The practice of recreational scuba diving has increased worldwide, with millions of people taking part each year. The aquatic environment is a hostile setting that requires human physiology to adapt by undergoing a series of changes that stress the body. Therefore, physical fitness and control of cardiovascular risk factors are essential for practicing this sport. Medical assessment is not mandatory before participating in this sport and is only required when recommended by a health questionnaire designed for this purpose. However, due to the significance of cardiovascular disease, cardiology consultations are becoming more frequent. The aim of the present consensus document is to describe the cardiovascular physiological changes that occur during diving, focusing on related cardiovascular diseases, their management, and follow-up recommendations. The assessment and follow-up of individuals who practice diving with previous cardiovascular disease are also discussed. This document, endorsed by the Clinical Cardiology Association of the Spanish Society of Cardiology (SEC) and the SEC Working Group on Sports Cardiology of the Association of Preventive Cardiology, aims to assist both cardiologists in evaluating patients, as well as other specialists responsible for assessing individuals’ fitness for diving practice.
Keywords
Since its inception, recreational diving in all its forms has gained increasing popularity worldwide. In particular, scuba diving has spread widely and is now practiced by millions of people each year.1 Recreational diving is a noncompetitive sport, whose main characteristics are a depth limit of 40 meters below sea level and the use of breathable gas mixtures of air or Nitrox (enriched-air).2
The main problem is that human physiology must adapt to the hostile conditions of the aquatic environment by undergoing a series of changes that stress the body. Physical fitness is therefore critical for the practice of this sport. In addition, diving is associated with a series of illnesses caused by the influence of this hostile environment on human physiology. These illnesses are frequently cardiological and sometimes prove fatal.3,4 Consequently, cardiological assessments play a vital role in identifying people unfit for diving due to the possible development of related complications.
Accordingly, we identified the need for the present document, endorsed by the Clinical Cardiology Association of the Spanish Society of Cardiology (ACC-SEC) and the Working Group on Sports Cardiology of the Association of Preventive Cardiology of the SEC (ACP-SEC). Our aim was to combine the expertise of cardiologists and undersea and hyperbaric medicine specialists in an attempt to trace a common path leading to the correct and rapid assessment of individuals, as well as to serve as guidelines on the management of illnesses associated with the effects of diving on the cardiovascular system.
PHYSICS AND PHYSIOLOGY OF SCUBA DIVING. CARDIOVASCULAR CHANGESThe changes in human physiology and in the cardiovascular system in particular cannot be fully grasped without a clear understanding of the basic physical principles governing the condition of the immersed human body.5 This understanding involves familiarity with general gas laws, particularly those of Boyle-Mariotte, Henry, and Dalton. The changes produced are explained in greater detail in the supplementary data.
DECOMPRESSION SICKNESS AND ARTERIAL GAS EMBOLISM. ROLE OF PATENT FORAMEN OVALEDecompression sickness (DCS) comprises various signs and symptoms caused by the formation and presence of inert gas bubbles (nitrogen if air or Nitrox is being inhaled) in the tissues and blood as a result of reduced ambient pressure.6,7 The manifestations of this disease vary widely, ranging from banal to fatal.7,8
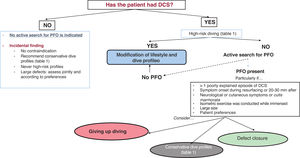
DCS has classically been associated with a patent foramen ovale (PFO).9 Indeed, the incidence of PFO is higher in individuals who have experienced DCS (up to 97% of them), mainly its cutaneous and neurological forms.10–13 When a decompression issue is identified or when an individual has more than 2 risk factors for DCS, attempting to identify the presence of this defect is not advised.14–16 The condition can be diagnosed by referring the patient to a tertiary referral cardiology department.
The management of patients with detected PFO depends on the size of the defect, on the type of dives that will be performed, and on patient preferences (figure 1). Some studies have suggested that implementing measures to reduce the inert gas bubble formation may suffice to avoid a new episode of DCS14–17 (table 1). If the person does not adopt these more conservative dive profiles or has personal preferences, percutaneous occlusion of the PFO is an option. Observational studies have demonstrated a reduction in DCS episodes after defect closure.14,17–19 In this case, patients must be informed of the possible complications of this procedure and that only individuals with fully sealed defects can resume diving (recommended at least 3 months after closure). Naturally, DCS can develop in the absence of PFO.18,20
Decision tree for the detection and management of patent foramen ovale (PFO). DCS, decompression sickness. Adapted from Pristipino et al.14.
