To estimate the percentage of heart failure patients in Spain that received the European Society of Cardiology recommended treatments, and in those that did not, to determine the reasons why.
MethodsThe study included 2834 consecutive ambulatory patients with heart failure from 27 Spanish hospitals. We recorded general information, the treatment indicated, and the reasons why it was not prescribed in some cases. In patients who met the criteria to receive a certain drug, true undertreatment was defined as the percentage of patients who, without justification, did not receive the drug.
ResultsIn total, 92.6% of ambulatory patients with low ejection fraction received angiotensin converting enzyme inhibitors or angiotensin receptor blockers, 93.3% beta-blockers, and 74.5% mineralocorticoid receptor antagonists. The true undertreatment rates were 3.4%, 1.8%, and 19.0%, respectively. Target doses were reached in 16.2% of patients receiving angiotensin converting enzyme inhibitors, 23.3% of those with angiotensin receptor blockers, 13.2% of those prescribed beta-blockers, and 23.5% of those with mineralocorticoid receptor antagonists. Among patients who could benefit from ivabradine, 29.1% received this drug. In total, 36% of patients met the criteria for defibrillator implantation and 90% of them had received the device or were scheduled for implantation, whereas 19.6% fulfilled the criteria for resynchronization therapy and 88.0% already had or would soon have the device. In patients who met the criteria, but did not undergo device implantation, the reasons were not cost-related.
ConclusionsWhen justified reasons for not administering heart failure drugs were taken into account, adherence to the guideline recommendations was excellent. Exclusive use of the percentage of treated patients is a poor indicator of the quality of healthcare in heart failure. Measures should be taken to improve the attainment of optimal dosing in each patient.
Keywords
Heart failure (HF) is a persistent health problem that places a significant burden on the health system and society in general and is anticipated to increase in the future.1
Certain treatments for this condition, some of which have been recently implemented,2,3 have proven effective for reducing HF events, particularly those leading to rehospitalization. Nonetheless, the incorporation of these advances in clinical practice tends to be slow. As a result, several studies investigating HF4,5 and other conditions6,7 have reported a discrepancy between the accepted approaches published in clinical practice guidelines and the activity seen in regular clinical practice. With regard to HF, the gap between recommendations and what is done in clinical practice is much smaller now than in previous years, after justified reasons for not administering a recommended therapy have been taken into account.8
The European Society of Cardiology (ESC) has developed an HF registry, the ESC Heart Failure Long-Term Registry,8 to which Spain makes a prominent contribution, with 28.4% of all patients included in Europe (3536 of 12 440). This registry provides a good opportunity to evaluate whether the treatment of hospitalized and ambulatory HF patients in Spain is performed in accordance with the European recommendations.3,9
Thus, the primary aim of this study was to estimate the percentage of HF patients attended in Spain who received the treatments recommended in the 2012 ESC guidelines, and, in those who did not, to determine the reasons why.
METHODSStudy Design and CentersThe ESC Heart Failure Long-Term Registry registry is a prospective, multicenter observational study performed in HF patients attending 211 cardiology centers in 21 ESC member countries in Europe and the Mediterranean area, including Spain.
The aim of ESC Heart Failure Long-Term Registry is to describe the clinical epidemiology of ambulatory and hospitalized patients with HF and to determine the diagnostic and therapeutic processes (including the organization of programs for HF management) applied in these patients over Europe as a whole and in the Mediterranean countries.
The registry was designed within the EORP (EURObservational Research Program) of the European Heart House of the ESC, and is coordinated by the EORP, which provides support to the related committees, national coordinators, and participating centers.10 Data are entered in a common electronic database that limits inconsistencies and errors and provides online help for key variables. Each center has access to its own data and each national coordinator has access to the data from all participating centers in that country.
