In primary angioplasty, the interval between first medical contact (FMC) and reperfusion should be less than 120minutes. The time to reperfusion varies depending on where FMC is established. Recent studies suggest longer times in patients presenting in off-hours. The objective is to evaluate the time intervals between the onset of symptoms and reperfusion according to where the FMC occurs and time of day of patient presentation.
MethodsProspective observational study of acute myocardial infarction patients treated with primary angioplasty (February 2007 to May 2009). Depending on the FMC, patients were classified as belonging to the hospital group (hospital with primary angioplasty), the transfer group (hospital without primary angioplasty), or the emergency medical system (EMS) group (out-of-hospital care). For each group, the prehospital delay, diagnostic delay, delay in activation and/or transfer, and procedure delay were recorded.
ResultsPrimary angioplasty was performed in 457 patients: 155 in the hospital group, 228 in the transfer group and 72 in the EMS group. The median [interquartile range] door-to-reperfusion times were 80 [63-107], 148 [118-189] and 81 [66-98] minutes, respectively (P <.0001). The transfer group showed a greater delay in diagnosis (P <.0001) and delayed activation and/or transfer (P <.0001). The EMS group had the shortest total time due to a reduced prehospital delay (P =.001). No difference was found with regard to the time of presentation (P =.42).
ConclusionsTransfer group patients were treated later and EMS group patients much earlier. There were no differences in association with the time of presentation. The identification of inappropriate delays should enable the introduction of measures to improve the efficiency of treatment.
Keywords
.
INTRODUCTIONPrimary angioplasty (PA) is the treatment of choice in ST-segment elevation acute myocardial infarction (STEMI), provided it is performed by an experienced team and with an interval between the first medical contact (FMC) and balloon inflation (first medical contact-to-reperfusion time [FMCRT]) of less than 120minutes.1 This procedure has been shown to be superior to fibrinolysis, with significantly lower rates of mortality, reinfarction and cerebral hemorrhage.2, 3, 4, 5 This benefit is observed even if it is necessary to transfer the patient to a center specialized in PA.6, 7
In Spain, access to PA is still limited for many patients. Although some centers are linked to local networks8 and certain Spanish autonomous regions have established PA programs (APRIMUR [Primary Angioplasty in the Region of Murcia] and PROGALIAM [Program for Management of Acute Myocardial Infarction in Galicia], among others),9 the MASCARA study demonstrated that only 37% of the patients with STEMI who received reperfusion therapy were treated with PA.10 Depending on where the FMC takes place, we can differentiate among patients who are brought to centers with PA capability, patients brought to centers in which PA cannot be performed, and patients treated in an out-of-hospital setting by the emergency medical system (EMS). There are a number of factors that lead to a delay in treatment and they vary depending on the site of the FMC; thus, the route by which the patient arrives can be a determinant in the analysis of the delay attributable to PA. Moreover, several recently published reports indicate that patients arriving during off-hours are subject to a longer delay in the performance of PA.11, 12
The objective of this study is to analyze the time elapsed between the onset of symptoms and reperfusion during PA according to where the FMC occurs and whether the procedure is performed during normal working hours or during off-hours (after hours and on weekends or holidays). This was made possible by the establishment, in our health area, of a local network of voluntary cooperation among the centers that comprise it.
METHODS PatientsThe study was based on a prospective observational registry of all the consecutive patients with STEMI treated with PA between February 2007 and May 2009. This therapeutic approach was considered to be indicated in patients with chest pain and an electrocardiogram showing ST segment elevation in two or more adjacent leads, reaching at least 0.1mV in frontal leads and 0.2mV in precordial leads, or with left bundle branch block, either newly acquired or of indeterminate age. The exclusion criteria were the presence of end-stage disease or severe comorbidity or the absence of arteriovenous access, according to the criteria of the physician attending the FMC.
The clinical and procedural variables and the time intervals measured were recorded in a database immediately after the performance of PA.
