Implantable cardioverter-defibrillators reduce mortality in some patients with heart disease. Battery replacement is a frequent occurrence in clinical practice and is required in up to 30% of implants. The benefit/risk ratio of defibrillators varies over time and should be reevaluated at the time of replacement. The aim of this study was to determine the clinical characteristics and incidence of defibrillator therapies in patients who underwent generator replacement.
MethodsThis multicenter retrospective study involved patients from the UMBRELLA national registry who underwent replacement due to defibrillator battery depletion. The incidence of ventricular arrhythmias was determined via remote monitoring. Risk factors for sustained ventricular arrhythmia after replacement were analyzed.
ResultsA total of 354 patients were included (mean age [standard deviation], 61.8 [14.5] years; men, 80%; secondary prevention, 42%; ventricular arrhythmias in the explanted generator, 62%). After a 25-month follow-up, 70 patients (20%) received appropriate therapies and 8 (2.3%) received inappropriate discharges. Male sex, structural heart disease, heart failure, and the absence of resynchronization were independent predictors of ventricular arrhythmia occurrence.
ConclusionsOne-fifth of patients had appropriate defibrillator therapies in the first 2 years after generator replacement. Determination of the factors associated with arrhythmia occurrence after replacement may be useful to optimize implantable cardioverter-defibrillator treatment.
Keywords
Implantable cardioverter-defibrillator (ICD) therapy has reduced overall mortality in numerous clinical trials of heart disease patients at risk of sudden cardiac arrest in both secondary1–3 and primary4–8 prevention. Consequently, ICD use is indicated in clinical practice guidelines,9 and the number of implantations has grown annually in both Europe and the United States.10 However, ICDs are associated with a number of disadvantages, such as inappropriate shocks,11,12 deterioration in the quality of life related to device discharge,13 and a high economic cost.14
Implantable cardioverter-defibrillator replacement is the perfect time to reevaluate the indication of a treatment whose risk/benefit ratio may no longer be favorable.15 Replacement, moreover, carries some risks,16,17 and the complications rate at the surgical wound is double that of the first implantation.18
The number of ICD replacements performed in Spain is growing annually, both in absolute numbers and in proportion to the number of first implants. According to data published in the latest national ICD registries, 950 generator replacements were performed in 2009 (24.4% of all ICD implants),19 which increased to 1135 (26.12%) in 201020 and 1253 (29.8%) in 2011.21
Although generator replacement increases health care activity and costs, few data have been published on the performance of ICD therapy in this population. The present study aimed to determine the clinical profile of patients undergoing ICD generator replacement in Spain, the incidence of this treatment in this population, and the factors associated with the occurrence of sustained ventricular arrhythmias after replacement.
METHODSThis study was conducted within the framework for observational research provided by the Scientific Cooperation Platform (SCOOP). This platform is based on the UMBRELLA national registry (incidence of arrhythmias in the Spanish population with a Medtronic ICD), registered at ClinicalTrials.gov as NCT01561144. This voluntary registry, promoted by Medtronic, includes patients in both primary and secondary prevention implanted with a Medtronic ICD with remote monitoring (CareLink). Of the 72 Spanish centers CareLink systems have been implanted, 44 voluntarily participated. At the time of writing, 1661 patients had been enrolled in the study. Patient participation was approved by the ethics committees of the participating centers and all patients provided informed consent.
The study population consisted of all patients included in the UMBRELLA registry upon undergoing ICD generator replacement due to battery depletion. We excluded replacements made for other reasons, such as infection or system updating.
The prevalence of sustained ventricular arrhythmias at the time of replacement was obtained via a questionnaire completed by the treating physician. Patient follow-up was systematically performed using remote monitoring. Sustained ventricular arrhythmias were considered to be those that provoked an appropriate ICD therapy. Patients with Brugada syndrome, long QT syndrome, or idiopathic ventricular fibrillation were considered to be “without structural heart disease”.
A committee consisting of 6 experts studied the incidence of ventricular arrhythmia following replacement by analyzing the electrograms of the events stored in the CareLink network. Each event was reviewed in a double-blind manner by 2 committee members, who classified the type of arrhythmia and the effectiveness of the therapy. If there was disagreement, the event was referred to a third reviewer. If no agreement was reached between 2 of the 3 reviewers, the event was reassigned to a new pair of reviewers and, if necessary, to a sixth reviewer. If there was still no consensus between 2 of the 3 reviewers, the event was classified in a joint meeting of all the committee members.
