Keywords
INTRODUCTION
Several factors have been reported as influencing the maintenance of sinus rhythm (SR) in the long term after electrical cardioversion (EC) for persistent atrial fibrillation (AF). One of the factors most associated with this is the use of antiarrhythmic drugs.1-10
However, there are few data on the predictors of long-term maintenance of SR in patients without structural heart disease, or the benefit of prophylactic antiarrhythmic drugs in this type of patient.
The aim of the REVERSE (REgistro sobre la cardioVERSión en España) study was to investigate the clinical effectiveness of electrical cardioversion in AF, since no sufficiently large and specific multicenter registries were available that described their use in daily clinical practice.
The aim of the present analysis was to investigate the clinical effectiveness of using antiarrhythmic treatment in the maintenance of SR during the first year after successful EC for persistent AF in patients without structural heart disease.
METHODS
The REVERSE11 registry prospectively included all the patients with persistent AF referred to elective EC in 96 Spanish hospitals between February 1, 2004 and June 30, 2004. Patients without structural heart disease underwent clinical and electrocardiographic follow-up for 1 year. A sample of hospitals from each region was selected which was proportional to their demographic weight. The selection was also representative of all levels of clinical care. The inclusion criteria were as follows: a) age ≥18 years; b) AF for at least 7 days; and c) no precipitating causes (hyperthyroidism, fever, pericarditis, etc). The registry included 1515 patients of which 1355 underwent EC and was successful in 1175 (87%) patients.12 Of these, 528 (45%) were considered to not have structural heart disease and follow-up was conducted during 1 year. The latter group was the one studied in the present analysis. Data were recorded on clinical characteristics, treatment, AF characteristics, EC, and echocardiogram. An echocardiogram performed within the 6 months prior to EC was required. The patient was considered to have structural heart disease when presenting some of the following abnormalities: moderate or severe valvular heart disease or mitral stenosis of any degree; myocardial infarction; cardiomyopathy; hypertensive heart disease (hypertension and posterior wall or septal thickness >13 mm); systolic dysfunction (EF <50%). Atrial fibrillation was considered isolated when the patient was less than 60 years and did not have lung disease, hypertension, or left ventricular hypertrophy.13 No specific treatment or management procedure was recommended. Follow-up was conducted at 1 month, 3 months, 6 months, and 12 months. A total of 98% of patients were followed up at 1 month, 98% at 3 months, 97% at 6 months, and 97% at 12 months. A total of 94% completed all follow-up assessments.
Discrete variables were compared using the c2 test and continuous variables compared using the Student t test. Kaplan-Meier curves were constructed to describe the effect of antiarrhythmic treatment on the recurrence of persistent AF (duration ≥7 days) during the first year and logarithmic ranges were compared to assess between-group differences. A Cox proportional hazards model was used in the multivariate analysis to assess whether the absence of antiarrhythmic treatment was associated with the recurrence of persistent AF. The linearity and proportionality of the variables introduced in the model were assessed as required. The following factors were included in the analysis: weight, age, sex, hypertension, left atrial dilatation (≥50 mm), antiarrhythmic treatment at discharge, treatment with angiotensin-converting enzyme (ACE) inhibitors or angiotensin II-receptor antagonists (ARA-II), and duration of AF >1 year. Possible interactions between the variables of the model were analyzed.
A P value less than .05 was considered significant. All analyses were performed using the SPSS 14.0 statistical software package.
RESULTS
The clinical characteristics of the 528 patients studied are summarized in Table 1. A total of 80% of the patients were receiving prophylactic antiarrhythmic treatment at discharge, the most frequently used drug being amiodarone (68% of the patients treated) (Table 2). Some 42% were treated with ACE inhibitors or ARA-II. No variable (duration of AF, previous cardioversion, sex, age, isolated AF) was associated with greater use of antiarrhythmic drugs. A high percentage of the patients who remained in SR at each follow-up assessment were still taking antiarrhythmic drugs (80% at 1 month, 89% at 3 months, 88% at 6 months, and 95% at 12 months), as antiarrhythmics were still being administered after 1-year follow-up in 59% of patients who remained in SR at all assessments.