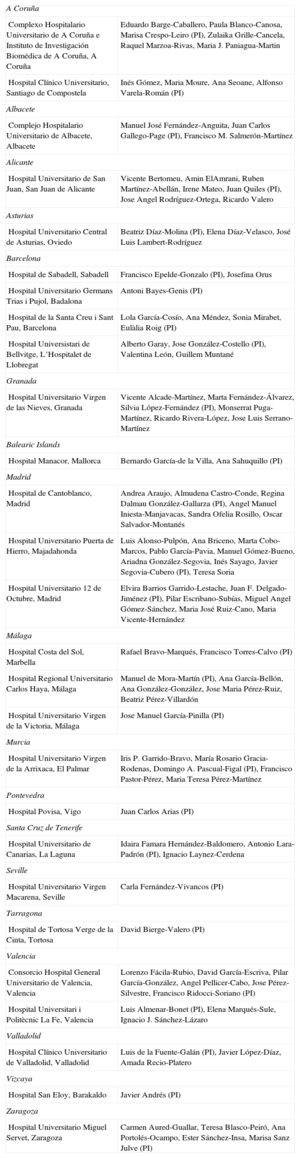
The number of centers participating in each country was determined according to the size of the population. Attempts were made to have a balanced geographical representation while taking into account the differing care levels of the cardiology departments treating HF patients. Centers were selected (Appendix) through each country's national cardiology society and HF section, as established for EORP registries and surveys.11
PatientsOn 1 day of the week over the 12 months of the inclusion period (April 2012-April 2013), each center included all HF patients older than 18 years attending the outpatient clinic and all those hospitalized on the same day for acute HF (either de novo HF or decompensation of a previous acute HF) with an intravenous therapy requirement (inotropic agents, vasodilators, or diuretics). Data collection was performed according to the criteria of the principal investigator of each center, and was usually carried out by personnel with no clinical activity assigned to the project.
A follow-up visit was scheduled at 1 year, either by personal interview or telephone contact (the data are not presented in this article). The present report includes only the ambulatory patients (chronic HF) recorded in the registry. In this population, the most robust recommendations in the 2012 ESC guidelines are for patients with HF and low ejection fraction (EF). An analysis was performed to determine whether these patients received the treatments recommended in the guidelines, specifically angiotensin-converting enzyme inhibitors (ACEI)/angiotensin receptor blockers (ARB), mineralocorticoid receptor antagonists (MRA), and ivabradine. Furthermore, the investigators recorded the dose of each drug given, and whether the dose used was the target dose established in clinical trials. In patients who did not receive these drugs and in those who did not attain the target dose, the reasons for these circumstances were analyzed.
The ESC Heart Failure Long-Term Registry has a quality assurance program that includes audits in around 10% of the participating centers, selected randomly. Two Spanish centers were audited in 2013.
The study was approved by the ethics committee of each center, and all patients gave informed consent for their inclusion.
Statistical AnalysisThe results for continuous variables are expressed as the median [first and third quartile] and the results for categorical variables as percentages. The analyses were performed centrally by support staff of the EORP Department of the European Heart House using SAS software (SAS Institute, Inc.; Cary, North Carolina, United States).
RESULTSThe results presented correspond to 2834 ambulatory patients (chronic HF group) recorded from Spanish centers. The results from the group of hospitalized patients (n=702 in Spain) are not included because the guideline recommendations for this population are based on a low level of evidence. The 27 hospitals participating in Spain included centers providing different levels of care: 19 centers offered the full range of cardiologic services, including interventional procedures (catheterization, cardiac resynchronization, defibrillator implantation) and cardiac surgery (in Spain, most of these centers also perform heart transplants); 4 centers provided interventional procedures, but not cardiac surgery; and 4 centers had cardiology units but did not carry out cardiac interventional procedures or cardiac surgery.
