To the Editor:
The AngioSculpt PTCA balloon catheter (Angioscore, Inc.) consists of a semirigid balloon surrounded by nitinol spirals, the purpose of which is to dilate and rupture complex atherosclerotic plaques, minimizing slippage of the balloon, as in cases of restenotic, ostial, fibrocalcific, or other types of lesions. We describe the entrapment of an AngioSculpt PTCA balloon catheter during the predilatation of a heavily calcified lesion, analyzing the possible causal mechanism.
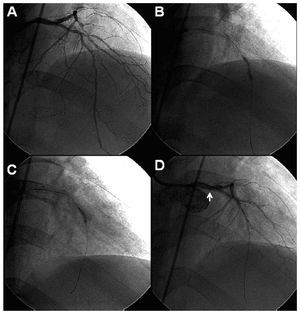
The patient was a 60-year-old man with a history of hypertension, diabetes mellitus and end-stage renal disease requiring chronic dialysis. He was admitted due to unstable angina, with anterior electrocardiographic changes and heart failure. His left ventricular ejection fraction was severely depressed. Coronary arteriography revealed disease in three major vessels, with a long, calcified lesion in the middle segment of anterior descending artery (ADA) (Figure 1A). Surgery was ruled out due to the high risk involved and the poor condition of the distal beds. Thus, percutaneous revascularization of the ADA was attempted.
With great difficulty, we were able to advance a hydrophilic guidewire along the middle segment of the ADA with a 1.25´10 mm balloon; it was necessary to dilate the proximal portion of the lesion and gradually push the balloon until it was completely advanced. Then, dilatation was repeated in the most critical stenosis with a 2´15 mm balloon, but adequate expansion was not achieved (Figure 1B). Thus, an AngioSculpt balloon (2´10 mm) was utilized but, after several attempts, it did not pass through the entire lesion and, therefore, as with the previous balloon, it was inflated in the proximal portion (Figure 1C). Once deflated, the attempt was made to advance it without success. Upon withdrawing it, it could only be moved a few millimeters and remained entrapped within the coronary artery. The attempt was again made to advance it with rotating movements and withdraw it, unsuccessfully. Another guidewire was introduced with another parallel balloon in the attempt to free it (with the buddy balloon technique), again unsuccessfully. After several attempts, a nonocclusive dissection was produced in left main coronary artery, caused by the deep intubation of the guide catheter (Figure 1D). Finally, emergency surgery was indicated in order to resolve the situation. As the heart surgeon was unable to withdraw the catheter, he cut it at the level of the ostium of the left main coronary artery, and it proved impossible to bridge the artery because of the poor condition of the bed and the severe calcification. The patient was discharged, but died 6 months after the procedure.
Figure 1. A: cranial anteroposterior projection showing a long calcified lesion in the middle segment of anterior descending coronary artery. B: conventional balloon dilatation with residual plaque, indicating the difficulty involved in its rupture. C: dilatation with the AngioSculpt balloon catheter at the level of the lesion. D: final angiography showing distal dissection of left main coronary artery (white arrow), with reduced flow in anterior descending coronary artery.
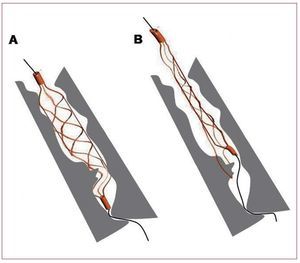
Percutaneous treatment of diffuse, calcified lesions is associated with a high risk of complications, and the advance and release of the devices, as well as their correct expansion, prove problematic. Although the rotoblator is the device of choice in the management of these lesions, one alternative is the use of balloons that cut the plaque, such as the cutting balloon or the AngioSculpt balloon.1 A possible complication can be the entrapment of this device, as occurred in this case, and a hypothetical explanation would be that the nitinol guidewire that forms a spiral around the AngioSculpt balloon could get caught on the calcium spicules on withdrawal (Figure 2).
Figure 2. Hypothetical mechanism of entrapment. A: dilatation with AngioSculpt balloon catheter of a calcified lesion. B: the nitinol guidewire that surrounds the balloon may get caught on the calcium spicules when the attempt is made to withdraw it.
There are a number of strategies in the attempt to withdraw an entrapped balloon catheter, such as inflation-deflation, advancing and rotational movements, the buddy balloon technique and deep intubation of the guide catheter. In this case, all of them failed and, thus, it was ultimately decided to perform surgical withdrawal. The operation usually consists in placing a graft in the damaged artery and removing foreign elements from the aorta to prevent thrombus formation.2 It is up to the surgeon to decide whether to attempt to withdraw the entrapped catheter because of the arterial damage that this maneuver can produce.
This report describes a serious complication of the use of the AngioSculpt catheter in diffuse, heavily calcified lesions. We consider it important to avoid the inflation of the balloon if it has not gone beyond the most critical lesion. When the balloon catheter can not be withdrawn, one possible cause is that the guidewire that surrounds it gets caught in the calcium spicules. One maneuver that can be employed to withdraw it would be advancing and rotating the balloon to release it. Finally, this case illustrates the importance of considering rotational atherectomy in the treatment of diffuse calcified lesions.