Keywords
INTRODUCTION
Evaluation of patients with chest pain is one of the biggest challenges facing physicians who work in emergency departments. This complaint accounts for between 5% and 20% of all admissions to the emergency department and it is estimated that one emergency for chest pain is attended for every 1000 inhabitants covered by a referral hospital.1 Management of chest pain in emergency departments is not standardized as physicians of differing levels of training work in such hospitals (residents, general physicians, specialists). This can give rise to problems in clinical practice. In recent years, chest pain units (CPUs) have become increasingly common in different hospitals throughout Spain, either with their own beds, or based on virtual management of chest pain using computer programs. However, given that the number of recommended beds for a CPU is only 1-2/50 000 emergencies/year,1 the percentage of patients who present in the emergency department with chest pain and who are finally assessed in a CPU (real or virtual) is low.
Traditionally, risk stratification in the CPU of patients with low-intermediate risk is based on the findings of tests for detecting ischemia; patients with positive tests are admitted and those with negative tests or those with results suggestive of low risk are discharged.2,3 Recently, we and other authors have reported the usefulness of clinical variables grouped into indexes to stratify risk in CPUs.4-8 Given that these indexes allow patients of both very low and very high risk to be identified, they may be of assistance for identifying patients who should not be admitted to the CPU because direct discharge or discharge to the general ward would be more beneficial.
The objectives of this study were, on the one hand, to characterize the population of patients who present with nontraumatic chest pain in the emergency department of a tertiary hospital. On the other hand, we wished to assess the usefulness of the CPU-65 index (comorbid, diabetes, typical pain, use of aspirin, and age 65 years or more)4,8 for stratifying the short-term risk of these patients.
METHODS
The family physicians prospectively recorded all patients aged 17 years or over with nontraumatic chest pain who attended the emergency department of our center between March 1 and May 31, 2003. It is important to highlight that there was no CPU or specific program for attending to patients with chest pain in place in our hospital at that time. Likewise, during this period, patient flow, their location, and the diagnostic tests performed were those normally used in our hospital at the time. Investigators did not intervene in organizing the management of patients with chest pain until the data collection period of the study was complete. Admission of the patient to the cardiology ward or to a coronary unit was decided on an individual basis by the physician on duty in the cardiology ward. Admissions to other services were decided by the physicians in the emergency department. Chest pain was classified as typical when explicitly indicated by the physician in the emergency department or similar expressions were used (such as chest pain of likely coronary origin). Chest pain was classified as atypical when the physician in the emergency department explicitly indicated this diagnosis or when he or she used similar expressions (such as mechanical chest pain). Chest pain was classed as undefined when it did not meet either of the previous conditions. The diagnostic tests used in the emergency department, the time during which the patients were seen, and the final destination of each patient were recorded. Acute myocardial infarction was diagnosed using the definition of the European Society of Cardiology/American College of Cardiology published in 2000.9 For cases in which troponin was not measured, the biochemical marker used for diagnosis of myocardial infarction was creatine phosphokinase.
Statistical Methods
For group comparisons, the c2 test was used (or the Fisher exact test if appropriate) for categoric variables and the Student t test or analysis of variance for tendencies of continuous variables after checking that the distributions were normal. The SPSS statistical analysis program, version 11.0 for Windows (SPSS Inc., Chicago, Illinois, USA) was used.
RESULTS
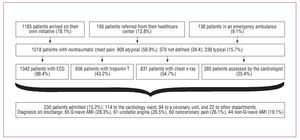
In 3 months, 1518 patients were admitted to the emergency department with nontraumatic chest pain, that is, 6.1% of the medical emergencies and 3.2% of all emergencies. The daily mean number of patients with nontraumatic chest pain was 16.5. Bearing in mind the population of the area covered by our hospital (650 000 inhabitants), 0.8 admissions per month were made for every 1000 inhabitants. The clinical characteristics of the patients and their variation with score on the CPU-65 index are summarized in Table 1 and the patient flow is summarized in Figure 1.
Figure 1. Flow diagram of the 1518 patients with nontraumatic chest pain who attended the emergency room of our hospital during the study period. AMI: acute myocardial infarction.