At 1-year follow-up, 260 (51%) patients remained in SR. Of these patients, 191 (37%) remained in SR at all assessments and without identified episodes of persistent AF. Most recurrences (64%) occurred in the first month after EC. Of the 337 patients who had recurrences of persistent AF during follow-up, 41 (12%) reverted to SR using antiarrhythmic drugs, 89 (26%) underwent a new EC during the year of follow-up, and 25 (7%) were managed using non-pharmacological methods (ablation or pacemaker implantation).
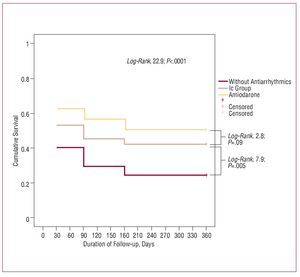
Table 3 describes the effect of antiarrhythmic treatment between each assessment on the prevention of AF recurrence in patients who remained in SR. Antiarrhythmic treatment was associated with a significantly lower percentage of recurrences of persistent AF between discharge and the third month; between the third and sixth month there was a tendency in favor of antiarrhythmic treatment. Antiarrhythmic treatment tended to be changed more frequently when patients were being treated at discharge with flecainide or propafenone (Vaughan-Williams Ic group drugs) than when they were being treated with amiodarone (14% with the Ic group drugs vs 8% with amiodarone; P=.07). The main reason was the ineffectiveness of the treatment (13% with the Ic group drugs and 5% with amiodarone) followed by onset of adverse drug reactions (3% with amiodarone and 0.9% with the Ic group drugs). Figure shows the Kaplan-Meier curve for recurrence of persistent AF during the first year in relation to antiarrhythmic treatment at discharge (amiodarone, Ic group drugs or without treatment); significant differences can be observed between the 3 groups (log-rank test, 22.9; P<.001). The group treated with amiodarone had the lowest percentage of recurrences. Analysis of the differences between the group treated with amiodarone and the group treated with Ic group antiarrhythmics showed that amiodarone tended to be significantly better (log-rank test, 2.8; P=.09). On the other hand, fewer recurrences were recorded in the group treated with Ic group antiarrhythmics than in the group without treatment (log-rank test, 7.9; P=0.005). Multivariate Cox regression analysis identified no antiarrhythmic treatment at discharge (hazard ratio [HR] = 1.59; P=.001) and weight (HR per each kilogram = 1.01; P=.04) as being independently associated with the recurrence of persistent AF during the first year, adjusted by age, sex, hypertension, presence of left atrial dilatation (≥50 mm), treatment with ACE inhibitors or ARA-II, and duration of AF >1 year. No significant interaction was found between the variables of the model.
Figure. Kaplan-Meier curve for recurrence of persistent atrial fibrillation during the first year in relation to antiarrhythmic treatment at discharge.
DISCUSSION
We found that in routine clinical practice in Spain, after successful EC, most patients without structural heart disease receive antiarrhythmic drugs at discharge, especially amiodarone, and this is maintained in more than half of the patients who remain in SR at 1 year. Antiarrhythmic treatment at discharge was the most relevant prognostic factor of those associated with the maintenance of SR during the first year, and had its maximum effect 3-6 months after EC. Amiodarone tended to be better than the other antiarrhythmic drugs.
Although many published studies have analyzed the usefulness of antiarrhythmic treatment after EC, none have specifically focused on patients with persistent AF but without structural heart disease. These studies regularly report the use of antiarrhythmic drugs as a predictor of maintaining SR.3-10 Although different antiarrhythmic drugs, such as sotalol, flecainide, and propafenone, have demonstrated their usefulness, amiodarone is probably the most studied drug and has demonstrated better results.6-10 The SAFE-T8 trial included 665 patients and is the largest study published to date which compared the benefit of antiarrhythmic drugs before and after EC for persistent AF. Amiodarone was better than sotalol—and sotalol was superior to placebo—in the maintenance of long-term SR. The REVERSE registry confirmed that amiodarone is the most frequently used drug after EC in Spain and it seems to be better than other antiarrhythmic drugs in patients without structural heart disease. An aspect on which there is no consensus in the literature is the duration of antiarrhythmic treatment after EC. Some recent studies have reported benefits from maintaining treatment with amiodarone for 3-6 months. The SAFE-T showed benefit of treatment when this was maintained in the long term (1-4 years) after EC. The REVERSE registry showed that, in Spain, long-term antiarrhythmic treatment is frequently maintained in patients without heart disease, and is continued in more than half of the patients who remain in SR at 1 year. On the other hand, we can infer that antiarrhythmic treatment in the prevention of recurrence of persistent AF in these patients is especially useful in the first 3 months and can be effective in the first 6 months after EC.