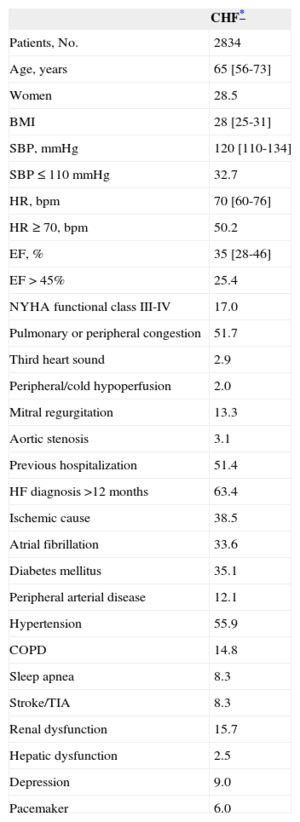
General CharacteristicsThe patients’ characteristics are summarized in Table 1. Patients included in the study were relatively young (half younger than 65 years), predominantly male, and only 1 of 4 patients had preserved EF (> 45%).
Baseline Patient Characteristics
| CHF* | |
|---|---|
| Patients, No. | 2834 |
| Age, years | 65 [56-73] |
| Women | 28.5 |
| BMI | 28 [25-31] |
| SBP, mmHg | 120 [110-134] |
| SBP ≤ 110 mmHg | 32.7 |
| HR, bpm | 70 [60-76] |
| HR ≥ 70, bpm | 50.2 |
| EF, % | 35 [28-46] |
| EF > 45% | 25.4 |
| NYHA functional class III-IV | 17.0 |
| Pulmonary or peripheral congestion | 51.7 |
| Third heart sound | 2.9 |
| Peripheral/cold hypoperfusion | 2.0 |
| Mitral regurgitation | 13.3 |
| Aortic stenosis | 3.1 |
| Previous hospitalization | 51.4 |
| HF diagnosis >12 months | 63.4 |
| Ischemic cause | 38.5 |
| Atrial fibrillation | 33.6 |
| Diabetes mellitus | 35.1 |
| Peripheral arterial disease | 12.1 |
| Hypertension | 55.9 |
| COPD | 14.8 |
| Sleep apnea | 8.3 |
| Stroke/TIA | 8.3 |
| Renal dysfunction | 15.7 |
| Hepatic dysfunction | 2.5 |
| Depression | 9.0 |
| Pacemaker | 6.0 |
BMI, body mass index; CHF, chronic heart failure; COPD, chronic obstructive pulmonary disease; EF, ejection fraction; HF, heart failure; HR, heart rate; NYHA: New York Heart Association functional class; SBP, systolic blood pressure; TIA, transient ischemic attack.
Unless otherwise indicated, the values express the percentage or the median [first and third quartile].
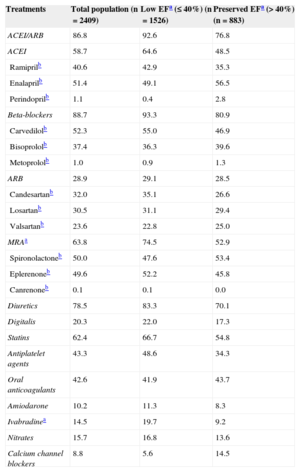
Angiotensin converting enzime inhibitors/ARB were prescribed in 86.8% of ambulatory patients, beta-blockers (BB) in 88.7%, and MRA in 63.8% (Table 2). In patients with low EF (EF ≤ 40% or ≤ 35% for MRA), which is the profile of patients deemed suitable to receive these treatments in the 2012 ESC guidelines, ACEI/ARB were prescribed in 92.6%, BB in 93.3%, and MRA in 74.5%. Furthermore, 65.4% (795/1.216) of patients with EF ≤ 35% were prescribed all 3 types of drugs (ACEI/ARB, BB, and MRA).
