There is debate regarding the prognostic significance of the absence of significant coronary lesions in patients with non—ST-segment elevation acute myocardial infarction. We investigated long-term prognosis in a contemporary cohort of these patients.
MethodsRetrospective observational study of 5203 patients with acute coronary syndrome. Propensity score matching was used to create 2 groups of 367 patients with non—ST-segment elevation acute myocardial infarction matched by the absence or presence of significant coronary lesions. In the matched cohort, we determined the impact of the absence of significant coronary lesions on mortality or readmission for acute coronary syndrome for 4.8 (2.6) years after discharge.
ResultsMortality or readmission for acute coronary syndrome was lower among patients without significant lesions (26.4% vs 32.7%; P = .09). Mortality in both groups was 19.1%. In contrast, patients without significant lesions had a lower incidence of readmission for acute coronary syndrome (2.0/100 vs 3.9/100 person-years; P = .003). The incidence of mortality or readmission for acute coronary syndrome was similar in patients without significant lesions and those with significant 1-vessel disease (26.4% vs 27.5%; P = .19), but lower than that in patients with 2-vessel disease (37.8%; P = .007) and 3-vessel disease or left main coronary artery disease (41.1%; P = .002).
ConclusionsPatients with non—ST-segment elevation acute myocardial infarction and coronary arteries without significant lesions have similar long-term mortality but lower readmission rates for acute coronary syndrome than patients with significant lesions. Mortality or readmission for acute coronary syndrome is similar in patients without significant lesions and patients with 1-vessel disease, but lower than in patients with disease in 2 or more vessels.
Keywords
Complex coronary atherosclerosis is the common pathological substrate of acute coronary syndrome (ACS). However, angiographic studies have shown that a considerable number of patients with non—ST-segment elevation acute coronary syndrome lack significant obstructive coronary lesions.1–3
Several pathophysiological theories have been advanced to explain this phenomenon, including abnormal coronary flow reserve due to macrovascular or microvascular dysfunction, rupture or erosion of atherosclerotic plaques with spontaneous lysis of the thrombus, and other noncoronary causes of myocardial damage.4–8
Non—ST-segment elevation acute coronary syndrome is often a diagnostic and therapeutic challenge to the clinician. Furthermore, there is no consensus on whether coronary angiography alone is an effective tool to define risk in this group of patients, regardless of clinical stratification.3,9–12
The aim of this study was to investigate the long-term outcome of a cohort of patients with non—ST-segment elevation acute myocardial infarction (NSTEMI) and with no significant coronary lesions (nSCL) by angiography.
METHODSStudy PopulationA retrospective cohort study based on the CardioCHUS registry, which included all consecutive patients admitted with a diagnosis of ACS to the Servicio de Cardiología of the Complejo Hospitalario Universitario de Santiago de Compostela (coronary care unit, intermediate care unit, and hospitalization ward) from December 2003 to September 2012 (n = 5532).
Figure 1 shows the patient selection flowchart. Firstly, patients with an incorrect diagnosis of ACS were excluded as well as those with ACS precipitated by a secondary cause: severe anemia (hemoglobin < 7 g/dL), recent surgery, sepsis, substance abuse, or CO poisoning. Subsequently, patients with ST-segment elevation acute myocardial infarction were excluded because its prognosis differs from that of NSTEMI.
Patient selection flowchart. ACS, acute coronary syndrome; AMI, acute myocardial infarction; CABG, coronary artery bypass graft; NSTEACS, non—ST-segment elevation acute coronary syndrome; NSTEMI, non—ST-segment elevation acute myocardial infarction; STEMI, ST-segment elevation acute myocardial infarction; PCI, percutaneous coronary intervention.
Given that the aim was to study long-term prognosis, patients who did not survive the hospital phase were also excluded. Patients who die at this stage have different characteristics and their inclusion would alter the analysis of results of follow-up after hospital discharge. In addition, patients who did not undergo coronary angiography during admission were excluded as well as patients with a history of coronary artery bypass surgery or percutaneous coronary intervention due to the difficulty involved in establishing the presence and severity of coronary lesions in these patients. Patients with a diagnosis of unstable angina were also excluded to minimize sample heterogeneity. Finally, 43 patients were excluded due to the lack of follow-up data following discharge.
