLc, torcetrapib and dalcetrapib, have shown no cardiovascular benefit, despite 30% increases in HCLc, and the 2 trials with nicotinic acid have failed. Therefore, to increase HCLc, interventions on lifestyle modification (smoking cessation, a healthy heart diet, weight control and exercise) continue to be essential.
Platelet Function (Antiplatelet Therapy)The guidelines review acetylsalicylic acid (AAS), its mechanism of action, and the results of studies on cardiovascular prevention. There is no doubt about its indication in secondary prevention. In contrast, there are no data supporting its use in primary prevention, in which it is only recommended in diabetic patients at high risk (when the 10-year risk of cardiovascular events is > 10%); this recommendation in supported by weak evidence based on expert opinion.
Clopidogrel monotherapy is indicated in patients intolerant to AAS and in those with symptomatic peripheral vascular disease (a recommendation based on a single clinical trial): combined with AAS (low-dose), clopidogrel is indicated in coronary intervention and in ACS for 1 year if the bleeding risk is low. The most novel aspect concerns the new antiplatelet agents (prasugrel and ticagrelor), which are considered superior to clopidogrel in the ACS contexts studied.
Multifactorial ManagementThe guidelines underline the importance not only of glycemic control in diabetic patients but also of a multifactorial approach, with tight control of all associated risk factors. Targets for BP, exercise, smoking, diet, and weight control generally concur with the ESC guidelines on prevention11 and specific guidelines, while LDLc targets differ from those of guidelines on dyslipidemia,12 which consider all diabetic individuals to be at high risk and that the target should be LDLc < 70 mg/dL.
Management of Stable And Unstable Coronary Artery DiseaseOptimal Medical Treatment in Patients With Chronic Coronary Artery Disease and Diabetes MellitusAlthough most of the information has been obtained from analyses of subgroups of patients with DM in large trials, the results show similar efficacy in diabetics and nondiabetics. The updated guidelines repeat well-established pharmacological indications and strategies, such as treatment with an ACE-I/ARB-II + statins + antiplatelet agent; the recommendation for beta-blockers carries less weight, but the document justifies and defends their use, despite their “poor metabolic behavior”; there is no doubt about their benefit after a myocardial infarction. Ivabradine is indicated in some situations.
For glycemic control in ACS, 2 strategies are discussed to improve prognosis; metabolic modulation, though glucose-insulin-potassium (GIP), which has not been shown to reduce morbidity and mortality in randomized studies, and glycemic control, although the target is still not well-defined, since some registries indicate a J-or U-shaped relationship between glycemic control and prognosis, implying that both hypoglycemia and hyperglycemia may be prognostically unfavorable. A reasonable conclusion that can be drawn from studies with intensive insulin therapy is that controlling glycemia in patients with acute myocardial infarction will produce a b enef it if hyperglycemia is significant (> 180 mg/dL). Attempts should be made to achieve normal glucose levels but with less stringent targets adapted to distinct comorbidities.
RevascularizationRevascularization procedures continue to be challenged by the higher atherosclerotic burden of coronary artery disease in diabetic patients, with involvement of a greater number of vessels and more diffuse atherosclerosis. There is a higher rate of restenosis after percutaneous coronary interventions (PCI) and saphenous graft occlusion after coronary artery bypass graft surgery.
The updated guidelines repeat most of the recommendations published in 2010 on myocardial revascularization in diabetic patients. Some more recent evidence has been introduced, mainly concerning the longstanding controversy about surgery and PCI, but the literature is considered to be confusing due to bias in the registries, the development of drug-eluting stents and, apart from the FREEDOM trial, 13 the lack of prospective randomized studies. In general, the document concludes that, although PCI is a potential treatment for patients with less complex lesions, surgery is indicated in most diabetic patients with multivessel disease. Data from recent registries also indicate that outcome is better in DM with surgery than with drug-eluting stents. Based on the FREEDOM trial,13 surgery is considered to be superior to PCI in patients with DM and advanced coronary artery disease. Although the guidelines affirm that this trial represents the real world due to its inclusion of a wide variety of patients, this affirmation is questionable, since the trial only included 10% of the patients initially evaluated and its favorable results, especially in surgical mortality, cannot be extrapolated to all centers. It is concluded that the type of intervention should be decided after discussion with the patient, explaining the risks and benefits of the treatment, and after assessment of individual risk and the results of each particular center.
Heart Failure and Diabetes MellitusThe guidelines underline the high incidence and prevalence of HF among diabetic individuals and the high mortality when both entities coexist. The importance of looking for signs and symptoms in the at-risk population is stressed, as well as the performance of echocardiograms to improve diagnosis. Prevention in based on intervening on the determining factors. The frequent coexistence of hypertension and other novel and independent risk factors during follow-up is stressed; these factors include elevated HbA1c values, the presence of coronary artery disease, retinopathy, nephropathy with proteinuria, and the need for insulin therapy.
The section on therapeutic management contains the specific recommendations for treatment with drugs with demonstrated b enefit. The role of cardiac resynchronization therapy and implantable cardioverter-defibrillators is mentioned, and there is no evidence of differences in patients with or without diabetes. In contrast, although DM per se does not contraindicate cardiac transplantation, this procedure is more likely to be contraindicated in patients with DM and long-term survival is lower in this population.