Conservative dive profiles
| Reduce immersion time. Always within no-decompression limits |
| Increase the surface interval time (in the case of 2 dives) |
| Perform just 1 dive per day |
| Limit the dive depth to 15 m (using air) |
| Preferentially use Nitrox* |
| Lengthen decompression stops (if required) |
| Avoid vigorous/isometric exercise at least 4 h after (preferably 12 h) |
Nitrox: enriched-air Nitrox (EAN). The percentage of oxygen varies according to the mix used but will always be > 21% and will be noted on the outside of the bottle (eg, EAN 30% means 30% O2 instead of 21% air). Surface interval is the time spent on the surface until the start of the next dive. Based on this interval, the residual nitrogen from the first dive is calculated; this value is the nitrogen level at which the diver starts the second dive. Decompression stops are stops at a specific depth and time that are established based on the depth reached and the time at depth and are detailed in the decompression tables for diving with compressed air.
Current management guidelines14,18 highlight the high incidence of this defect in the general population (∼25%) and a much lower incidence of DCS (∼0.005%-0.08% of dives). Accordingly, the guidelines indicate that primary screening for this defect is ineffective in recreational diving settings.14,18 Nonetheless, recent studies suggest that screening for this defect and the application of treatment or conservative dive profiles could reduce the incidence of DCS.21
IMMERSION PULMONARY EDEMAImmersion pulmonary edema (IPE) is a commonly underdiagnosed type of pulmonary edema found in swimmers and divers.22,23 The condition causes about 10% of all diving accidents and has a mortality rate of up to 1%.24 It affects healthy individuals and typically has a benign clinical course,25 although it may sometimes be life-threatening. IPE is more frequent in women and is recurrent in almost 30% of cases.26
The pathophysiology of IPE is complex and not fully understood. Multiple predisposing factors are involved (eg, pressure, cold, increased respiratory effort, stress, physical exertion),25,27 which trigger changes in cardiopulmonary physiology, in addition to vascular redistribution from dependent areas caused by immersion, central circulation overload with the increased preload and afterload, and elevated pulmonary circulation pressure.28–30 Intense physical exercise constitutes a first-order predisposing factor,27 which increases systemic and pulmonary blood pressure.31 In addition, its genesis exhibits a predominance of right ventricular overload.32,33 The risk of IPE is greatly increased by the coexistence of a previous cardiovascular disease.
Symptoms begin at depths or during ascent and are the same as those of acute pulmonary edema due to other causes. The outcome is sometimes fatal, although other severe complications may develop, such as drowning, and, to a lesser extent, lung overexpansion and DCS. If compatible symptoms are detected, the diver must cease all physical activity, increase gas exchange in the respiratory system, and passively ascend to the surface (while trying to adhere to the decompression schedule).
Thoracic ultrasound is highly useful for early diagnosis because visualization of the comet tail artifact is well correlated with the presence of alveolar-interstitial edema.34 Symptoms rapidly ameliorate with normobaric oxygen, and diuretic and nitrate administration should be conservative, given the dehydration inherent in diving. Drugs that reduce pulmonary pressures have also been proposed, such as sildenafil,35 although their use is not widespread. After an IPE episode, resumption of underwater activity is controversial due to the risk of recurrence. The individual must undergo a fitness to dive assessment.
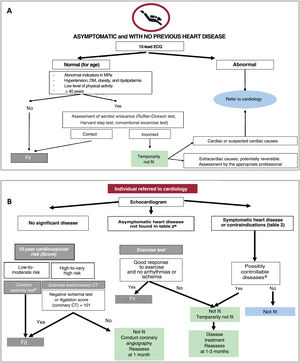
PHYSICAL FITNESS, RISK FACTORS, AND DIVINGPhysical fitness is essential for safe diving.4 Nonetheless, poor physical fitness should not be an absolute contraindication for recreational diving, as long as the diver acts responsibly.36 The objective is to determine both physical fitness and the possible development of risk factors or concomitant illnesses (figure 2).