Thus, the final cohort consisted of 1883 patients with a definite diagnosis of NSTEMI.
Non—ST-segment elevation acute myocardial infarction was defined by symptoms consistent with myocardial ischemia, the absence of persistent ST-segment elevation on the initial electrocardiogram, and cardiac troponin I above the upper boundary of the normal reference range (Flex® reagent cartridges, Dimension® system, Siemens®, Inc.; United States).
The patients were classified into 2 groups based on the presence or absence of stenotic lesions ≥ 70% visually assessed at the discretion of the attending cardiologist. This percentage is equivalent to 50% stenosis as assessed using quantitative analysis.13 Lesions of the left main coronary artery (LCA) were considered significant if they were ≥ 50%.
The study was conducted according to the principles of the Declaration of Helsinki.
Objective and Follow-upThe primary aim was to evaluate the prognostic effect of the absence of significant coronary lesions on the composite event of death and readmission for ACS (reACS).
The secondary objective was to determine mortality and reACS. After discharge, patients were followed up in a specialized ischemic heart disease clinic and primary care center. Structured follow-up was conducted by using electronic records (exclusively in the autonomous community of Galicia, IANUS program), reviewing medical care reports and hospital records, and contacting the patient by phone if needed. Mean follow-up was 4.8 (2.6) years.
Statistical AnalysisQuantitative variables are expressed as mean (standard deviation) and categorical variables as number (percentage). Prior to propensity score matching, the chi-square test or Fisher exact test were used to compare qualitative variables in the pre-matching cohort.
Given the nonrandomized nature of the study and the multiple biases that could have influenced the prognosis of patients with nSCL, propensity score matching was performed to minimize the bias inherent to observational studies. Firstly, the propensity score was used to assess the probability of each patient having nSCL, according to baseline characteristics. Propensity score matching was then performed to match the characteristics of the groups by defined variables such that the effect of a factor or intervention could be analyzed. We used a 1:1 protocol without replacement, and calipers of width equal to 0.1 of the standard deviation of the logit of the propensity score.
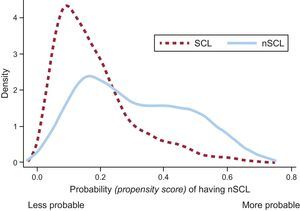
Propensity score matching was performed using binary logistic regression in which the dependent variable was nSCL and the explanatory variables were age, sex, diabetes mellitus, smoking, hypertension, peripheral artery disease, previous myocardial infarction, previous atrial fibrillation, peak troponin I, ST deviation (ST depression ≥ 0.5mm or transient ST elevation), serum creatinine, hemoglobin, heart rate, and Killip class. Two groups of 367 patients were created, matched by the presence or absence of significant coronary lesions. The predictive power of the model used to generate the propensity score was 0.74 (95% confidence interval [95% CI], 0.72-0.77; P < .001] and the model was well-calibrated (Hosmer-Lemeshow test, P = .68). Figure 2 shows the degree of propensity score overlap between the groups.
Survival analyses were performed for the matched cohort. The Kaplan-Meier method was used to construct survival curves and event-free survival curves for the composite of reACS or death, and stratified log rank test for the purposes of comparison. Subsequently, a Cox regression model was constructed that included nSCL as the explanatory variable. Given its nature, the matched sample was stratified by the estimates obtained by Cox regression according to the variable that identified each pair of the 367 pairs of patients.
Cumulative incidence curves were plotted to analyze reACS-free survival, and the Gray test was used to analyze differences between groups. A Fine and Gray competing risks (death and reACS) regression model was used to determine the effect of the explanatory variable on the risk of reACS.14
Within the group of patients with significant lesions, differences were found in the prognosis and in the severity and extent of coronary artery disease (1-, 2-, and 3-vessel disease or LCA disease). To better understand the impact of coronary arteries with and without significant lesions, the GRACE score15 was used to adjust the survival models to compare the incidence of the primary and secondary objectives in the 2 subgroups, according to the severity and extent of coronary artery disease, as defined above. The Schoenfeld residuals test was used to test the proportional hazard assumption.