The impact of glucose-lowering treatment on the progression and outcome of CVD in diabetic patients with HF is unknown, but the registries and trials with a control group continue to consider metformin as the first-line drug in stable patients, alone or combined with other glucose-lowering agents. Thiazolidinediones are not recommended, due to their tendency to cause fluid retention, which may aggravate the clinical picture. The remaining glucose-lowering drugs, including insulin, show no association with cardiovascular mortality, although doubts remain about the use of some sulphonylureas.14 Recent data from the SAVOR trial,8 awaiting more detailed evaluation, indicate an increased admission rate for HF among diabetic patients treated with saxagliptin.
Diabetes Mellitus and Arrhythmias: Atrial Fibrillation and Sudden Cardiac DeathDue to the high prevalence of atrial fibrillation (AF) among diabetic persons, leading to high morbidity and mortality without appropriate treatment, the new guidelines recommend systematic screening. Type 2 diabetes is an embolic risk factor in patients with AF, and anticoagulant therapy is indicated, unless there are contraindications. The update includes the new oral anticoagulants and embolic risk stratification according to the CHA2DS2-VASc classification and bleeding risk stratification according to the HAS-BLEED scale. The economic impact of the incorporation of these new drugs is not mentioned, although it has been widely discussed in the literature from Spain.15
Diabetes mellitus is a risk factor for sudden cardiac death at any age and the risk is greater among women. Fatal events are associated with hypertension and higher BMI. The association with hypoglycemic episodes, the QT-interval, and neuropathy or dysautonomy is unclear. To reduce the incidence of sudden cardiac death, the indication for implantation of an implantable cardioverter defibrillator in patients with ischemic heart disease and ejection fraction (EF) < 35% is the same as in the nondiabetic population. In patients who have already had a myocardial infarction, the indication for beta-blockers has the highest level of evidence in preventing sudden cardiac death.
Peripheral and Cerebrovascular Disease. Retinopathy and NephropathyA different view from that possibly held by cardiologists is offered, but without in-depth evaluation of the physiopathology of microvascular and macrovascular lesions. The information provided is not especially novel but does serve as an update on noncardiac topics related to DM. A positive feature of the guidelines is the summary of current knowledge on DM and its vascular complications, with useful literature references. Also useful are the therapeutic algorithms, the only algorithms contained in the guidelines (treatment of intermittent claudication, critical limb ischemia, and carotid artery disease), as these diseases do not fall within the daily clinical practice of cardiologists; the implementation of these algorithms will be strongly influenced by the neurology, nephrology and vascular surgery departments of each center and their respective protocols.
Macrovascular Lesions. Carotid and lower Extremity Artery DiseaseImportantly, signs of disease and physical examination continue to be of great importance in diagnosis and prognosis, with emphasis on the ankle-brachial index. Both primary and secondary prevention underline lifestyle modification, physical exercise, and risk factor control. Initial medical treatment should include antiplatelet agents and statins. Beta-blockers are not contraindicated in diabetic patients with lower extremity artery disease.
Retinopathy and NephropathyTreatment of microvascular disease, both in primary and in secondary prevention, should start with lifestyle modifications and tight glycemic control. The HbA1c target in T1DM and T2DM is < 7%. In BP control, emphasis is placed on renin-angiotensin-aldosterone blockade in the primary and secondary prevention of kidney disease: the recommende d target for patients with retinopathy or nephropathy is < 140/85 mmHg, as in all diabetic patients, except in the presence of proteinuria, in which case the target is lower (systolic BP < 130 mmHg), if tolerated by the patient. Adequate lipid control (plasma cholesterol and triglyceride control) is included in the prevention of kidney disease; no information is provided on retinopathy. Antiplatelet therapy is not contraindicated in patients with retinopathy because there have been no observations of an increase in bleeding. Erythropoietin therapy in patients with diabetic nephropathy involves monitoring the progression of retinopathy and car dio vascular risk . F inall y, the guidelines describ e the ophthalmological treatments required in severe retinopathy.
Patient-centered CareOne of the most novel features of the updated guidelines is the last section, on patient-centered care, while the 2007 document ended with an economic analysis of the impact of DM. To achieve lifestyle modifications and therapeutic targets, effective patient support programs are required that take account of the patient's social and cultural context so that patients will effectively self-manage their condition. Ideally, multidisciplinary teams would be involved, headed by nursing staff, and using cognitive-behavioral strategies and a motivational interview to improve adherence to a healthy lifestyle and drug therapy.
GAPS AND CONTROVERSIAL ASPECTSIn the previous guidelines, the recommendation to actively look for silent ischemia in all diabetic patients was–quite rightly-highly controversial. The present version takes a step backward (although the figure in the previous version giving rise to the controversy is retained in the introduction and has been expanded by the inclusion of Holter monitoring) and acknowledges that systematic screening for myocardial ischemia is not required and should be reserved for selected patients depending on their risk and the presence of symptoms. In practical terms, this recommendation will avoid thousands of unnecessary stress tests and hundreds of other, more sophisticated procedures, as a result of misleading results in the former.