Continuous variables are expressed as mean (standard deviation [interval]) and/or [interquartile range] and discrete variables are expressed as proportions. Continuous variables were compared using the Student t test for independent samples or a 1-way analysis of variance, after confirmation of the normality of the distribution. Binary logistic regression was used to calculate the risk factors for the occurrence of appropriate therapies. First, a univariate analysis was performed with each of the variables analyzed in the study. Next, a multivariate model was constructed using those variables with P < .20 in the univariate analysis. Data analysis was performed with the IBM SPSS Statistics software package, version 20. P values < .05 were considered significant.
RESULTSPatient CharacteristicsA total of 354 patients who underwent ICD generator replacement due to battery depletion between January 2007 and November 2012 were included in this study.
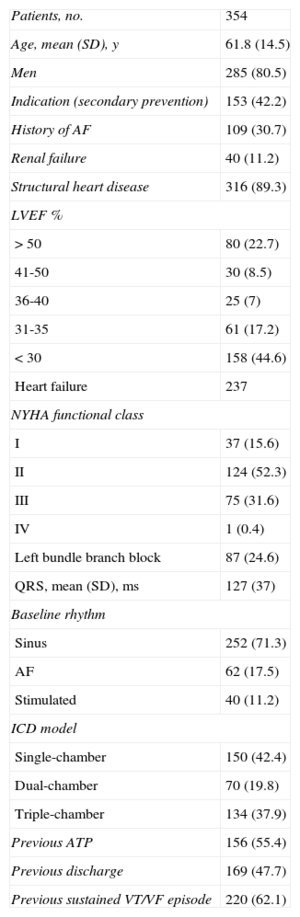
The mean patient age was 61.8 (14.5 [53-73]) years. Of the 354 patients, 62% had sustained ventricular arrhythmias at the time of generator replacement. The clinical characteristics and device type are summarized in Table 1.
Clinical Characteristics of Patients Undergoing Generator Replacement
| Patients, no. | 354 |
| Age, mean (SD), y | 61.8 (14.5) |
| Men | 285 (80.5) |
| Indication (secondary prevention) | 153 (42.2) |
| History of AF | 109 (30.7) |
| Renal failure | 40 (11.2) |
| Structural heart disease | 316 (89.3) |
| LVEF % | |
| > 50 | 80 (22.7) |
| 41-50 | 30 (8.5) |
| 36-40 | 25 (7) |
| 31-35 | 61 (17.2) |
| < 30 | 158 (44.6) |
| Heart failure | 237 |
| NYHA functional class | |
| I | 37 (15.6) |
| II | 124 (52.3) |
| III | 75 (31.6) |
| IV | 1 (0.4) |
| Left bundle branch block | 87 (24.6) |
| QRS, mean (SD), ms | 127 (37) |
| Baseline rhythm | |
| Sinus | 252 (71.3) |
| AF | 62 (17.5) |
| Stimulated | 40 (11.2) |
| ICD model | |
| Single-chamber | 150 (42.4) |
| Dual-chamber | 70 (19.8) |
| Triple-chamber | 134 (37.9) |
| Previous ATP | 156 (55.4) |
| Previous discharge | 169 (47.7) |
| Previous sustained VT/VF episode | 220 (62.1) |
AF, atrial fibrillation; ATP, antitachycardia pacing; ICD, implantable cardioverter-defibrillator; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association; SD, standard deviation; VF, ventricular fibrillation; VT, ventricular tachycardia.
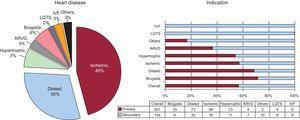
The predominant underlying heart disease was ischemia (46.5%), and 9.5% of the patients had no structural heart disease. The proportion of patients in secondary prevention varied by heart disease, from 25% of patients with Brugada syndrome to 100% of patients with long QT syndrome or idiopathic ventricular fibrillation. The types of heart disease and corresponding indications are shown in Figure 1.
The chart on the left shows the distribution of heart disease types in patients who underwent replacement of implantable cardioverter-defibrillator generators. The graph and table on the right show the proportion of the type of indication, both in general and for each type of heart disease. ARVD, arrhythmogenic right ventricular dysplasia; IVF, idiopathic ventricular fibrillation; LQTS, long QT syndrome.