Central illustration. Treatment approach for assessment for fitness to scuba dive. A: asymptomatic individuals with no previous cardiovascular disease. B: individuals referred to cardiology (due to symptoms, new findings, or previously known disease). Initially, the specialist in underwater and hyperbaric medicine assesses asymptomatic individuals with no relevant cardiological history and refers to cardiology only those with the indicators in panel A, after performing the illustrated steps. Cardiology evaluates individuals with previously known cardiovascular disease exhibiting abnormal data in the previous assessment (panel A), based on that shown in panel B. In all people assessed in panel B, echocardiography (ECG) should be performed to evaluate cardiac structure and function. Based on the results, the person will be ruled “fit”, “not fit”, or “temporarily not fit” for diving. The difference between these last 2 designations is that “temporarily not fit” is characterized by a situation that can be corrected and the candidate may thus become “fit” (see the text). CT, computed tomography; DM, diabetes mellitus; MRs, medical records.
a Rule out diseases listed as contraindications (table 2).
b Evaluation of exercise capacity via simple exercise testing.
Cardiovascular disease causes 26% of disabling lesions in diving and 13% of deaths, mainly in divers aged > 60 years.37,38 Specific registries of divers have found a high proportion of middle-aged people (> 50 years), as well as a high percentage of cardiovascular risk factors.24,39
According to data from the annual database of the Diving Alert Network,24 the most frequent cause of sudden cardiac death in divers is coronary heart disease; its incidence peaks at the age of 50 to 60 years. Accordingly, coronary heart disease screening is important in individuals aged > 45 years with risk factors in order to avoid the onset of an event in stressful situations as well as to identify silent ischemia (including coronary angiotomography, imaging stress testing, or conventional stress testing).4,40 Although the latter has relatively low sensitivity for early coronary heart disease, it is able to determine exercise capacity. In addition, conventional stress testing can be modified to test sustained exercise (20-30minutes) at a minimum of 6 MET, which is a plausible expectation for a recreational diver, although higher capacities are recommended for increased demands during diving.4 In particular, the ability to reach a workload of 12 to 13 MET is a good indicator of sufficient functional capacity to cope with the possible contingencies in recreational diving.46 In this regard, if possible, exercise testing with gas exchange or cardiopulmonary exercise testing is recommended due to their higher sensitivity and specificity.
The main risk associated with diabetes mellitus is loss of consciousness due to hypoglycemia, mainly in patients requiring insulin, given that diving is associated more with this type of risk.4,41 Classically, diabetes used to be a contraindication for diving. However, several undersea and hyperbaric medicine societies have relaxed their criteria for approving patients with diabetes for diving. Patients must have good control of their diabetes, with no medication change in the last month, and must undergo a medical review before and after diving. In addition, such individuals are advised to adopt a more conservative dive profile and to dive with a nondiabetic diver.42
Well-controlled controlled hypertension with no other risk factors associated with coronary heart disease is acceptable for diving, independently of whether the individual is under treatment. Grade 2 hypertension (≥ 160mmHg) is a contraindication for diving until further investigation and treatment.43
Other factors related to diving and hypertension must be mentioned. First, central blood pressure transiently increases with diving due to the physiological factors explained above.41,43 However, after diving, systemic blood pressure is unchanged vs predive values. Another related effect is the high prevalence of hypertension in people with IPE (up to 25%).44 Hypertension is associated with a higher probability of subsequent recurrence,26,45 and normotensive individuals who experience IPE are more likely to subsequently develop hypertension.22
Obesity compromises overall physical fitness and can increase the risk of DCS due to greater nitrogen consumption. Exhaustive examination is required to identify a probable underlying heart disease.4