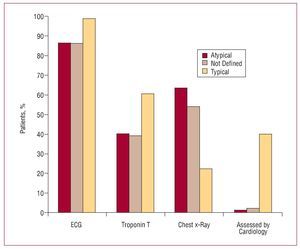
The scores on the Geleijuse scale10 (Appendix) of the patients with atypical, undefined, and typical chest pain were 3.5 (3.8), 4.6 (3.7), and 9.3 (2.7), respectively (P<.001). The frequency with which tests were carried out and assessment by the cardiology duty physician also varied according to the type of chest pain (Figure 2). The ECG data are summarized in Table 2.
Figure 2. Complementary tests performed and assessment by the duty cardiologist according to type of chest pain.
Reperfusion treatment was undertaken in 47 patients (3.1%)—28 procedures corresponded to primary angioplasty and 19 to fibrinolysis. Seven patients died while in hospital (3% of those admitted and 0.5% of all patients), in 6 cases due to cardiac causes (3 cardiogenic shock, 1 cardiac rupture, 1 asystole during percutaneous coronary intervention, and 1 arrhythmic storm), and 1 due to a noncardiac cause (lymphoma).
In total, the emergency department discharged 1288 patients (84.8%), 1271 with the primary diagnosis shown in Table 3. Seventeen were discharged with the diagnosis of "no urgent disease." The most common diagnosis was atypical chest pain, followed by respiratory infection, including 25 patients (2%) with pneumonia.
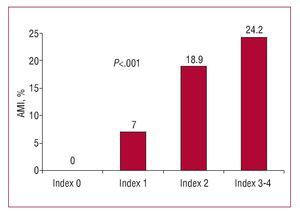
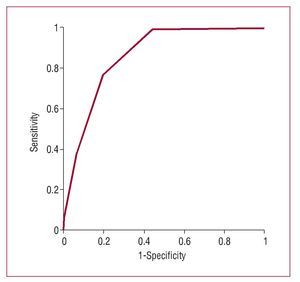
The distribution of scores on the UDT-65 risk index is shown in Table 1. This index was associated with acute myocardial infarction (Figure 3). No patient with a score of 0 on the index died while admitted and the rate of inhospital mortality increased with increasing index scores (index score 1, 1 patient [0.3%]; index score 2, 3 patients [1.2%]; index scores 3-4, 3 patients [2%]). The discriminatory power of the scoring to predict patients with final diagnosis of ischemic heart disease had an area under the receiver operator characteristics curve of 0.87 (Figure 4). The specificity, sensitivity, and positive and negative predictive values for different cutoffs are shown in Table 4.
Figure 3. Prevalence of acute myocardial infarction (AMI) according to CPU-65 index (comorbid diabetes, typical pain, use of aspirin, and age 65 years or more).
Figure 4. ROC curve for the CPU-65 index (comorbid diabetes, typical pain, use of aspirin, and age 65 years or more) for final diagnosis of ischemic heart disease
DISCUSSION
In our study, we found that patients who present in the emergency department with chest pain represent an enormous healthcare burden, and this confirms previous findings (approximately 1 admission to the emergency department/month per 1000 inhabitants).1 Although the risk factors and a history of cardiovascular disease are common, half the patients have a profile of low risk, and so they might not benefit from being assessed in a CPU.