The mean lifespan of the generators replaced was 5.6 (1.9) years. Device type was the only factor independently correlated with generator lifespan. The lifespan of single-chamber ICDs was 6.6 (1.9) years, whereas those of dual-chamber ICDs and ICDs with cardiac resynchronization therapy (CRT) were 5.8 (1.5) years and 4.4 (1.1) years (P < .001), respectively. Therapy history (bursts or discharges) in the explanted generators had no effect on battery lifespan.
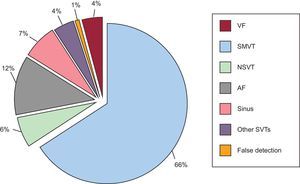
Incidence of Ventricular ArrhythmiasAfter a mean follow-up of 25 (18) months, 1340 stored events were recorded as ventricular arrhythmias in 11 patients (31%). Event analysis concluded that 937 of the 1340 events (70%) were sustained ventricular arrhythmias and that the other events were nonsustained ventricular arrhythmias, supraventricular arrhythmias, or false detection (due to noise or T wave oversensing). The types of events following electrogram-based classification are shown in Figure 2.
Events detected during the follow-up of patients after generator replacement according to the expert committee. AF, atrial fibrillation; NSVT, nonsustained ventricular tachycardia; SMVT, sustained monomorphic ventricular tachycardia; SVTs, supraventricular tachycardias; VF, ventricular fibrillation.
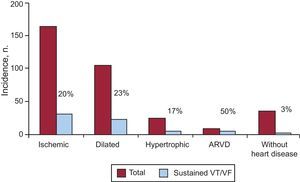
Events corresponding to sustained ventricular arrhythmias were recorded in 70 of the 354 patients (20%; 95% confidence interval, 15.3%-23.7%). Discharges were appropriate in 39 patients (11%) and were inappropriate in 8 patients (2.3%; 95% confidence interval, 0.8%-3.7%). The type of heart disease that proportionally showed the highest number of sustained events was arrhythmogenic right ventricular dysplasia. Patients without structural heart disease had a lower incidence of appropriate ICD therapies (2.6%). The incidence of sustained ventricular arrhythmias by heart disease type is shown in Figure 3. The time from generator replacement to the first appropriate ICD discharge was 14.5 (13.5 [0.2-51.9]) months. Each patient had a mean of 4 (0-322) antitachycardia pacings and 0.4 (0-13) shocks during follow-up.
Comparison of the incidence of sustained ventricular arrhythmia by heart disease type. Each pair of columns shows the total number of patients and the number of patients with events. ARVD, arrhythmogenic right ventricular dysplasia; VF, ventricular fibrillation; VT, ventricular tachycardia.
There were no sustained ventricular arrhythmias before replacement or during follow-up in 113 patients (32%). At the time of replacement, 19 of these patients were > 75 years (17% of the total) and 6 were > 80 years (5% of the total). Of these, 72% had a primary prevention indication.
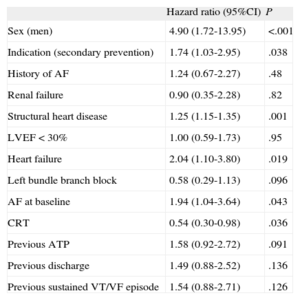
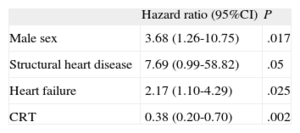
Univariate analysis of the factors associated with the occurrence of sustained ventricular arrhythmias after ICD replacement is shown in Table 2. In multivariate analysis, only male sex, structural heart disease, and heart failure were associated with a higher incidence of ventricular arrhythmias, while CRT acted as a protective factor against this type of arrhythmia (Table 3). Detection of ventricular arrhythmias or discharges in the explanted ICD showed a nonsignificant tendency to predict ventricular arrhythmias after replacement. No significant differences were detected in the occurrence of sustained ventricular arrhythmias based on ejection fraction in the overall patient population or in the subgroup of 269 patients with ischemic heart disease or dilated heart muscle disease.