CARDIOVASCULAR DISEASE AND DIVINGCoronary heart diseaseIn professional athletes (> 35 years) in general, the presentation of coronary heart disease ranges from asymptomatic forms to sudden cardiac death during exercise.46,47 Nonetheless, the most frequent presentation is angina. Although scuba diving does not involve considerable workloads, because the swimming required is very slight, the degree of exertion can markedly increase in certain situations (many unexpected), such as cold water, currents, and waves, which can become a highly stressful event.40 People with a history of coronary heart disease should be symptom-free and receiving optimal treatment and their risk should be evaluated using exercise testing.4,40 Individuals who have recently had acute coronary syndrome can resume diving after a variable period of rest, if they have undergone revascularization, received optimal treatment, and show both the absence of inducible ischemia on stress testing and a good exercise response. In this context, lower exercise capacities in the ischemia test would be acceptable, as long as divers are recommended to plan dives in less stressful environments (warm temperatures, without currents or large waves).40 If exercise capacity is low, it is advisable to recommend improvements, which can be effectively achieved through adherence to cardiac rehabilitation programs. Although there is no diving-specific evidence, it is prudent to follow the standard approach for any patient with a coronary episode and to reassess the patient with an exercise test between 1 and 3 months after the event. Periodic fitness examinations are recommended for divers.3,36,40
Cardiomyopathies and valvular heart diseasesIdentifying patients with cardiomyopathies is critical, because the aquatic environment can unpredictably trigger symptoms in such patients.4,36 Nonetheless, cardiomyopathy is not considered a contraindication for diving per se, with the exception of inherited cardiomyopathies, which are an absolute contraindication. However, in certain cases and after expert evaluation, a person can be certified fit for recreational diving if all parties involved accept the risk. This expert evaluation will assess exercise capacity, as well as the specific phenotype and arrhythmia burden in each person, and fitness for diving will be more frequently reviewed. Practice guidelines on sporting activity consider that adequately managed individuals with > 50% or slightly reduced (40%-59%) ejection fraction who are stable and have a good New York Heart Association functional class (NYHA I) can even participate in competitive sports.48 For diving, an ejection fraction cutoff point of > 50% has been established for participation in this activity. Classically, aquatic sports have been contraindicated in patients with cardiac dysfunction due to the preload increase with immersion, although some studies support their participation.49,50 Such patients are advised to undergo an evaluation to assess the treatment and symptoms at least yearly, as well as an exercise test to determine functional capacity and induction of hypotension and arrhythmia.4,36 Special attention should be paid to patients who have previously developed stress cardiomyopathy, given that there is a risk of relapse in stressful situations.
Mild valvular heart disease is not a contraindication.48 Controversy surrounds moderate valvular heart disease, although asymptomatic persons with regurgitation with hemodynamic effects, ejection fraction > 50%, good functional class, and no arrhythmias or ischemia on exercise testing could be considered fit. Severe regurgitation and moderate-to-severe stenosis are absolute contraindications.4,40
Arrhythmias and long QT syndrome. Implanted devicesIn individuals with arrhythmias or potentially arrhythmogenic substrates, there are 2 key considerations: the risk of sudden cardiac death, and the extent of control of the risk of the development of syncope or limiting symptoms (reduced exercise tolerance) during immersion. The aquatic environment can reduce control and thereby lead to symptoms.48,51 Compared with supraventricular arrhythmias, ventricular arrhythmias normally have a worse prognosis and are associated with structural damage, highlighting the importance of their identification and treatment.48 Supraventricular arrhythmias generally have a better prognosis but must be controlled due to the possibility of syncope or exercise limitation, which can severely complicate immersion.4,36 Patients with these conditions are advised to undergo an exercise test to assess the extent of control and exercise tolerance using the thresholds described above under the heading “Physical fitness, risk factors, and diving”. In addition, the stress produced by the environment can lead to a loss of rhythm control during dives.14,17,18 Currently, many arrhythmias (particularly supraventricular) can be effectively corrected through invasive procedures, allowing these patients to resume diving after a new cardiology assessment.