Organization of the Local Healthcare NetworkIn February 2007, we set up a local network for PA with its base in our center, which provides care to a population of 817000 inhabitants, mainly distributed among 4 urban centers in the Spanish province of Barcelona (Badalona, Santa Coloma de Gramenet, Mataró and Calella de la Costa). Each city has a hospital and all have easy access to our center via expressway at distances of 2, 7, 20 and 45km, respectively.
The patients were brought from the emergency service of our own PA center, from the emergency services of the 4 regional hospitals, or from other centers outside our sphere of influence, or received out-of-hospital care from an emergency unit equipped to provide life support, pertaining to the EMS.
A series of measurements were made at the start of the program in the attempt to optimize care time:
1. A diagnostic and procedural protocol to be applied in any candidate for PA was drawn up.
2. A checklist was prepared with indications, contraindications, and medication to be administered, in which the different time intervals studied were prospectively included for subsequent analysis.
3. The decision was made to install a direct dedicated telephone line for permanent contact.
4. The decision was made to transport all the patients transferred from other centers or treated outside the hospital setting by the EMS.
5. A commitment to the permanent availability of beds was adopted.
The program was launched without incrementing the infrastructure or the personnel involved.
The patients who come directly to the hospital with PA capability are initially assessed in the emergency service and, if STEMI is suspected, the cardiologist on duty is alerted and he or she activates the PA system.
In the case of patients who arrive at a hospital without PA capability, the cardiologist on duty at our center is contacted and, again, he or she activates the PA system. The transport from one hospital to another is carried out in emergency units from the EMS, which are specific for interhospital transport and generally differ from those employed in out-of-hospital care (secondary EMS).
Out-of-hospital care is activated by means of a call to an emergency telephone (061 or 112) and is provided by EMS units, which have 3 bases, 1 in our center and the other 2 in regional hospitals in the area (primary EMS).
Normal working hours are from 8:00 to 21:00 on Monday through Thursday and from 8:00 to 15:00 on Fridays.
Outside these hours and on weekends and holidays, a team consisting of an interventional cardiologist and 2 qualified nurses is on call. There are 3 interventional cardiologists and the nursing staff of the unit to cover off-hours. This team is activated by means of a centralized call and should be in the laboratory within 30minutes.
Study VariablesThe clinical characteristics of the patients and the characteristics of the procedure were collected prospectively. The patients were classified into 3 groups according to where the FMC took place:
– Hospital group: patients who went directly to the emergency department or patients who were already hospitalized in our center (with PA team).
– Transfer group: patients sent from other hospitals (no PA team).
– EMS group: patients who received out-of-hospital care from EMS personnel.
For the analysis of the delay, we decided to collect prospectively the following time points:
– Time of onset of the symptoms, directly from the patients or their relatives.
– Time of initiation of the FMC (in-hospital or out-of-hospital): moment at which the patient arrived at a location in which STEMI could be diagnosed and PA indicated. In those patients treated in the hospital setting, this was considered to be the time of arrival at the emergency department according to the administrative records, and in the patients receiving out-of-hospital care, the time of arrival of the EMS unit.
– Time of therapeutic indication: moment at which our center was alerted from the point of origin of the patients from other centers or of those receiving out-of-hospital care, or the moment in which the cardiologist on duty alerted the interventional cardiology team for those patients being treated directly in our center.
– Time of arrival in the cardiac catheterization laboratory: moment at which the patient entered the laboratory.
– Time of arterial access: moment at which the first intracoronary device (simple balloon, stent, or thrombectomy device)13 was introduced into the diseased artery.
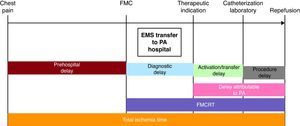
Using these time points, the following intervals were defined (Figure 1):
– Prehospital delay: time of symptom onset to time of initiation of the FMC.
– Diagnosis-related delay: time of initiation of the FMC to time of therapeutic indication.
– Activation/transfer-related delay: time from therapeutic indication to time of arrival in the cardiac catheterization laboratory.