Univariate Analysis for Estimating the Risk of the Occurrence of Sustained Ventricular Arrhythmias From a Selection of Study Variables
| Hazard ratio (95%CI) | P | |
| Sex (men) | 4.90 (1.72-13.95) | <.001 |
| Indication (secondary prevention) | 1.74 (1.03-2.95) | .038 |
| History of AF | 1.24 (0.67-2.27) | .48 |
| Renal failure | 0.90 (0.35-2.28) | .82 |
| Structural heart disease | 1.25 (1.15-1.35) | .001 |
| LVEF < 30% | 1.00 (0.59-1.73) | .95 |
| Heart failure | 2.04 (1.10-3.80) | .019 |
| Left bundle branch block | 0.58 (0.29-1.13) | .096 |
| AF at baseline | 1.94 (1.04-3.64) | .043 |
| CRT | 0.54 (0.30-0.98) | .036 |
| Previous ATP | 1.58 (0.92-2.72) | .091 |
| Previous discharge | 1.49 (0.88-2.52) | .136 |
| Previous sustained VT/VF episode | 1.54 (0.88-2.71) | .126 |
95%CI, 95% confidence interval; AF, atrial fibrillation; ATP, antitachycardia pacing; CRT, cardiac resynchronization therapy; HR, hazard ratio; LVEF, left ventricular ejection fraction; VF, ventricular fibrillation; VT, ventricular tachycardia.
Multivariate Analysis for Estimating the Risk of the Occurrence of Sustained Ventricular Arrhythmias
| Hazard ratio (95%CI) | P | |
| Male sex | 3.68 (1.26-10.75) | .017 |
| Structural heart disease | 7.69 (0.99-58.82) | .05 |
| Heart failure | 2.17 (1.10-4.29) | .025 |
| CRT | 0.38 (0.20-0.70) | .002 |
95%CI, 95% confidence interval; CRT, cardiac resynchronization therapy.
Only statistically significant predictors are shown.
Implantable cardioverter-defibrillator generator replacements are systematically performed in most centers. Typically, patients are sent to undergo ICD replacement from device consultation in a largely automated manner once battery depletion is seen, which can lead to a lack of attention to this process. Replacement of ICDs is as important a clinical decision as the decision to implant the first device and requires an individualized reevaluation of patient status and therapy indication.
The results of the present study provide novel data on the characteristics of patients who undergo ICD replacement in Spain, the performance of the explanted devices, and the incidence of ventricular arrhythmias after replacement.
The main findings of the study are as follows: a) the prevalence of sustained ventricular arrhythmia detected by the explanted ICD was 62%; b) the cumulative incidence of sustained ventricular arrhythmia at the 2-year follow-up was 20%; c) the cumulative incidence of inappropriate discharges in this period was 2.3%, and d) the independent predictors of the occurrence of sustained ventricular arrhythmia were male sex, structural heart disease, heart failure, and absence of CRT.
Age of Patients Undergoing Generator ReplacementThe age of the study patients (61.8 [14.5] years) was similar to that found in national ICD registries. The mean age of patients with a first implantation or replacement was 62.5 (13.4) years according to the 2011 registry and was 61.7 (13.6) years in the case of first implants (the age of patients who underwent replacement was not specified).21 Although ICD therapy is effective for the treatment of ventricular arrhythmias in all age groups, its impact on mortality is reduced and the clinical benefit is lower in patients > 75 years (19% of the patients in this study).22
Incidence of Therapies After ReplacementThe series of the Leiden group, which included patients with ICDs in primary and secondary prevention, showed a cumulative incidence of appropriate therapies at 1 year and 3 years of 18% and 33%, respectively, whereas the incidence of inappropriate discharges at 1 year and 3 years was 7% and 13%, respectively.23 The incidence of appropriate shocks after generator replacement was similar in this study, but the incidence of inappropriate discharges was clearly lower. The low incidence of inappropriate discharges after replacement can be explained by adjustments in the programming and/or antiarrhythmic treatment to prevent this type of therapy during the follow-up performed before generator replacement.
The cumulative 2-year incidence of appropriate therapies in our patients was lower than the approximately 30% noted in the German INSURE registry series of patients with ICD generator replacement, which was the other large series published to date. No data have been published on the incidence of inappropriate therapies in this registry.24 Possible explanations for the different incidences of appropriate therapies are that the overwhelming majority of patients studied in the INSURE registry were in secondary prevention and that CRT patients were excluded.
