To the Editor:
We present the case of a 48-year-old woman, an ex-smoker with hypertension as the only history of interest, who came to the emergency room after having experienced 3 episodes of effort-induced syncope.
The physical examination revealed a systolic murmur (grade III/IV) localized to lung and normocytic and normochromic anemia as the only analytical sign of disease. The electrocardiogram and chest radiography were normal.
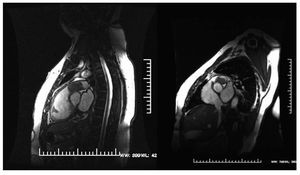
Transthoracic echocardiogram revealed severe pulmonary stenosis, although adequate vision of the pulmonary valve was not achieved. Thus, transesophageal echocardiography was performed, which showed an infiltrative-like mass in main pulmonary artery, a finding that was highly indicative of intimal sarcoma. This finding was confirmed by means of magnetic resonance (Figure 1).
Figure 1. Magnetic resonance shows a hyperintense mass that occupies nearly the entire main pulmonary artery.
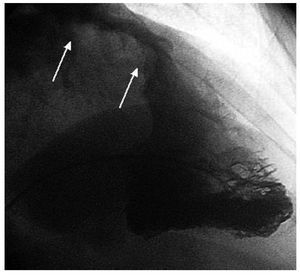
Left and right-heart catheterization demonstrated a defect in repletion (45´30 mm) at the level of the pulmonary trunk, which nearly occluded the systolic blood flow in that region (Figure 2).
Figure 2. Angiography of right ventricle shows a defect in repletion (45´30 mm) at the level of the main pulmonary artery that extends to the level of the valve and the ventricular outflow tract.
Manometry demonstrated a systemic pressure of 160/80 mm Hg, of 90/14 mm Hg in right ventricle and of 14 mm Hg in mid-right ventricle. There were no lesions in the coronary arteries.
With a more than probable diagnosis of sarcoma of the pulmonary artery, a surgical intervention was carried out to resect the tumor. It was not possible to preserve the pulmonary valve because the tumor mass affected two of its leaflets. Thus, it was replaced with a 25-mm Biocor porcine bioprosthesis, and the pulmonary artery was reconstructed with a bovine pericardium patch. The diagnosis of sarcoma was confirmed intraoperatively.
The postoperative period was uneventful and the patient was discharged, after which, she was referred to the oncological day clinic to begin adjuvant chemotherapy. After 8 months of follow-up, she is asymptomatic and there is no evidence of tumor recurrence.
Primary sarcoma of the pulmonary artery is an uncommon condition, and its early diagnosis is difficult, since the presenting symptoms are usually nonspecific. The patients may present with dyspnea, pleuritic pain, cough and hemoptysis, which can be interpreted as pulmonary thromboembolism or signs and symptoms of neoplasm1 (asthenia, weight loss, and poor general condition).
The definitive diagnosis is established on the basis of the histopathological study. Primary pulmonary artery sarcomas are classified as intramural (usually leiomyosarcomas) and luminal, referred to as intimal sarcomas. The latter are highly undifferentiated and can derive from pluripotential subendothelial mesenchymal cells that differentiate toward myofibroblastic cells. They extend throughout the lumen as polypoid masses; less frequently, they grow proximally, affecting the pulmonary valve and right ventricle, as in this case.
A high index of suspicion is required to achieve an early diagnosis, and there is no specific diagnostic test for this condition. Chest radiography may reveal pulmonary nodules, pulmonary artery dilation, reduced pulmonary vasculature and cardiomegaly. The echocardiogram may show a dilated right ventricle with obstruction of the ventricular outflow tract or of the pulmonary trunk. Angiography reveals defects in repletion in the pulmonary artery lumen. Contrast-enhanced computed tomography enables the detection of masses in the pulmonary artery, but is unable to differentiate between a thrombus and a tumor in the absence of secondary lesions, such as pulmonary nodules or adenopathies. Gadolinium-enhanced magnetic resonance is useful because it enables the differentiation between a thrombus and a tumor, since the injection of gadolinium reveals the latter.2
The mortality caused by these tumors depends on their location and the vascular extension.
Surgery is elective, but will only be successful if the resection is complete. The techniques employed include pneumonectomy with reconstruction of the pulmonary artery outflow tract and endarterectomy with cardiopulmonary bypass.3
The prognosis is poor, with a mean survival of less than 2 months in patients who do not undergo surgery and approximately 10 months in those who do, regardless of the histological findings.4 The role of radiotherapy and chemotherapy is not clearly defined.
In conclusion, sarcoma of the pulmonary artery is uncommon, and the onset can be nonspecific. Thus, early diagnosis is difficult and requires a high degree of clinical suspicion. It is important to take this lesion into account in the differential diagnosis of chronic dyspnea and in cases of pulmonary thromboembolism with poor response to anticoagulation therapy or in which there is clinical evidence of neoplasm.