– Procedure-related delay: time of arrival in the cardiac catheterization laboratory to time of arterial access.
– PA-related delay: time of therapeutic indication to time of arterial access.
– FMCRT: time of initiation of the FMC to time of arterial access.
– Total ischemia time: time of onset of the symptoms to time of arterial access.
Figure 1. Time intervals analyzed from the onset of symptoms to reperfusion. EMS, emergency medical system; FMC, first medical contact; FMCRT, first medical contact-to-reperfusion time; PA, primary angioplasty.
Statistical AnalysisThe continuous variables were expressed as the mean±standard deviation and were compared using one-way ANOVA with 3 treatment groups. The categorical variables were expressed as n (%) and were compared by means of the Pearson chi-square test. Those variables that did not follow a normal distribution were expressed as the median [interquartile range] and were compared using the Kruskal-Wallis nonparametric test. A two-sided P value less than .05 was considered significant for all the tests. The analysis of the data was carried out using the SPSS 16.0 software package (SPSS Inc.; Chicago, Illinois, United States).
RESULTS Population CharacteristicsBetween February 15, 2007 and May 30, 2009, PA was performed in 457 consecutive patients with STEMI (290 procedures per million population/year): 155 patients (34%) in the hospital group, 230 patients (50%) in the transfer group, and 72 patients (16%) in the EMS group. We did not reject any of the patients assessed outside our center who fulfilled all inclusion criteria and none of the exclusion criteria. The clinical and angiographic characteristics of the patients and the features of the procedure are summarized in Table 1.
Table 1. Patient Baseline and Procedural Characteristics.
| Hospital (n=155) | Transfer (n=230) | EMS (n=72) | P | Off-hours (n=291) | Normal working hours (n=166) | P | Total (n=457) | |
| Age (years) | 62.4±12.8 | 61.7±13.4 | 63.6±10.7 | .53 | 62.2±13 | 62.2±12.5 | .99 | 62.2±12.8 |
| Men | 121 (78.1) | 183 (79.6) | 60 (83.3) | .66 | 233 (80.1) | 131 (78.9) | .77 | 364 (79.6) |
| Smoking | 53 (34.2) | 112 (48.7) | 33 (45.8) | .02 a | 126 (43.3) | 72 (43.4) | .99 | 198 (43.3) |
| Hypertension | 81 (52.3) | 114 (49.6) | 42 (58.3) | .43 | 152 (52.2) | 85 (51.2) | .83 | 220 (48.1) |
| Dyslipidemia | 71 (45.8) | 108 (47.0) | 31 (43.1) | .84 | 139 (47.8) | 71 (42.8) | .3 | 210 (46) |
| Diabetes mellitus | 44 (27.1) | 54 (23.5) | 17 (23.6) | .71 | 75 (25.8) | 38 (22.9) | .5 | 113 (24.8) |
| Renal failure | 13 (8.4) | 10 (4.3) | 7 (9.7) | .15 | 19 (6.5) | 11 (6.6) | .97 | 30 (6.6) |
| Peripheral vascular disease | 28 (18.1) | 27 (11.7) | 12 (16.7) | .2 | 45 (15.5) | 22 (13.3) | .52 | 67 (14.7) |
| Previous AMI | 31 (20) | 14 (6.1) | 5 (6.9) | <.0001 b | 34 (11.7) | 16 (9.6) | .5 | 50 (10.9) |
| Previous PCI | 26 (17.3) | 14 (6.1) | 6 (8.5) | .003 c | 30 (10.3) | 16 (9.6) | .82 | 46 (10.1) |