The situation differs for channelopathies, particularly long QT syndromes, which are an absolute contraindication for diving.4,36,51,52 The “autonomic conflict” is a recognized trigger for episodes in individuals with an arrhythmogenic substrate.14,17,18 In addition, immersion in water and swimming are classic triggers for arrhythmias in long QT syndrome type 1.48 A common treatment is implantation of intracardiac devices, such as pacemakers and defibrillators. The latter devices are a formal contraindication for diving. Studies have examined pacemaker response to the elevated pressures due to the possibility of damage or malfunction at pressures > 4.0atm (30-meter depth).53
Adult congenital heart diseasesDue to the improved survival of patients with congenital heart disease (CHD) and their generally good quality of life when they reach adulthood, the number of people with CHD wishing to practice diving has increased. Because CHDs vary widely, not all are currently deemed as contraindications for diving. All individuals with a CHD interested in taking up diving must undergo an annual medical review in a CHD referral center to assess their anatomy, surgical history, and residual lesions. Essential components of this assessment are echocardiography and exercise testing (with gas exchange). In the latter, regardless of the type of heart disease, the individual must have a minimum exercise capacity of 8 MET (recommended maximum oxygen volumes of > 40mL/kg/min in men and > 35mL/kg/min in women). Specific considerations for each heart disease are detailed in table 1 of the supplementary data.54
CARDIOLOGICAL ASSESSMENT OF FITNESS TO DIVEA medical certificate should be obtained confirming divers’ good physical fitness and health. According to the Boletín Oficial del Estado (Official State Gazette of Spain), all divers are responsible for ensuring that their health meets the required standards, with the sole requirement for recreational diving being a declaration of health status, which is obtained using a questionnaire. Evidence of any condition that could jeopardize diver safety or indications that the diver's health is insufficient will result in diving not being permitted without a certificate accrediting that the individual has passed an annual medical review.2
We recommend that all candidates wishing to be exposed to the aquatic environment, particularly those older than 45 years, undergo a medical examination to determine their fitness to dive.4 This will focus on both health habits (sporting activity, with consideration of intensity and weekly frequency), and screening of pathological history (table 2 and table 1 of the supplementary data). The assessment must include resting a 12-lead electrocardiogram in all candidates, given that they will be starting or continuing a sporting activity.55 The physical evaluation of the candidate can be conducted through tests measuring aerobic endurance and heart recovery (Ruffier-Dickson test) or with an exercise test when there is evidence of a physical limitation, in people aged > 40 years with obesity, or in individuals with cardiovascular concerns (figure 2).55,56
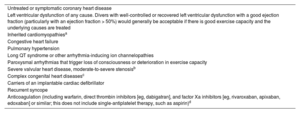
Contraindications for diving (not fit).
| Untreated or symptomatic coronary heart disease |
| Left ventricular dysfunction of any cause. Divers with well-controlled or recovered left ventricular dysfunction with a good ejection fraction (particularly with an ejection fraction > 50%) would generally be acceptable if there is good exercise capacity and the underlying causes are treated |
| Inherited cardiomyopathiesa |
| Congestive heart failure |
| Pulmonary hypertension |
| Long QT syndrome or other arrhythmia-inducing ion channelopathies |
| Paroxysmal arrhythmias that trigger loss of consciousness or deterioration in exercise capacity |
| Severe valvular heart disease, moderate-to-severe stenosisb |
| Complex congenital heart diseasesc |
| Carriers of an implantable cardiac defibrillator |
| Recurrent syncope |
| Anticoagulation (including warfarin, direct thrombin inhibitors [eg, dabigatran], and factor Xa inhibitors [eg, rivaroxaban, apixaban, edoxaban] or similar; this does not include single-antiplatelet therapy, such as aspirin)d |
Modified from Jepson et al.4
Individuals can be considered fit to dive if they have moderate regurgitation without hemodynamic repercussion or symptoms with EF > 50% and with a good functional class without arrhythmia or ischemia induction on exercise stress testing.
These abnormalities must be evaluated by an underwater and hyperbaric medicine specialist and a cardiologist before such individuals are authorized to dive. See table 1 of the supplementary data.
Some experts permit anticoagulant therapy in certain circumstances. This issue remains controversial and there is a lack of reliable evidence supporting one or the other approach. The same occurs with dual antiplatelet therapy after stent implantation, although the most reasonable strategy is to wait until the patient is switched to monotherapy.
The result of the medical assessment will be “fit”, “not fit”, or “temporarily not fit”, when the condition is possibly reversible or can be controlled with medication suitable for underwater use. The frequency of the cardiovascular medical evaluation is based on age and the condition in question. Healthy persons aged 40 years or less are recommended to undergo a medical review every 2 years. Individuals aged > 40 years or with cardiovascular disease should be examinated annually or even every 6 months; this is to be decided by the examining cardiologist.