Pharmacological Treatment in Ambulatory Patients with Heart Failure
| Treatments | Total population (n=2409) | Low EFa (≤ 40%) (n=1526) | Preserved EFa (> 40%) (n=883) |
|---|---|---|---|
| ACEI/ARB | 86.8 | 92.6 | 76.8 |
| ACEI | 58.7 | 64.6 | 48.5 |
| Ramiprilb | 40.6 | 42.9 | 35.3 |
| Enalaprilb | 51.4 | 49.1 | 56.5 |
| Perindoprilb | 1.1 | 0.4 | 2.8 |
| Beta-blockers | 88.7 | 93.3 | 80.9 |
| Carvedilolb | 52.3 | 55.0 | 46.9 |
| Bisoprololb | 37.4 | 36.3 | 39.6 |
| Metoprololb | 1.0 | 0.9 | 1.3 |
| ARB | 28.9 | 29.1 | 28.5 |
| Candesartanb | 32.0 | 35.1 | 26.6 |
| Losartanb | 30.5 | 31.1 | 29.4 |
| Valsartanb | 23.6 | 22.8 | 25.0 |
| MRAa | 63.8 | 74.5 | 52.9 |
| Spironolactoneb | 50.0 | 47.6 | 53.4 |
| Eplerenoneb | 49.6 | 52.2 | 45.8 |
| Canrenoneb | 0.1 | 0.1 | 0.0 |
| Diuretics | 78.5 | 83.3 | 70.1 |
| Digitalis | 20.3 | 22.0 | 17.3 |
| Statins | 62.4 | 66.7 | 54.8 |
| Antiplatelet agents | 43.3 | 48.6 | 34.3 |
| Oral anticoagulants | 42.6 | 41.9 | 43.7 |
| Amiodarone | 10.2 | 11.3 | 8.3 |
| Ivabradinea | 14.5 | 19.7 | 9.2 |
| Nitrates | 15.7 | 16.8 | 13.6 |
| Calcium channel blockers | 8.8 | 5.6 | 14.5 |
ACEI, angiotensin converting enzyme inhibitors; ARB, angiotensin receptor blockers; MRA, mineralocorticoid receptor antagonists; EF, ejection fraction. Data are expressed as percentage.
As to ivabradine, 70.9% of ambulatory patients (249/351) with sinus rhythm, EF ≤ 35%, and heart rate ≥ 70 bpm did not receive ivabradine, and in this same subgroup, only 21.6% of patients (76/351) were prescribed all 4 types of drugs (ACEI/ARB, BB, MRA, and ivabradine).
In a large proportion of the patients not prescribed the treatments recommended in the guidelines (ACEI/ARB, BB, and MRA), there was a justification for doing so. The distribution of ambulatory patients with low EF (≤ 40%) according to whether or not they received each of the 3 main drug classes is shown in Figure 1, and in those who did not receive these drugs, the reasons for not doing so are listed. In patients who were not prescribed each of the treatments, the true underprescription rates—that is, the percentage of patients not prescribed a treatment and with no recorded justification—were 3.4% for ACEI/ARB, 1.8% for BB, and 19.0% for MRA.
Reason why recommended treatments were not used in patients (n=1526) with low ejection fraction (≤ 40%). ARB, angiotensin receptor blockers; ACEI, angiotensin converting enzyme inhibitors; MRA, mineralocorticoid receptor antagonists; COPD, chronic obstructive pulmonary disease; HF, heart failure.
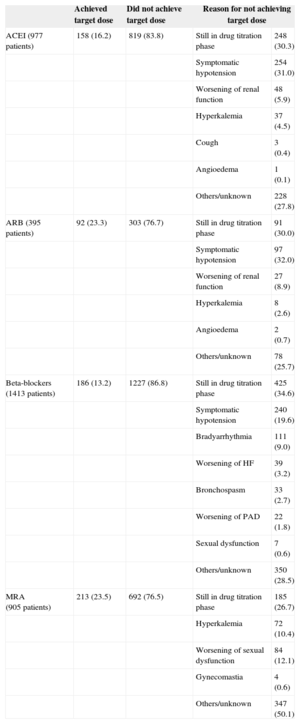
Only a small percentage of ambulatory patients with a low EF reached the target doses reported in clinical trials using these drugs: 16.2% of those receiving ACEI, 23.3% of those with ARB, 13.2% of patients with BB, and 23.5% of patients receiving MRA (Table 3). There was often a clinical reason indicating that the dose prescribed was optimal for the patient, but in at least 1 of 4 patients (1 of 2 in the case of MRA), no justification was recorded.