Recently, we have described the CPU-65 index, which is associated with the prevalence of coronary artery disease and with the prognosis of patients assessed in the CPU.4 Since that publication, Sanchís et al5,6 have found similar index scores in a CPU in which detection of ischemia is performed by exercise testing only. If we limit ourselves to patients with normal or nondiagnostic ECG,5 the index published by that group is very similar to ours, with coincident points such as diabetes, type of pain, and age. These authors did not include aspirin use, which they "replace" with prior percutaneous coronary intervention and also add the variable of 2 or more episodes of chest pain in the previous 24 hours. Although both indexes are very similar, we preferred to use ours as the one described by Sanchís et al would exclude patients with a history of surgical revascularization, whereas including the use of aspirin groups together most patients with a history of cardiovascular disease. Castillo Moreno et al7 have also described a similar index that reproduces 3 of our 4 variables and replaces the use of aspirin with prior myocardial infarction. Finally, Sánchez et al11 propose an index that coincides with ours in diabetes, type of pain, and age, and replaces use of aspirin with prior coronary disease. Once more, we wish to highlight the usefulness of the variable "aspirin use," which is easy to record in the medical histories whereas patients may readily confuse previous chest pain with myocardial infarction and diagnostic coronary angiograms without significant lesions with percutaneous coronary intervention. In fact, the variable "aspirin use" is also included in the TIMI risk index (Thrombolysis In Myocardial Infarction), which is designed to stratify risk in patients with acute coronary syndrome. Finally, this same year, we have managed to show that the CPU-65 index is associated with the extent of coronary disease.8
Our data show that diagnosis of acute coronary syndrome could not be confirmed in as many as 26% of the patients admitted to the cardiology ward with suspicion of this syndrome. These patients were discharged with the diagnosis of chest pain of noncoronary origin. Most of these admissions are not appropriate. The implementation of the CPU in our hospital, 3 months after the end of data collection in this study, has proved effective at reducing this high percentage of inappropriate admissions.12 Recently published data from the DESCARTES study (Description of the State of Acute Coronary Syndromes in a Temporary Spanish Registry) gives us an idea of the size of the problem of inappropriate admissions in Spain.13 This registry included 1877 patients admitted to hospital for more than 24 hours, all with an initial diagnosis of non-ST-elevation acute coronary syndrome. Nevertheless, the discharge report ruled out coronary cause of the signs and symptoms in 18% of the cases.
Although the CPU is an effective measure for avoiding unnecessary admissions,14 inclusion of patients with a low-risk profile in the CPU, whether real or virtual, might also be inappropriate. In Spain, the prevalence of ischemic heart disease is low15 and patients are attended in the emergency department for free. These factors taken together mean that many patients attend the emergency department with noncoronary chest pain, and so mechanisms are needed to select patients who need to be assessed in the CPU. Patients with a CPU-65 index score of 0 correspond to half the population. In these 748 patients, we did not find a single case of acute myocardial infarction or death. In addition, having an index score of 0 had a negative predictive value for ischemic heart disease of 99.9%. These patients, with such a low risk profile, might not benefit from being in a CPU for tests to detect ischemia. Even the need to measure troponin levels is questionable.
Of the patients discharged from the emergency department, the most common diagnosis was atypical chest pain, followed by respiratory infection, which included pneumonia in 2% of the patients. Recent studies have shown a close relationship between pneumonia and acute myocardial infarction, as approximately 7% of the patients who caught pneumonia also suffered acute myocardial infarction16 and vice versa.17 Thus, the presence of pneumonia or some other respiratory infection does not mean that the patient is not suffering acute coronary syndrome and a careful assessment of these patients is recommended.
Limitations
Given that troponin T was only measured in 43% of the patients, we cannot rule out that some patients had an infarction and were not diagnosed. In addition, we do not have data available on biochemical markers such as C-reactive protein or the amino terminal fragment of the natriuretic peptide B, which have been shown to be useful in assessing patients with chest pain.18,19 Also, the lack of follow-up data does not allow us to draw definitive conclusions. Finally, our hospital covers a catchment area with a fairly elderly population—18% of the inhabitants are over 65 years old20—and so some of our findings might not be extrapolated to other types of population. On the other hand, our study has 2 important advantages. By studying a large number of unselected patients (1518), we have, for the first time in Spain, been able to characterize the profile of patients with chest pain who attend an emergency department. In addition, this is the first external validation of the CPU-65 index in a population other than the one used to obtain it.
CONCLUSIONS
Half of the patients who presented at the emergency department with chest pain have a very low risk profile and so their admission to a CPU (real or virtual) and, probably, measurement of markers of myocardial damage might not be necessary.
ABBREVIATIONS
CPU: chest pain unit
CPU-65: comorbid diabetes, typical pain, use of aspirin, and age 65 years or more
This study was received partial financial support from the Red Cardiovascular (RECAVA) of the Health Investigation Fund of the Ministry of Health and Consumer Affairs.
Correspondence:
Dr. M. Martínez-Sellés.
Servicio de Cardiología. Hospital Universitario Gregorio Marañón.
Dr. Esquerdo, 46. 28007 Madrid. España.
E-mail: mmselles@secardiologia.es
Received January 25, 2008.
Accepted for publication May 22, 2008.