Some differences exist between the use of prophylactic antiarrhythmic drugs in clinical practice in Spain and the recommendations summarized in the recent update on AF in clinical practice from the ESC/AHA/ACC.14 The guideline proposes the optional use of antiarrhythmic drugs at discharge after EC, since these are considered more useful in patients with heart disease and proposes their use in patients with previous EC or early recurrence. In Spain, we have found that the use of antiarrhythmic drugs after EC is routine practice, regardless of the presence of heart disease or previous EC. Although the guideline makes no explicit reference to the type of antiarrhythmic drug of choice in the section on cardioversion, the section on pharmacological treatment recommends amiodarone as a second-line drug for the maintenance of SR in most cases, especially when structural heart disease is absent. Our study confirms that amiodarone is the most frequently used drug and seems to be better than the other antiarrhythmic drugs in reducing the recurrence of persistent AF, even in patients without structural heart disease. With regard to the duration of treatment, the guideline advises against maintaining prolonged antiarrhythmic treatment after EC, whereas we found that in Spain this is maintained in half of the patients who remain in SR at 1 year, although its maximum effect was found to be in the first 3-6 months after EC.
The SR maintenance rate during the first year (37%) is similar to that reported by previous studies which included patients with and without heart disease. In addition to the use of antiarrhythmic drugs, our study showed that the risk of recurrence of AF was related to weight, a variable that had not been previously described as a predictor of recurrence, probably because many of the previous studies had not included this in the analyses. This effect may be due to a relatively lower dose of antiarrhythmic drugs given to heavier patients or to the effect itself of obesity and additional comorbidity.
The fact that other predictors of recurrence were not identified does not invalidate the usefulness of other predictors previously described in other populations. These results should be set in the context of a group of patients without structural heart disease and the influence of previous studies on the selection of patients who were candidates for CE.11 In our study, there was a very low percentage of patients with long-term AF and left atrial dilatation, and thus these variables are unlikely to have statistical relevance in predicting the recurrence of persistent AF.
We also draw attention to the fact that a second EC within the first year is not uncommon and of the limited use of non-pharmacological treatment (pacemaker or ablation). Although the ESC/AHA/ACC guidelines state that later EC is of little use except in very symptomatic patients, more than a quarter of patients with recurrence underwent a new EC. It can be inferred that rhythm control strategies are employed fairly frequently and that a non-negligible percentage of patients have symptomatic AF that is difficult to control. Although the rhythm control strategy seems to have declined in popularity following the AFFIRM and RACE studies, no evidence exists that indicates their conclusions can be extrapolated to a population without structural heart disease, given the inclusion of a high percentage of patients with heart disease (around 80%).
CONCLUSIONS
In routine clinical practice, after successful EC for persistent AF in patients without structural heart disease, the great majority of patients receive antiarrhythmic drugs, especially amiodarone. In this population, the use of antiarrhythmic drugs, especially amiodarone, is the main factor associated with the maintenance of sinus rhythm at 1 year.
The REVERSE registry was financed by 3M pharmaceutical and endorsed by the Arrhythmia Section of the Spanish Society of Cardiology.
ABBREVIATIONS
AF: atrial fibrillation
EC: electrical cardioversion
SR: sinus rhythm
Correspondence: Dr. J.M. Alegret.
Hospital Universitari de Sant Joan de Reus. Sant Joan, s/n. 43201 Reus. Tarragona. España.
E-mail: txalegret@hotmail.com
Received December 13, 2007.
Accepted for publication July 22, 2008.