| Previous coronary surgery | 5 (3.2) | 1 (0.4) | 0 | .03 d | 4 (1.4) | 2 (1.2) | .88 | 6 (1.3) |
| Anterior myocardial infarction | 62 (40) | 101 (43.9) | 30 (41.7) | .68 | 120 (41.2) | 73 (44) | .32 | 193 (42.2) |
| Killip III/IV | 16 (14.7) | 25 (10.9) | 7 (9.8) | .51 | 37 (12.7) | 17 (10.2) | .43 | 54 (11.9) |
| Use of anti-GPIIb/IIIa | 136 (87.7) | 196 (85.2) | 58 (80.6) | .36 | 246 (84.5) | 144 (86.7) | .52 | 390 (85.3) |
| Aspiration catheter | 111 (71.6) | 172 (74.8) | 60 (83.3) | .16 | 218 (74.9) | 125 (75.3) | .93 | 343 (75.1) |
| Drug-eluting stent | 51 (32.9) | 68 (29.6) | 22 (30.6) | .78 | 94 (32.3) | 47 (28.3) | .37 | 141 (30.9) |
| No. lesions treated per procedure | 1.46±0.8 | 1.35±0.7 | 1.35±0.6 | .3 | 1.43±0.8 | 1.31±0.5 | .04 | 1.39±0.7 |
| Stents per procedure | 1.38±0.9 | 1.35±0.7 | 1.35±0.6 | .93 | 1.38±0.9 | 1.33±0.6 | .43 | 1.36±0.8 |
| Multivessel intervention | 7 (4.5) | 11 (4.8) | 2 (2.8) | .76 | 13 (4.5) | 7 (4.2) | .9 | 20 (4.4) |
| LVEF (%) | 46.5±12.5 | 47.2±11.4 | 45.5±13 | .58 | 46±12.1 | 47.8±11.8 | .13 | 43.7±12 |
| Use of IAOBCP | 6 (3.9) | 5 (2.2) | 3 (4.2) | .54 | 11 (3.8) | 3 (1.8) | .22 | 14 (3.1) |
| Successful | 147 (94.8) | 214 (93) | 67 (93.1) | .35 | 271 (93.1) | 157 (94.6) | .9 | 428 (93.7) |
AMI, acute myocardial infarction; EMS, emergency medical service; IAOBCP, intraaortic balloon counterpulsation; LVEF, left ventricular ejection fraction; PCI, percutaneous coronary intervention.
Results are expressed as mean±standard deviation or n (%).
a Hospital versus transfer, P=.005; hospital versus EMS and transfer versus EMS, not significant.
b Hospital versus transfer, P<.0001; hospital versus EMS, P=.012; transfer versus EMS, not significant.
c Hospital versus transfer, P=.001; hospital versus EMS and transfer versus EMS, not significant.
d Hospital versus transfer, P=.04; hospital versus EMS and transfer versus EMS, not significant.
The mean age was 62 years and there was a predominance of men (79.6%). In all, 11.9% of the patients were Killip14 class III or IV at the time of the procedure. Radial access was the predominant approach (97%). The procedure was considered to be successful (final TIMI [Thrombolysis in Myocardial Infarction] flow15 grade 3 and residual stenosis less than 10%) in 93.7% of the cases. There was a higher proportion of patients with previous infarction, coronary artery surgery, or coronary interventional procedure and a lower proportion of smokers in the hospital group; there were no other significant differences with respect to patient characteristics.
The total in-hospital mortality rate was 4.8% and there were no significant differences between the 3 groups of patients (5.2%, 4.8% and 4.2%, respectively; P =.95).
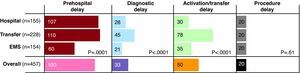
Care TimesThe different time intervals, overall and in each group, are summarized in Table 2 and Figure 2.
Table 2. Times and Delays According to Route by Which the Patient Arrived.