In the case of reACS, the jackknife technique with 350 repetitions was used to calculate the statistical significance of the P values and to estimate HR (hazard ratio) or sHR (subhazard ratio) and their respective 95%CI. Statistical analyses were performed using the SPSS 21 and STATA 13 software packages. P value < .05 was used as a cutoff value for statistical significance.
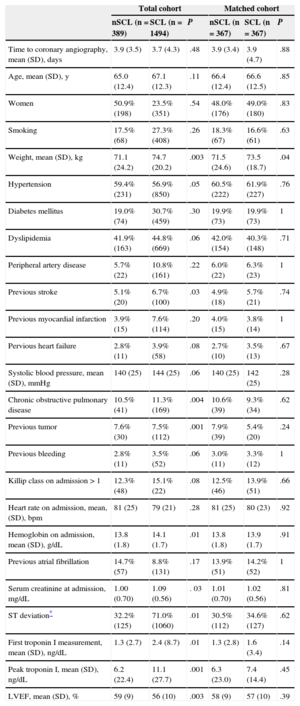
RESULTSBaseline CharacteristicsThe patients in the group with nSCL were younger and more often women (Table 1). They also had a lower prevalence of smoking, diabetes mellitus, peripheral artery disease, and prior myocardial infarction, but higher percentage of history of atrial fibrillation. Among these patients, ST deviation and peak troponin I were lower. There was no significant change in the proportion of these patients between December 2003 and September 2012: 2003-2006, 19.5%; 2007-2009, 20.9%; and 2010-2012, 22.2% (P = .61).
Baseline Characteristics Stratified by the Presence or Absence of Significant Coronary Lesions in the Total Cohort and the Matched Cohorts
| Total cohort | Matched cohort | |||||
|---|---|---|---|---|---|---|
| nSCL (n = 389) | SCL (n = 1494) | P | nSCL (n = 367) | SCL (n = 367) | P | |
| Time to coronary angiography, mean (SD), days | 3.9 (3.5) | 3.7 (4.3) | .48 | 3.9 (3.4) | 3.9 (4.7) | .88 |
| Age, mean (SD), y | 65.0 (12.4) | 67.1 (12.3) | .11 | 66.4 (12.4) | 66.6 (12.5) | .85 |
| Women | 50.9% (198) | 23.5% (351) | .54 | 48.0% (176) | 49.0% (180) | .83 |
| Smoking | 17.5% (68) | 27.3% (408) | .26 | 18.3% (67) | 16.6% (61) | .63 |
| Weight, mean (SD), kg | 71.1 (24.2) | 74.7 (20.2) | .003 | 71.5 (24.6) | 73.5 (18.7) | .04 |
| Hypertension | 59.4% (231) | 56.9% (850) | .05 | 60.5% (222) | 61.9% (227) | .76 |
| Diabetes mellitus | 19.0% (74) | 30.7% (459) | .30 | 19.9% (73) | 19.9% (73) | 1 |
| Dyslipidemia | 41.9% (163) | 44.8% (669) | .06 | 42.0% (154) | 40.3% (148) | .71 |
| Peripheral artery disease | 5.7% (22) | 10.8% (161) | .22 | 6.0% (22) | 6.3% (23) | 1 |
| Previous stroke | 5.1% (20) | 6.7% (100) | .03 | 4.9% (18) | 5.7% (21) | .74 |
| Previous myocardial infarction | 3.9% (15) | 7.6% (114) | .20 | 4.0% (15) | 3.8% (14) | 1 |
| Pervious heart failure | 2.8% (11) | 3.9% (58) | .08 | 2.7% (10) | 3.5% (13) | .67 |
| Systolic blood pressure, mean (SD), mmHg | 140 (25) | 144 (25) | .06 | 140 (25) | 142 (25) | .28 |
| Chronic obstructive pulmonary disease | 10.5% (41) | 11.3% (169) | .004 | 10.6% (39) | 9.3% (34) | .62 |