Predictors of the Occurrence of Ventricular Arrhythmias During Follow-upThe higher incidence of appropriate therapies found in patients with heart failure and structural heart disease is in agreement with the current available evidence on the general population of patients with ICDs.25
The correlation between a history of ventricular arrhythmias in the explanted ICD and the incidence of ventricular arrhythmias is more controversial. Although this history was a risk factor in the INSURE study,24 in the series of Van Welsenes et al26 the absence of events after the useful life of an ICD generator failed to predict the absence of events after ICD replacement in primary prevention patients with idiopathic or ischemia-related dysfunction of the left ventricle. In our series, there was no statistically significant correlation between the incidence of appropriate therapies and the history of ventricular arrhythmias in the replaced ICD and therefore this association may be only produced or produced with greater strength in secondary prevention patients.
The protective effect of CRT in reducing ICD therapies found in patients after replacement contrasts with the neutral effect in this regard published in a substudy of patients of the Contak-CD and InSync-ICD clinical trials.27 The general neutral effect of CRT is explained by a heterogeneous response: whereas in some patients CRT had a proarrhythmic effect due to repolarization dispersion produced by epicardial pacing,28 in others, a reduction was seen in the appropriate ICD therapies that was associated with reverse remodeling of the left ventricle.29,30 Survival until generator replacement is required probably selects in some way for responsive patients and those cases of proarrhythmia associated with CRT were excluded, which explains the net favorable effect in this group.
This study is the first to uncover the protective role of female sex in the postgenerator replacement population. A substudy of the MADIT-II trial showed a lower incidence of ventricular arrhythmias in women,31 although these data have not been confirmed in other studies.32,33 Women with ventricular dysfunction respond better than men to drug treatment with beta-blockers34 and angiotensin inhibitors35 and to CRT,36 which could translate into a beneficial reduction in the incidence of ventricular arrhythmias at the time of replacement.
Decision on implantable cardioverter-defibrillator Generator Replacement Following Battery DepletionOnce the need for ICD battery depletion approaches, the patient's life expectancy and attitude to the possibility of cardiac arrest may have changed since the first implant, particularly in very elderly patients and/or those with serious comorbidities. For those with primary prevention indications that have not received appropriate therapies during the useful life of the defibrillator, these considerations gain importance. The recommendations of the European consensus document on the management of implantable devices in terminally ill patients clearly state that deactivating or neglecting to replace a defibrillator is not considered a form of euthanasia.37 Thus, this option should be considered in certain patients. So far, it is unknown what proportion of patients with ICD battery depletion does not undergo generator replacement, the reason for treatment interruption, and the clinical course of this type of patient, which could be objectives of future studies.
LimitationsThis registry was based on a preformatted data collection sheet, which precluded the identification of other clinical data of interest when evaluating ICD prognosis and indication, such as the presence of degenerative diseases, cancer, end-stage renal failure, etc.
The presence of sustained ventricular arrhythmias may be overestimated by considering them to be incidences of ventricular tachycardia interrupted by overdrive pacing, as a proportion of these events could correspond to self-limiting ventricular arrhythmias.
Extrapolation of the data to other brands should be performed with caution because the data were obtained from patients fitted with an ICD from only 1 manufacturer. This caveat is particularly important when referring to device lifespan because lifespan is already known to vary among devices made by distinct manufacturers.38 The reduced number of patients without structural heart disease or with right ventricular dysplasia in the series should be remembered when interpreting ICD performance in this group of patients.
CONCLUSIONSMost patients who undergo generator replacement in Spain have had sustained ventricular arrhythmias at the time of replacement. One-fifth of patients who undergo generator replacement have appropriate therapies after 2 years of follow-up. Whereas the incidence of appropriate therapies is almost identical to that of the general population of patients with ICDs, the incidence of inappropriate discharges after replacement is lower. Predictors of the occurrence of sustained ventricular arrhythmia after replacement are male sex, structural heart disease, heart failure, and the absence of CRT.
The results of this study may be useful for optimizing therapy performance and understanding the clinical benefits of ICD replacement, which could help decisions be made about whether ICD generator replacement should be performed in specific patients.
CONFLICTS OF INTERESTSDr. Fontenla has received fees for consulting work and Medtronic has facilitated his attendance at medical conferences.