A 40-year-old man, originally from Morocco, was admitted to our hospital with suspicion of vascular catheter-associated bacterial endocarditis. His only past medical history was idiopathic intestinal pseudo-obstruction, which had been thoroughly investigated by the gastroenterology team, and which caused intestinal obstructive crises and oral intolerance, so he had been started on parenteral nutrition 2 months prior.
He presented with Staphylococcus epidermidis bacteremia, sensitive to methicillin (4/4 blood cultures) secondary to vascular catheter infection, with positive tip culture during an admission for an intestinal obstructive crisis in a district hospital in our area. The vascular catheter was replaced and treatment with cloxacillin started. Echocardiography showed no structural heart disease and a 25 × 12mm mobile mass in the right atrium, which appeared to be attached to the interatrial septum but also surrounded the catheter. He was referred to our hospital for assessment of possible catheter-associated endocarditis.
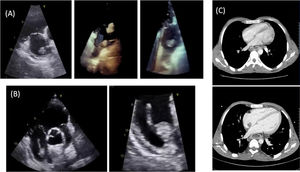
On arrival, he was hemodynamically stable, and physical examination revealed he was notably cachexic, with no signs of heart failure or stigmata of endocarditis. Echocardiography (figure 1A) showed persistence of the mobile mass in the right atrium. Blood cultures were negative. The vascular catheter was removed under echocardiographic guidance. The mobile mass remained attached to the interatrial septum (figure 1B). Catheter culture was negative. Computed tomography (CT) angiography ruled out pulmonary embolism and confirmed the presence of a thrombus adhered to the interatrial septum, which had not been seen on chest and abdomen CT performed months prior as part of the gastrointestinal workup (figure 1C), making a diagnosis of atrial myxoma very unlikely. Although the most likely diagnosis was atrial thrombus, it was decided to continue antibiotic therapy, and prophylactic anticoagulation was increased to a therapeutic dose, but this had to be stopped at 72hours due to an episode of upper gastrointestinal bleeding, with severe anemia, secondary to stress ulcers seen on urgent endoscopy.
Follow-up echocardiography at 1 week showed persistence of the mass. Due to the risk of embolism given its size, the case was discussed in a medical-surgical case meeting but rejected on the basis of severe malnutrition. Given the impossibility of restarting anticoagulation, it was decided to proceed to percutaneous extraction using the AngioVac thrombus aspiration system (AngioDynamics, Inc; USA).
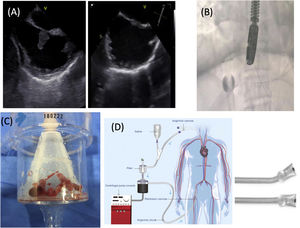
The procedure was performed under general anesthetic, with endotracheal intubation and mechanical ventilation, in the cardiac catheterization laboratory, with a cardiac surgeon present in case of complications requiring conversion to open surgery. An extracorporeal bypass circuit was set up by placing a cannula in the right femoral vein (26 Fr), through which the thrombus aspiration catheter (22 Fr) was introduced; a reinfusion cannula (26 Fr) was placed in the left femoral vein, after passing through a filter. The procedure was done under transesophageal echocardiographic (figure 2A) and fluoroscopic (figure 2B) guidance. Copious thrombotic material was aspirated (figure 2C), with pathology indicating thrombus, with no microorganisms and with negative cultures. The diagnosis of catheter-associated atrial thrombus was confirmed.
After the procedure, the patient was admitted to the coronary care unit and progressed well, so was transferred to the gastrointestinal ward to continue treatment for his intestinal condition. Portable echocardiography 1 month later showed no presence of thrombus.
AngioVac is a percutaneous thrombus aspiration system designed for en bloc aspiration of endovascular material (figure 2D). It was designed in 2009 by Vortex Medical and approved by the Food and Drug Administration the same year. The first clinical use was reported in 2011 for the removal of an implantable cardioverter defibrillator-associated infected clot.1 Using a venous-venous extracorporeal circuit, blood is drained through an aspiration cannula and returned via a second venous cannula, after passing through a filter that separates the clot from the recirculating blood.
The system has been used for extraction of thrombi from the inferior vena cava and the right atrium (80.5% success), endocarditis vegetations on right heart valves or devices (74.5% success), and pulmonary thromboembolism (32.4% success), with greater difficulty in this situation due to the low flexibility of the catheter.2,3 Cases of mural thrombus extraction without complications have been described.4
The complication rate is low; the most common is hematoma at the puncture site and distal embolization. Rare, but potentially serious complications include cardiac rupture, tricuspid valve damage, and dislodging of intracardiac devices. The system allows conversion to veno-arterial extracorporeal membrane oxygenation with the insertion of an arterial cannula and adaptation of an oxygenation membrane to the circuit. The main limitations are its high cost, risk of complications, and current lack of scientific evidence, supported only by clinical cases and case series without comparison groups. In our opinion, therefore, this treatment should be considered as an alternative to medical or surgical treatment in patients unable to undergo conventional treatment.
In conclusion, this is the first published experience in our country using the AngioVac percutaneous thromboaspiration technique. It is a safe and effective technique for the extraction of thrombi in the inferior vena cava or right atrium and of right heart valve or device-associated vegetations and is a potential alternative for cases in which conventional treatment is contraindicated.