| Previous tumor | 7.6% (30) | 7.5% (112) | .001 | 7.9% (39) | 5.4% (20) | .24 |
| Previous bleeding | 2.8% (11) | 3.5% (52) | .06 | 3.0% (11) | 3.3% (12) | 1 |
| Killip class on admission > 1 | 12.3% (48) | 15.1% (22) | .08 | 12.5% (46) | 13.9% (51) | .66 |
| Heart rate on admission, mean, (SD), bpm | 81 (25) | 79 (21) | .28 | 81 (25) | 80 (23) | .92 |
| Hemoglobin on admission, mean (SD), g/dL | 13.8 (1.8) | 14.1 (1.7) | .01 | 13.8 (1.8) | 13.9 (1.7) | .91 |
| Previous atrial fibrillation | 14.7% (57) | 8.8% (131) | .17 | 13.9% (51) | 14.2% (52) | 1 |
| Serum creatinine at admission, mg/dL | 1.00 (0.70) | 1.09 (0.56) | . 03 | 1.01 (0.70) | 1.02 (0.56) | .81 |
| ST deviation* | 32.2% (125) | 71.0% (1060) | .01 | 30.5% (112) | 34.6% (127) | .62 |
| First troponin I measurement, mean (SD), ng/dL | 1.3 (2.7) | 2.4 (8.7) | .01 | 1.3 (2.8) | 1.6 (3.4) | .14 |
| Peak troponin I, mean (SD), ng/dL | 6.2 (22.4) | 11.1 (27.7) | .001 | 6.3 (23.0) | 7.4 (14.4) | .45 |
| LVEF, mean (SD), % | 59 (9) | 56 (10) | .003 | 58 (9) | 57 (10) | .39 |
LVEF, left ventricular ejection fraction; nSCL, no significant coronary lesions; SCL, significant coronary lesions; SD, standard deviation.
Adjusting for the propensity score yielded 367 patients in each matched group. Table 1 shows the baseline characteristics of the total cohort and the matched cohort.
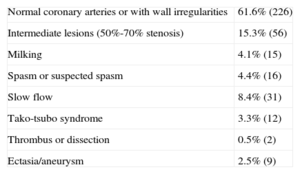
Table 2 shows the specific angiographic diagnoses within the nSCL group: 61.6% had normal coronary arteries or wall irregularities and 15.3% had intermediate lesions (50%-70% stenosis).
Specific Diagnoses Within the Group of Patients (N = 367) With the Generic Diagnosis of Coronary Arteries Without Significant Lesions
| Normal coronary arteries or with wall irregularities | 61.6% (226) |
| Intermediate lesions (50%-70% stenosis) | 15.3% (56) |
| Milking | 4.1% (15) |
| Spasm or suspected spasm | 4.4% (16) |
| Slow flow | 8.4% (31) |
| Tako-tsubo syndrome | 3.3% (12) |
| Thrombus or dissection | 0.5% (2) |
| Ectasia/aneurysm | 2.5% (9) |
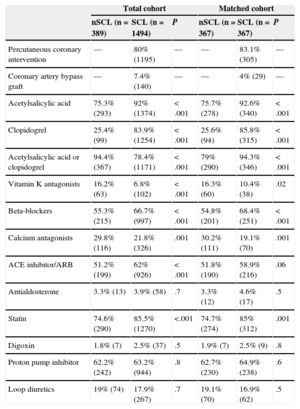
Table 3 shows treatment at discharge of the total cohort and matched cohort. With the exception of digoxin, diuretics, and proton pump inhibitors, the nSCL group received significantly fewer class I drugs16 (antiplatelet agents, statins, and angiotensin-converting enzyme inhibitors/angiontensin receptor blockers). These patients also received fewer beta-blockers. However, they received more calcium channel antagonists.