Attainment of the Target Dose in Recommended Treatments for Ambulatory Patients With Low Ejection Fraction
| Achieved target dose | Did not achieve target dose | Reason for not achieving target dose | ||
|---|---|---|---|---|
| ACEI (977 patients) | 158 (16.2) | 819 (83.8) | Still in drug titration phase | 248 (30.3) |
| Symptomatic hypotension | 254 (31.0) | |||
| Worsening of renal function | 48 (5.9) | |||
| Hyperkalemia | 37 (4.5) | |||
| Cough | 3 (0.4) | |||
| Angioedema | 1 (0.1) | |||
| Others/unknown | 228 (27.8) | |||
| ARB (395 patients) | 92 (23.3) | 303 (76.7) | Still in drug titration phase | 91 (30.0) |
| Symptomatic hypotension | 97 (32.0) | |||
| Worsening of renal function | 27 (8.9) | |||
| Hyperkalemia | 8 (2.6) | |||
| Angioedema | 2 (0.7) | |||
| Others/unknown | 78 (25.7) | |||
| Beta-blockers (1413 patients) | 186 (13.2) | 1227 (86.8) | Still in drug titration phase | 425 (34.6) |
| Symptomatic hypotension | 240 (19.6) | |||
| Bradyarrhythmia | 111 (9.0) | |||
| Worsening of HF | 39 (3.2) | |||
| Bronchospasm | 33 (2.7) | |||
| Worsening of PAD | 22 (1.8) | |||
| Sexual dysfunction | 7 (0.6) | |||
| Others/unknown | 350 (28.5) | |||
| MRA (905 patients) | 213 (23.5) | 692 (76.5) | Still in drug titration phase | 185 (26.7) |
| Hyperkalemia | 72 (10.4) | |||
| Worsening of sexual dysfunction | 84 (12.1) | |||
| Gynecomastia | 4 (0.6) | |||
| Others/unknown | 347 (50.1) | |||
ACEI, angiotensin converting enzyme inhibitors; ARB, angiotensin receptor blockers; HF, heart failure; MRA, mineralocorticoid receptor antagonists; PAD, peripheral arterial disease. Data are expressed as No. (%).
Figure 2 shows the distribution of ambulatory patients according to whether or not they had an indication for defibrillator implantation or cardiac resynchronization therapy, whether they already had a device, and the reasons why they did not have a device despite having an indication for one. In total, 64.0% of patients did not fulfill the guidelines’ criteria for defibrillator implantation and 80.4% did not meet the criteria for cardiac resynchronization therapy. Among patients with criteria for defibrillation, 78% (788 of 1016) already had defibrillators and an additional 12% were in the planning process for defibrillator implantation. In patients with an indication for resynchronization therapy, 74% (406 of 549) already had a pacemaker and 14% (76 of 549) were in the planning process. In patients who met the criteria but were not considered for device implantation (10% for defibrillators and 12% for resynchronization), the main reason for this circumstance was uncertainty about the indication.
DISCUSSIONThis study brings to light the focus of HF treatment on meeting the requirements of individual patients. Furthermore, it shows that simple calculation of the percentage of treated patients may not be an appropriate measure to indicate the quality of the healthcare provided in a specific condition. Compared with previous reports, this study has the added value of careful, comprehensive collection of the treatments and doses administered in the population examined, as well as the reasons why indicated drugs were not prescribed or the doses given did not reach the targets defined in clinical studies. A previous estimation from the European Heart Failure Pilot Survey, ESC-HF Pilot,11 which described only the number of patients treated, reported administration of ACEI/ARB, BB, and MRA in 88.5%, 86.7%, and 43.7% of patients, respectively. In contrast, when justified reasons for not prescribing a certain treatment were taken into account, we found that the true problem of undertreatment in Spain is practically inconsequential with regard to ACEI/ARB and BB (3.4% and 1.8%), whereas there is still a wide margin for improvement in MRA prescription (true undertreatment in 19.0%).