| Hospital (n=155) | Transfer (n=228) | EMS (n=72) | P | Hospital-EMS | Hospital-transfer | Transfer-EMS | Total (n=457) | |
| Prehospital delay | 107 [60-180] | 110 [49-182] | 60 [30-115] | .001 | .001 | .88 | <.0001 | 100 [45-176] |
| Diagnosis-related delay | 28 [13-53] | 45 [25-79] | 21 [10-33] | <.0001 | .07 | <.0001 | <.0001 | 33 [17-60] |
| Activation/transfer-related delay | 30 [14-39] | 78 [62-98] | 35 [30-45] | <.0001 | <.0001 | <.0001 | <.0001 | 50 [32-80] |
| Procedure-related delay | 20 [15-26] | 20 [16-25] | 20 [16-24] | .61 | .55 | .33 | .89 | 20 [16-25] |
| PA-related delay | 50 [39-62] | 99 [83-119] | 57 [49-64] | <.0001 | .004 | <.0001 | <.0001 | 74 [53-100] |
| Total ischemia time | 196 [130-305] | 266 [193-385] | 139 [107-206] | <.0001 | .001 | <.0001 | <.0001 | 220 [151-335] |
| Door-to-reperfusion time | 80 [63-107] | 148 [118-189] | 81 [66-98] | <.0001 | .86 | <.0001 | <.0001 | 108 [79-157] |
EMS, emergency medical system; PA, primary angioplasty.
The results are expressed as the median [interquartile range] in minutes.
Figure 2. Analysis of the different time intervals (median, in minutes) according to the route by which the patients arrived. Median length of delay expressed in minutes. EMS, emergency medical system.
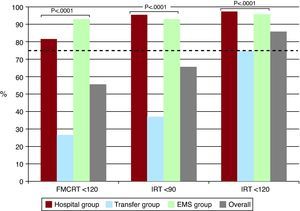
There was a prehospital delay of more than 2h in 60% of all cases (n=275): 55.8% in the hospital group, 56.7% in the transfer group, and 80.3% in the EMS group. The FMCRT was less than or equal to 120minutes in 55.5% of all cases (n=254): 80.8% of the hospital group, 26.8% of the transfer group, and 93% of the EMS group (P <.0001).
The PA-related delay was 74 [53-100] minutes. According to groups, it was 50 [39-62] minutes in the hospital group, 99 [83-119] minutes in the transfer group, and 57 [49-64] minutes in the EMS group (P <.0001) (Figure 3). The diagnostic delay was longer in the transfer group (45 [25-79] minutes versus 28 [13-53] minutes in the hospital group and 21 [10-33] minutes in the EMS group; P <.0001), as was the delay attributable to activation and/or transfer (78 [62-98] minutes versus 35 [30-45] minutes in the EMS group and 30 [14-39] minutes in the hospital group; P <.0001) and the FMCRT (148 [118-189] minutes versus 81 [66-98] minutes in the EMS group and 80 [63-107] minutes in the hospital group; P <.0001). There were no significant differences in the procedure-related delay in the 3 groups (P=.61).
Figure 3. Analysis of the time elapsed between the first medical contact and reperfusion and between the indication for primary angioplasty and reperfusion according to the route by which the patient arrived. The dashed line indicates 75% of the patients. EMS, emergency medical system; FMCRT, first medical contact-to-reperfusion time; IRT, indication-to-reperfusion time.
The total ischemia time was 220 [151-335] minutes. It was significantly shorter in the EMS group (139 [107-206] minutes versus 196 [130-305] minutes in the hospital group [P =.001] and 266 [193-385] minutes in the transfer group [P <.0001]).
Differences According to the Time of Day of the Performance of Primary AngioplastyWe found no significant differences in the FMCRT regardless of whether the procedure was carried out during normal working hours (166 patients) or during off-hours (291 patients), with FMCRT of 107 [74-155] minutes during normal working hours and of 109 [80-158] minutes during off-hours (P =.42). Again, there were no significant differences in the prehospital delay, diagnostic delay, delay attributable to activation and/or transfer, or total ischemia time. However, there was a difference in the procedure-related delay: 20 [16-25] minutes during off-hours and 19 [15-23] minutes during normal working hours (P =.02) (Table 3).