Inhospital and Discharge Treatment in the Cohort Matched by the Presence or Absence of Significant Coronary Lesions
| Total cohort | Matched cohort | |||||
|---|---|---|---|---|---|---|
| nSCL (n = 389) | SCL (n = 1494) | P | nSCL (n = 367) | SCL (n = 367) | P | |
| Percutaneous coronary intervention | — | 80% (1195) | — | — | 83.1% (305) | — |
| Coronary artery bypass graft | — | 7.4% (140) | — | — | 4% (29) | — |
| Acetylsalicylic acid | 75.3% (293) | 92% (1374) | < .001 | 75.7% (278) | 92.6% (340) | < .001 |
| Clopidogrel | 25.4% (99) | 83.9% (1254) | < .001 | 25.6% (94) | 85.8% (315) | < .001 |
| Acetylsalicylic acid or clopidogrel | 94.4% (367) | 78.4% (1171) | < .001 | 79% (290) | 94.3% (346) | < .001 |
| Vitamin K antagonists | 16.2% (63) | 6.8% (102) | < .001 | 16.3% (60) | 10.4% (38) | .02 |
| Beta-blockers | 55.3% (215) | 66.7% (997) | < .001 | 54.8% (201) | 68.4% (251) | < .001 |
| Calcium antagonists | 29.8% (116) | 21.8% (326) | .001 | 30.2% (111) | 19.1% (70) | .001 |
| ACE inhibitor/ARB | 51.2% (199) | 62% (926) | < .001 | 51.8% (190) | 58.9% (216) | .06 |
| Antialdosterone | 3.3% (13) | 3.9% (58) | .7 | 3.3% (12) | 4.6% (17) | .5 |
| Statin | 74.6% (290) | 85.5% (1270) | <.001 | 74.7% (274) | 85% (312) | .001 |
| Digoxin | 1.8% (7) | 2.5% (37) | .5 | 1.9% (7) | 2.5% (9) | .8 |
| Proton pump inhibitor | 62.2% (242) | 63.2% (944) | .8 | 62.7% (230) | 64.9% (238) | .6 |
| Loop diuretics | 19% (74) | 17.9% (267) | .7 | 19.1% (70) | 16.9% (62) | .5 |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blockers; nSCL, no significant lesions; SCL, significant coronary lesions.
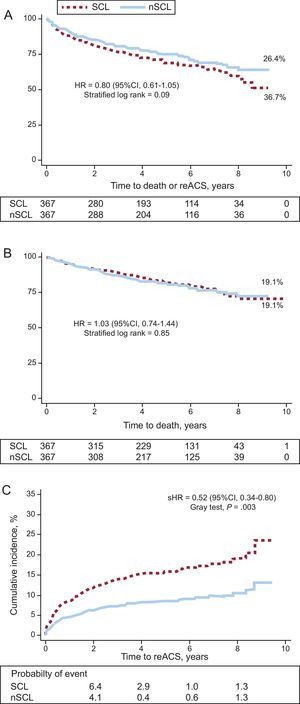
In the matched cohort, the primary event rate was slightly lower in the nSCL group (26.4%) than in the other group (32.7%; P = .09; Figure 3A). Mortality was the same in both groups (19.1%; Figure 3B).
A, survival curves and event-free survival curves for readmission for acute coronary syndrome by subgroup according to the presence or absence of significant coronary lesions. B, survival curves by subgroup according to the presence or absence of significant coronary lesions. C, accumulated incidence of readmission for acute coronary syndrome by subgroup according to the presence or absence of significant coronary lesions. Adjusted for mortality during follow-up as a competing event. 95%CI, 95% confidence interval; HR, hazard ratio; nSCL, no significant coronary lesions; reACS, readmission for acute coronary syndrome; SCL, significant coronary lesions; sHR, subhazard ratio.
Data on the cause of death were available for 88 of 140 (62.9%) patients: the cause was cardiovascular in 14.3% (n = 20) of the nSCL group and 19.3% (n = 27) in the other group (P = .38).
At follow-up, there was a lower incidence of reACS in the nSCL group than in the other group (2.0/100 vs 3.9/100 patient-years; P = .003). Survival curves show early divergence during follow-up (Fig. 3C).