Another observation highlighted by this study has important implications for clinical practice. We found that compliance with the guidelines regarding treatment indications has improved considerably compared with the situation 10 years ago. At that time, Spain showed the lowest use of BB and ACEI (around 10% and 40%, respectively) among all the participating European countries,12 whereas the current prescription of recommended HF treatments is excellent (with the possible exception of MRA). Nonetheless, this improvement was not seen in attainment of the doses defined in clinical trials, as most patients did not receive the target doses of the treatments indicated. In a large percentage of these patients, there was a sound reason for this situation: dosing was in the adjustment phase or there were toxicity symptoms indicating that the maximum dose tolerated had been reached. Therefore, many of these patients were actually receiving their optimal dose; that is, the maximum “possible dose” even though it may not have been the “target dose”. Despite these findings, in 1 of every 4 patients (1 of 2 in the case of MRA), no reason was given for the lower doses. These percentages should be considered the worst-case scenario according to the available information. Even in a high-quality registry carried out meticulously, the reasons for lower dosing might not be available to the person collecting this information in each center because of the nature of the HF treatment process (performed by several professionals over time, working in different settings). Another factor that could have made a substantial contribution to the gap between our results and the target doses is the difficulty of establishing rigorous programs for dose titration of HF drugs. Dose adjustment implies numerous visits and laboratory analyses to carefully tailor the treatment to the patient's requirements. It would be of particular value if our patients could be attended when and where they need these visits, and not simply according to the availability of regular care, which is necessarily restricted. This is a limitation that hinders proper use of our therapeutic resources and it underscores the need to establish integrated programs that go beyond the hospital setting and include health professionals of several types (eg, specialized physicians in the hospital and community, specialized nurses).13
This study has an advantage over other registries in Spain, some of them quite recent,4,14,15 in that it allows direct comparison with other data in the European registry, of which it forms a part. All contributors to this cornerstone project of the ESC use identical methods. Furthermore, it is an active registry that continues to include patients and their follow-up. The situation regarding the true undertreatment rates in Spain is virtually the same as that reported for the overall European study8 (including Spanish centers). However, although the percentage of patients reaching the target doses established in clinical trials is rather low throughout Europe, it is slightly lower in Spain.3
As to the more recently available HF drugs such as ivabradine, it seems that their incorporation has been faster in Spain than in Europe as a whole, in both patients with low EF (19.7% vs 10.5%) and in the overall cohort of ambulatory patients (14.5% vs 8.5%).8 Of note, however, in the subanalysis of ivabradine use in Spain, low EF was defined as ≤ 35%, whereas in the overall European analysis it was ≤ 45%.8 In a Spanish study in ambulatory patients conducted approximately 1 year before these results, only 7.2% of patients received this drug.16 Despite the current improvement, the percentage of patients in Spain who meet the criteria for ivabradine treatment but are not prescribed this drug remains high: only 29.1% of ambulatory patients with sinus rhythm, EF ≤ 35%, and heart rate ≥ 70 bpm received this medication, again reflecting the delay between demonstration of the benefits of a specific intervention and its incorporation into clinical practice. This aspect should be reassessed in the future. In contrast to other drugs, ivabradine was incorporated for the first time in the 2012 guidelines, which were published at the same time as the start of data collection for the registry in Spain. Information on adherence to the guidelines for this medication throughout Europe has not yet been published, which prevents direct comparison in the subgroup of patients in whom the guidelines recommend its use.
As regards device use, it seems that the reasons why patients with indications for these devices did not receive them are not exclusively economic, despite the economic crisis. It is possible that physicians themselves may be managing resource use while keeping in mind the existing economic difficulties, but this would have very different implications than if devices were not being implanted for purely economic reasons.