Table 3. Times and Delays According to the Time of Day of the Procedure.
| Off-hours (n=291) | Normal working hours (n=166) | P | Total (n=457) | |
| Prehospital delay | 105 [49-180] | 96 [35-161] | .39 | 100 [45-176] |
| Diagnosis-related delay | 35 [17-60] | 32 [15-62] | .92 | 33 [17-60] |
| Activation/transfer-related delay | 50 [35-77] | 54 [18-83] | .18 | 50 [32-80] |
| Procedure-related delay | 20 [16-25] | 19 [15-23] | .02 | 20 [16-25] |
| PA-related delay | 74 [55-100] | 75 [40-101] | .13 | 74 [53-100] |
| Total ischemia time | 235 [160-338] | 208 [135-333] | .35 | 220 [151-335] |
| Door-to-reperfusion time | 109 [80-158] | 107 [74-155] | .42 | 108 [79-157] |
PA, primary angioplasty.
The results are expressed as the median [interquartile range] in minutes.
In the present study, we demonstrate that the time to reperfusion differs depending on where the FMC takes place. However, we observed no differences according to whether the procedure is carried out during normal working hours or during off-hours. We have performed 290 PA per million population/year in our locality. This number is higher than the Spanish average (169 PA per million population/year, but lower than the European average (378 PA per million population/year). The Spanish autonomous communities in which the greatest numbers of procedures are performed are those, like Navarre (435 PA per million population/year), Galicia (318 PA per million population/year), the Basque Country (296 PA per million population/year), and Murcia (284 PA per million population/year), that participate in a structured PA program.16
Since June 2009, Catalonia has a STEMI treatment network, organized and coordinated by the Departament de Salut de la Generalitat de Catalunya (Department of Health of the Autonomous Government of Catalonia), which gives priority to the performance of PA in all of Catalonia (the so-called “Codi Infart”), and thus this number will probably increase until it is on a level with that of the other regions with similar programs. Future analyses will enable us to determine whether a well-structured regional PA network is capable of reducing some of the inappropriate delays identified in the present study.
Hospital GroupThe delay attributable to diagnosis was too long, lasting a median of 28minutes, and in 25% of the patients the diagnosis was delayed more than 53minutes. The diagnosis should be established within the first 20minutes after the FMC has taken place.17 Any patient presenting with chest pain must receive preferential attention, with priority on the performance and interpretation of an electrocardiogram (within the first 10 minutes). The creation of a specific unit for the assessment of chest pain has been shown to be of help in reducing the delays.18 Once the indication for PA had been established, the time to reperfusion (PA-related delay) was less than 1h in up to 75% of the patients.
Transfer GroupThe FMCRT was longer in these patients, only one fourth of whom were treated within the first 2h after the FMC, mainly due to a greater diagnostic delay and the time required for the transfer from the hospital in which PA could not be performed. The objective in these patients should also be to reach a diagnosis within 20minutes.
The median net delay attributable to the interhospital transfer was 48minutes longer than that recorded in the hospital group. Similar findings have recently been published for the PA network in the Italian region of Emilia-Romagna, where the FMCRT was 38minutes longer in the patients who required transfer.19
The length of the PA-related delay that can reduce the benefits of a percutaneous coronary intervention as compared to fibrinolytic therapy has been estimated to range between 60minutes20 and 120minutes.21, 22
In the 192 509 patients included in the National Registry of Myocardial Infarction (NRMI) 2-4,23 the mean delay for which the rate of mortality for the 2 strategies was the same was 114minutes. In this registry, it was also observed that this time period varied according to age, the duration of symptoms, and the site of the infarction. Trials specifically designed for the study of this subject have not been carried out and, thus, the a posteriori interpretation of the results of the analyses must be done with caution. In this situation, it is recommended that the decision to transfer the patient for treatment with PA or to administer fibrinolytic therapy be made on an individual basis. However, it appears to be reasonable that, once the diagnosis and indication have been established, the decision be made taking into account the delay associated with PA. The improvement in the coordination in transport introduced by the “Codi Infart” should, in the future, lead to a reduction in the time to reperfusion in patients being transferred to a PA center.
Emergency Medical System GroupIn these patients, the total ischemia time was reduced, mainly due to the shorter prehospital delay. In general, 60% of the patients arrived at our center within the first 2 h after the onset of symptoms, a percentage similar to that observed in earlier studies,24, 25 whereas in the EMS group, 50% arrived within the first 60minutes and 80%, within the first 2h.