Nevertheless, several sections of the document mention the importance of silent ischemia and its high prevalence. However, a specif ic section is nee de d, with a detaile d analysis of the physiopathology of this entity and the diagnostic and therapeutic options that can be used when this entity is present.
Also missing is a more complete description of diab etic myocardiopathy, which is only discussed in a paragraph in the section on HF. Equally, there is no in-depth review of cardiac autonomic neuropathy and its influence on the results of diagnostic studies and treatment response.
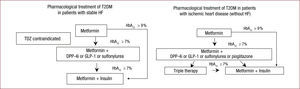
Recommendations on therapy could have included more information on when and how to use glucose-lowering drugs; recommendations on specific treatment in patients during admission and at discharge should have been included, as well as an algorithm for the selection of antidiabetic drugs in patients with HF, such as those designed at the behest of the Diabetes Group of the SEC16–18 (Figure).
Algorithm for pharmacological therapy in T2DM in patients with heart disease. Adapted with permission from Alonso et al.18 GLP-1, glucagon-like peptide 1 receptor agonists; HbA1c, glycated hemoglobin, HF, heart failure, DPP-4i, dipeptidyl peptidase IV inhibitors; T2DM, type 2 diabetes mellitus; TDZ, thiazolidinediones.
Finally, another gap is the lack of economic information on costeffectiveness, both for diagnostic techniques and for the new drugs, mainly antiplatelet agents, anticoagulants and glucose-lowering drugs.
CONCLUSIONSSince the publication of the previous guidelines in 2007, many advances have been made in DM and CVD, leading to the need for an update such as that presented by the ESC and EASD.
Despite the existing evidence and the extremely extensive literature reviewed, there are still many gaps, some of which have been identified by the authors themselves, mainly in targets for glycemic control and the effect of the new drugs.
Most of the recommendations of these guidelines on the diagnosis and treatment of the various CVD in patients with DM were already contained in the previous guidelines of the ESC in the subgroup of diabetics, which is routinely included.
Because the number of diabetics attended by cardiologists in clinical practice is on the increase, more information is needed on the diagnosis and treatment of aspects more specific to DM, which would help professionals specialized in CVD to take decisions on situations with which they are less familiar.
CONFLICTS Of INTERESTF. Arós: fellowship (Instituto Carlos III), educational presentations (Menarini AZ). V. Bertomeu: consulting (Takeda), presentations (Pf izer/BMS, N o v a rtis, Me dtr onic), tr a v el t o congr esses (Daichii-Sankyo). X. Garcia-Moll: consulting (Daichii-Sankyo, Kowa, Menarini, Servier), fellowships (Daichii-Sankyo, Astra-Zeneca, Menarini), presentations (Almirall, Astra-Zeneca, Bayer, Böhringer Ingelheim, Daiichi-Sankyo, Esteve, Menarini, MSD, Novartis, Recordati, Rovi, Servier). J. de la Hera: consulting (Lilly), presentations (AZ Bayer), travel to congresses (Menarini, Bayer). I. Lekuona: presentations and educational presentations (MSD). E. López de Sa: consulting (BMS, Daiichi-Sankyo, Ferrer, Pfizer, Servier), grants (Astra-Zeneca, BMS, Pfizer, Servier), expert witness (Pfizer, Servier), presentations and educational activities (Astra-Zeneca, BMS, Boehringer, Daiichi-Sankyo, Ferrer, Lilly, Pfizer, Servier). P. Mazón: presentations, e ducational activities, travel to congresses (Astra-Zeneca, Bayer, Almirall, Boehringer, MSD, Novartis, Rovi). M. Pedreira: travel to congresses (Bayer, Pfizer). R. Vidal: member of the board, information and communications technology committee of the SEC, travel to congresses (Pfizer). F. Worner: consulting (Daichii-Sankyo), presentations (Daichii-Sankyo, Astra-Zeneca).
Task Force of the SEC for the ESC Guidelines on Diabetes, Prediabetes and Cardiovascular Disease: Pilar Mazón, Isabel Diaz-Buschmann (coordinators), Eduardo Alegría, Alberto Cordero, Elías Delgado, Lorenzo Fácila, Xavier García-Moll, Jesús de la Hera, Nekane Murga and Milagros Pedreira.
Expert Reviewers for the ESC Guidelines on Diab etes, Prediabetes And Cardiovascular Disease: Fernando Arós, Vicente Bertomeu-Martínez, Almudena Castro, Regina Dalmau, Enrique Galve, Iñaki Lekuona, Esteban López de Sa, Juan Quiles and Rafael Vidal-Pérez.
Guideliness Committee of the SEC: Ángel Alonso Gómez, Manuel Anguita Sánchez, Ángel Cequier Fillat, Josep Comín Colet, Isabel Díaz-Buschmann, Ignacio Fernández-Lozano, Antonio Fernández Ortiz, José J. Gómez de Diego, Manuel Pan Alvarez-Osorio and Fernando Worner Diz.
The names of all authors are listed in the Appendix.