LimitationsSome of the potential limitations of this study have been mentioned in other sections of the discussion. The main limitation is that with the available data it is impossible to assure that case recording was complete in all the participating Spanish centers. Some hospitals included fewer patients than others of the same size and care level, although this occurred in very few centers. Huge efforts have been made to simplify the protocol and improve the possibility of including all consecutive patients seen on the registry days. Although complete recording has not been confirmed in all centers, the audits performed in 2 Spanish hospitals indicated good compliance with the study protocol (unpublished data, personal report from the EORP staff). As a reflection that case recording was good in our centers, Spain was the country with the largest number of patients included in the registry among all participants. Another possible limitation lies in the procedure for selecting participating centers, which was not done randomly. Among the centers interested in participating, a larger number of tertiary-level hospitals were included than those recommended by the protocol,11 which resulted in the participation of fewer lower-level centers. This reflects the organization of HF care in Spain: lower-level centers may not have HF units, and care for these patients is often delegated to internal medicine specialists rather than cardiologists, who mainly perform complementary testing. We believe that the final list reflects the varying profile of Spanish centers in which cardiologists are responsible for the care of HF patients and that it is geographically representative, in case this factor might be important in the estimations made. The design of the database and the software for data entry, which, for example, had online information about recommended dosing, guarantee high-quality data and enable examination of aspects that have not been thoroughly investigated to date, such as the reasons why target doses were not reached.
In summary, after taking into consideration justified reasons for not prescribing drugs to patients with low EF, compliance with the guidelines was excellent in Spain. Simple estimation of the percentage of patients treated is a poor quality indicator of HF care. The focus should be changed from emphasis on the indications for treatments to the introduction of measures that will improve the attainment of optimal doses for each patient (taking into account the maximum tolerated dose according to clinical, hemodynamic, and/or toxicity-related factors). The continuous updating of the registry makes it a magnificent instrument for monitoring HF treatment in Spain and enables comparison with the situation in the rest of Europe in order to identify strengths and weaknesses17 and design improvements where necessary.
CONFLICTS OF INTERESTNone declared.
Many of the participating investigators and centers are part of the Cardiovascular Research Network of Carlos III Institute of Health (Red de Investigación Cardiovascular [RIC] of the Instituto de Salud Carlos III).
Servier España contributed unconditional grant funding for the development of the registry in Spain through an agreement with the Heart Failure and Cardiac Transplantation Section of the Spanish Society of Cardiology.
We thank Javier Muñiz for his contribution in writing the first drafts of the manuscript.
We are grateful to the following members of the European Heart House EORP: Cecile Laroche (statistical analysis), Gerard Gracia (data monitor), Emanuela Fiorucci (project head), Aldo P. Maggioni (scientific coordinator), and Thierry Ferreira (head of department).
| A Coruña | |
| Complexo Hospitalario Universitario de A Coruña e Instituto de Investigación Biomédica de A Coruña, A Coruña | Eduardo Barge-Caballero, Paula Blanco-Canosa, Marisa Crespo-Leiro (PI), Zulaika Grille-Cancela, Raquel Marzoa-Rivas, Maria J. Paniagua-Martin |