In contrast to other recently published series, there was no significant decrease in the FMCRT in this group with respect to the hospital group; the major advantage in this group was a reduction in the total ischemia time, due, as mentioned above, to a shorter prehospital delay.17, 26, 27, 28 In these series, the interval was considered to commence with the arrival of the patient at the hospital, rather than the FMC, as defined and recommended in the guidelines.1 The reduction in the total ischemia time was not accompanied by a decrease in in-hospital mortality, probably because of the small sample size. However, early medical attention reduces the size of the infarction and can prevent fatal arrhythmic complications during the first hours after onset.29
Analysis of the Delays According to the Time at Which the Procedure Was PerformedIn our series, there were no differences in the FMCRT, regardless of whether the patient arrived during normal working hours or during off-hours. The analysis of a North American registry of over 100 000 patients treated with fibrinolysis or PA demonstrated that presentation during off-hours occurred with a greater frequency and was associated with longer periods of time in patients treated with PA, but not in those receiving fibrinolytic therapy, and that the mortality rate was higher in this group of patients.11 These findings coincide with those of another study from a North American center with a large population of patients with STEMI, which is why the authors pointed out the need for the physical presence of a PA team in the center 24h a day, 7 days a week.12
In Spain, the care times recorded in the APRIMUR registry for those patients who went directly to the PA center were not significantly different when normal working hours were compared with off-hours.30 Thus, in our country, the round-the-clock physical presence of a PA team does not appear to be necessary.
When all the time intervals analyzed were compared, there was only a slight, but significant, difference in the delay attributable to the procedure, with a better time profile during normal working hours. This finding is probably due to the fact that there are more personnel available at that time of day and thus the time required for the preparation and performance of the procedure is somewhat shorter.
Our study demonstrates that it is necessary to strengthen training and organizational strategies in order to optimize the time intervals and that we should make an effort to educate the population in the identification of the symptoms and to promote early medical attention by means of the EMS.
LimitationsThe time intervals were measured on the basis of the information provided by the patient or his or her relatives, the hospital admission records or the medical or nursing charts, and the direct reading of the time on the clock in the catheterization laboratory. The lack of synchronization among the different sources can induce an error in the measurement of the intervals.
In the patients receiving out-of-hospital care who went to a health center, which was a very small number, the FMC was considered to be the arrival of the EMS, rather than the time at which they were seen by the primary care physician. According to the European Society of Cardiology guidelines for the management of STEMI, the concept of FMC does not necessarily refer to the first professional that may attend to the patient, but the first who is capable of providing reperfusion therapy.1
One limitation to the study that could introduce a bias is the fact that we do not know the time of the electrocardiogram on which the indication for PA is based.
We have no data on the administration of fibrinolytics to the patients with STEMI in our region. In any case, the analysis of the data on PA time intervals from later reports in which this information was available has led us to think that the number of patients who received fibrinolytic therapy must have been low.
CONCLUSIONSThe patients transferred from other centers to undergo PA were subjected to longer delays in reperfusion than the other patients due to the time required for transfer and the greater diagnostic delay.
The time between the onset of the symptoms and reperfusion was shorter in those patients brought by the EMS, mainly because of the reduced prehospital delay.
There were no differences in treatment delay according to whether the patient arrived during normal working hours or during off-hours.
The detailed analysis of the time from onset of symptoms to reperfusion enables us to identify inappropriate delays and adopt measures to improve the efficiency of the system.
FUNDINGFunding for this study was provided by the Fondo de Investigación Sanitaria (FIS 07/0454).
Conflicts of interestNone declared.
Received 24 September 2010
Accepted 3 February 2011
Corresponding author: Unidad de Hemodinámica y Cardiología Intervencionista, Servicio de Cardiología, Hospital Universitari Germans Trias i Pujol, Ctra. de Canyet s/n, 08916 Badalona, Barcelona, Spain. oriolrodriguez@gmail.com