To the Editor:
We report a case of acute mitral insufficiency due to anterolateral papillary muscle rupture secondary to chest trauma. In our case, mitral valve repair was performed as an alternative to valve replacement, with good results during the immediate postoperative period and follow-up.
The patient was a 41-year-old man with nothing remarkable in his medical history. He presented with high-energy frontal and lateral polytrauma and chest trauma, without central nervous system involvement, following a traffic accident. As a consequence of the trauma, he had several fractured ribs and bilateral pneumothorax (tension pneumothorax on the left side) and, thus, pleural drainage catheters were inserted. He also presented with pneumomediastinum, subcutaneous emphysema, and areas of pulmonary contusion, with no other apparent chest injuries.
A few hours after admission, he exhibited radiological signs of acute pulmonary edema, which required orotracheal intubation and mechanical ventilation. Among the signs, we detected the development of a systolic cooing murmur (grade 3/6 over the mitral valve area), radiating toward the axilla. The electrocardiogram was normal.
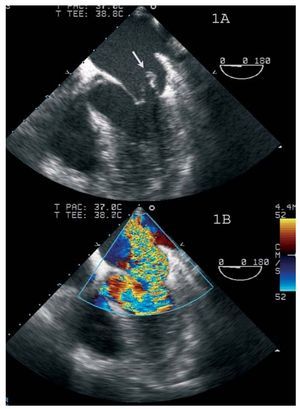
Transthoracic echocardiography was performed, revealing severe mitral regurgitation due to rupture of the head of the anterolateral papillary muscle, which provoked the complete prolapse of the P1 scallop (posterior leaflet) and A1 scallop (anterior leaflet), with eversion of the anterolateral commissure toward the left atrium (Figure 1).
Figure 1. A: 4-chamber transesophageal echocardiographic view, showing an image indicating anterolateral papillary muscle rupture, with prolapse into the left atrium (arrow). B: color Doppler ultrasound showing severe mitral regurgitation jet.
With a diagnosis of acute pulmonary edema caused by mitral regurgitation secondary to traumatic rupture of the anterolateral papillary muscle, the decision was made to treat the patient surgically. The intraoperative macroscopic findings were severe inferoposterior myocardial contusion with right lateral pericardial rupture and an anatomically normal mitral valve, with rupture of the head of anterolateral papillary muscle and loss of the support of the chordae of P1 and A1. Surgical repair was performed by means of mitral valvuloplasty, with resection of the papillary muscle and reconstruction, plication of the P1-A1 segments of the anterolateral commissure and a one-stitch suture in the zone of the ring to reduce the stress on the leaflets. Intraoperative echocardiography demonstrated a good result, with mild residual mitral regurgitation. The subsequent clinical course was good, and the patient was extubated 24 hours after surgery.
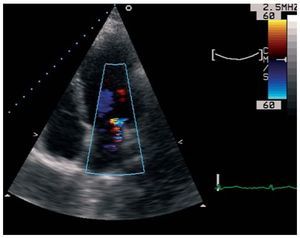
After a follow-up of 1 year, he continues to be asymptomatic with respect to dyspnea, and echocardiographic monitoring demonstrates mild-to-moderate mitral regurgitation, which remains stable (Figure 2).
Figure 2. Follow-up monitoring using 4-chamber transthoracic echocardiography in which color Doppler ultrasound shows mild-to-moderate mitral regurgitation jet.
Among our general population, traumatic cardiac injury occurs in 9% to 21% of cases of blunt chest trauma, more often with aortic rather than mitral valve involvement.1 In most cases, mitral valve involvement is associated with that of other cardiac structures, since an isolated lesion is very rare.
In a classic study, Parmley et al2 reported mitral valve lesions in a series of 546 autopsies in cases of nonpenetrating chest trauma, in all of which there were associated lesions. The most common mitral valve lesion involved the papillary muscles.
Mitral regurgitation following blunt chest trauma may be due to the involvement of any of the components of the valve apparatus (papillary muscles, chordae tendineae, leaflets, etc). The mechanism producing mitral valve lesions appears to be an increase in intracardiac pressure at end-diastole and during isovolumetric contraction.
Surgical treatment of mitral regurgitation due to traumatic rupture of the anterolateral papillary muscle is an uncommon approach. Only 12 cases of surgical intervention for anterolateral papillary muscle rupture have been reported.3-5 There is only one report of mitral valve repair with reimplantation of the anterolateral papillary muscle.5 Prosthetic valve replacement is the most widely performed intervention for anterolateral papillary muscle involvement, in contrast to posteromedial papillary muscle rupture, in which papillary muscle reimplantation and annuloplasty are much more frequently performed. In our case, mitral repair was carried out by means of a slightly different technique, with resection of the affected anterolateral papillary muscle. Given that the valve apparatus was anatomically normal and the alteration was acute, ring placement was not considered necessary, and good support was achieved with a one-stitch suture in the zone of the ring.