| Hospital Clínico Universitario, Santiago de Compostela | Inés Gómez, Maria Moure, Ana Seoane, Alfonso Varela-Román (PI) |
| Albacete | |
| Complejo Hospitalario Universitario de Albacete, Albacete | Manuel José Fernández-Anguita, Juan Carlos Gallego-Page (PI), Francisco M. Salmerón-Martínez |
| Alicante | |
| Hospital Universitario de San Juan, San Juan de Alicante | Vicente Bertomeu, Amin ElAmrani, Ruben Martínez-Abellán, Irene Mateo, Juan Quiles (PI), Jose Angel Rodríguez-Ortega, Ricardo Valero |
| Asturias | |
| Hospital Universitario Central de Asturias, Oviedo | Beatriz Díaz-Molina (PI), Elena Díaz-Velasco, José Luis Lambert-Rodríguez |
| Barcelona | |
| Hospital de Sabadell, Sabadell | Francisco Epelde-Gonzalo (PI), Josefina Orus |
| Hospital Universitario Germans Trias i Pujol, Badalona | Antoni Bayes-Genis (PI) |
| Hospital de la Santa Creu i Sant Pau, Barcelona | Lola García-Cosío, Ana Méndez, Sonia Mirabet, Eulàlia Roig (PI) |
| Hospital Universistari de Bellvitge, L’Hospitalet de Llobregat | Alberto Garay, Jose González-Costello (PI), Valentina León, Guillem Muntané |
| Granada | |
| Hospital Universitario Virgen de las Nieves, Granada | Vicente Alcade-Martínez, Marta Fernández-Álvarez, Silvia López-Fernández (PI), Monserrat Puga-Martínez, Ricardo Rivera-López, Jose Luis Serrano-Martínez |
| Balearic Islands | |
| Hospital Manacor, Mallorca | Bernardo García-de la Villa, Ana Sahuquillo (PI) |
| Madrid | |
| Hospital de Cantoblanco, Madrid | Andrea Araujo, Almudena Castro-Conde, Regina Dalmau González-Gallarza (PI), Angel Manuel Iniesta-Manjavacas, Sandra Ofelia Rosillo, Oscar Salvador-Montanés |
| Hospital Universitario Puerta de Hierro, Majadahonda | Luis Alonso-Pulpón, Ana Briceno, Marta Cobo-Marcos, Pablo García-Pavia, Manuel Gómez-Bueno, Ariadna González-Segovia, Inés Sayago, Javier Segovia-Cubero (PI), Teresa Soria |
| Hospital Universitario 12 de Octubre, Madrid | Elvira Barrios Garrido-Lestache, Juan F. Delgado-Jiménez (PI), Pilar Escribano-Subías, Miguel Angel Gómez-Sánchez, Maria José Ruiz-Cano, Maria Vicente-Hernández |
| Málaga | |
| Hospital Costa del Sol, Marbella | Rafael Bravo-Marqués, Francisco Torres-Calvo (PI) |
| Hospital Regional Universitario Carlos Haya, Málaga | Manuel de Mora-Martín (PI), Ana García-Bellón, Ana González-González, Jose Maria Pérez-Ruiz, Beatriz Pérez-Villardón |
| Hospital Universitario Virgen de la Victoria, Málaga | Jose Manuel García-Pinilla (PI) |
| Murcia | |
| Hospital Universitario Virgen de la Arrixaca, El Palmar | Iris P. Garrido-Bravo, María Rosario Gracia-Rodenas, Domingo A. Pascual-Figal (PI), Francisco Pastor-Pérez, Maria Teresa Pérez-Martínez |
| Pontevedra | |
| Hospital Povisa, Vigo | Juan Carlos Arias (PI) |
| Santa Cruz de Tenerife | |
| Hospital Universitario de Canarias, La Laguna | Idaira Famara Hernández-Baldomero, Antonio Lara-Padrón (PI), Ignacio Laynez-Cerdena |
| Seville | |
| Hospital Universitario Virgen Macarena, Seville | Carla Fernández-Vivancos (PI) |
| Tarragona | |
| Hospital de Tortosa Verge de la Cinta, Tortosa | David Bierge-Valero (PI) |
| Valencia | |
| Consorcio Hospital General Universitario de Valencia, Valencia | Lorenzo Fácila-Rubio, David García-Escriva, Pilar García-González, Angel Pellicer-Cabo, Jose Pérez-Silvestre, Francisco Ridocci-Soriano (PI) |
| Hospital Universitari i Politècnic La Fe, Valencia | Luis Almenar-Bonet (PI), Elena Marqués-Sule, Ignacio J. Sánchez-Lázaro |
| Valladolid | |
| Hospital Clínico Universitario de Valladolid, Valladolid | Luis de la Fuente-Galán (PI), Javier López-Díaz, Amada Recio-Platero |
| Vizcaya | |
| Hospital San Eloy, Barakaldo | Javier Andrés (PI) |
| Zaragoza | |
| Hospital Universitario Miguel Servet, Zaragoza | Carmen Aured-Guallar, Teresa Blasco-Peiró, Ana Portolés-Ocampo, Ester Sánchez-Insa, Marisa Sanz Julve (PI) |
PI, principal investigator.