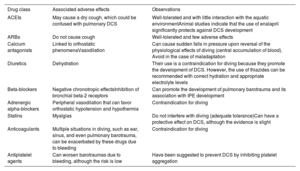
CARDIOVASCULAR DRUGS AND DIVINGThere are scarce data on the behavior of pharmacological agents in the aquatic environment 57–60; some studies have been performed in a dry environment (hyperbaric chamber), which limits the results because no consideration is given to the inherent effects of immersion and hypothermia or the physical effect of the fins and the manipulation of the diving equipment.58 Therefore, in candidates prescribed medication with cardiovascular effects, the fitness test should focus on various factors. Diving reduces glucose levels and favors the development of dehydration and acidosis.57,61 It is important to determine the person's tolerance to the drug, the presence of side effects that might be minimal on the surface but can become significant underwater,57 the possible intensification of toxic situations upon interaction with breathing gases,57 and, finally, elucidation of the possible arrhythmogenic effect of the drug in an environment that inherently favors changes in heart rhythm.60,62 The candidates’ disease is more limiting than the medication used for its treatment.61
Taking into account the abovementioned factors, various positions have been taken: some authors argue that patients with cardiovascular disease and taking heart medication are unfit to dive,57 while others adopt a more tolerant approach.41 In the case of the latter stance, options include changing the drug or dose61 or recommending a more conservative dive profile (table 1); informing the patient of the risks and preventive measures; teaching the patient to recognize the signs of an IPE and to halt the dive at the first warning sign43; and advising the patient to avoid dives in cold water or without adequate thermal protection. table 3 details the drug classes most frequently used in cardiology.
Common pharmacological agents and their relationship with diving
| Drug class | Associated adverse effects | Observations |
|---|---|---|
| ACEIs | May cause a dry cough, which could be confused with pulmonary DCS | Well-tolerated and with little interaction with the aquatic environmentAnimal studies indicate that the use of enalapril significantly protects against DCS development |
| ARBs | Do not cause cough | Well-tolerated and few adverse effects |
| Calcium antagonists | Linked to orthostatic phenomenaVasodilation | Can cause sudden falls in pressure upon reversal of the physiological effects of diving (central accumulation of blood). Avoid in the case of maladaptation |
| Diuretics | Dehydration | Their use is a contraindication for diving because they promote the development of DCS. However, the use of thiazides can be recommended with correct hydration and appropriate electrolyte levels |
| Beta-blockers | Negative chronotropic effectsInhibition of bronchial beta-2 receptors | Can promote the development of pulmonary barotrauma and its association with IPE development |
| Adrenergic alpha-blockers | Peripheral vasodilation that can favor orthostatic hypotension and hypothermia | Contraindication for diving |
| Statins | Myalgias | Do not interfere with diving (adequate tolerance)Can have a protective effect on DCS, although the evidence is slight |
| Anticoagulants | Multiple situations in diving, such as ear, sinus, and even pulmonary barotrauma, can be exacerbated by these drugs due to bleeding | Contraindication for diving |
| Antiplatelet agents | Can worsen barotraumas due to bleeding, although the risk is low | Have been suggested to prevent DCS by inhibiting platelet aggregation |
ACEIs, angiotensin-converting enzyme inhibitors; ARBs, angiotensin II receptor blockers; DCS, decompression sickness; IPE, immersion pulmonary edema.
The popularity of recreational diving has has grown globally, attracting practitioners with widely different ages, medical histories and, in particular, physical fitness levels. Because cardiovascular disease is the leading cause of diving-related accidents, including fatal and disabling incidents, these conditions need to be identified and appropriately treated and managed to prevent accidents. Nonetheless, the literature on cardiovascular disease and diving is scarce, and prospective registries are required to serve as the basis for treatments in an attempt to standardize the interventions of all professionals involved in the evaluation and management of cardiovascular disease in diving.
FUNDINGNone.
STATEMENT ON THE USE OF ARTIFICIAL INTELLIGENCEArtificial intelligence has not been used in the preparation of this article.
AUTHORS’ CONTRIBUTIONSA. Tello Montoliu, A. Olea González, A. Pujante Escudero, M. Martínez del Villar, F. de la Guía Galipienso, and L. Diaz González were in charge of the manuscript design, drafting, and revision. R. Fernández Olmo and R. Freixa-Pamias were in charge of manuscript revision. D. Vivas Balcones was in charge of the manuscript design and revision.
CONFLICTS OF INTERESTNone of the authors has a conflict of interest associated with the present article.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2024.04.001