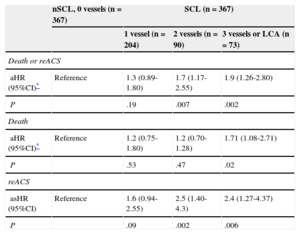
Table 4 shows the adjusted prognostic effect of nSCL compared with 1-, 2-, and 3-vessel disease or LCA. After adjustment using the GRACE score, no difference was found between nSCL and single-vessel disease in the composite of death and reACS (HR = 1.3; 95%CI, 0.89-1.80; P = .19). However, 2- or 3-vessel or LCA disease had a significantly greater negative impact on the composite of death or reACS (HR = 1.7; 95%CI, 1.17-2.55; P = .007) than nSCL (HR = 1.9; 95%CI, 1.26-2.80; P = .002).
Adjusted Prognostic Effect of the Absence of Obstructive Coronary Lesions and Coronary Obstructive Lesions According to Severity in the Matched Cohort
| nSCL, 0 vessels (n = 367) | SCL (n = 367) | |||
|---|---|---|---|---|
| 1 vessel (n = 204) | 2 vessels (n = 90) | 3 vessels or LCA (n = 73) | ||
| Death or reACS | ||||
| aHR (95%CI)* | Reference | 1.3 (0.89-1.80) | 1.7 (1.17-2.55) | 1.9 (1.26-2.80) |
| P | .19 | .007 | .002 | |
| Death | ||||
| aHR (95%CI)* | Reference | 1.2 (0.75-1.80) | 1.2 (0.70-1.28) | 1.71 (1.08-2.71) |
| P | .53 | .47 | .02 | |
| reACS | ||||
| asHR (95%CI) | Reference | 1.6 (0.94-2.55) | 2.5 (1.40-4.3) | 2.4 (1.27-4.37) |
| P | .09 | .002 | .006 | |
95%CI, 95% confidence interval; aHR, adjusted hazard ratio; asHR: adjusted subhazard ratio; LCA, left main coronary artery; nSCL, no significant coronary lesions; reACS, readmission for acute coronary syndrome; SCL, significant coronary lesions.
The presence of nSLC exhibited a protective effect against reACS, especially when compared to 2-vessel disease (sHR = 2.5; 95%CI, 1.40-4.30; P = .002) and 3-vessel disease or LCA disease (sHR = 2.4, 95%CI, 1.27-4.37; P = .006). In contrast, mortality was similar in patients with nSCL and patients with significant 1- and 2-vessel disease, but significantly less than in patients with 3-vessel disease or LCA disease.
DISCUSSIONThe main finding was that there was no significant difference in the elevated risk of death between the group with nSCL and NSTEMI and the other group. About 1 in 5 patients with nSCL and NSTEMI (mean age at admission 68 years) were deceased at 4.8 (2.6) years after discharge.
There was no significant difference in the adjusted risk of death in patients with nSCL and NSTEMI and patients with significant 2-vessel disease, but risk was higher in patients with a greater extent and severity of 3-vessel disease or LCA disease. In addition, the adjusted effect of NSTEMI and nSCL and risk of reACS was not significantly different from that found in patients with 1-vessel disease.
This study is the first to apply an analytical approach using propensity score matching to the long-term prognosis after discharge of patients with nSCL and NSTEMI. This study is also the first to determine the prognosis of patients with or without significant coronary lesions who have survived the acute phase of NSTEMI. This approach is of clinical relevance because patients with nSCL and NSTEMI can be incorrectly considered as patients at a low risk of future adverse events during follow-up.
There is debate concerning the overall prognosis, and particularly the long-term prognosis, of these patients. Several studies have demonstrated that patients with nSCL have better short-term prognosis than patients with significant coronary lesions,3,11 but there is little information on their long-term prognosis. In a sample of 274 patients with chest pain and nSCL, Hirota et al17 demonstrated a low rate of major cardiovascular events during a follow-up ranging from 2 to 13 years. In Spain, Cortell et al10 found that the absence of significant coronary stenosis was associated with a decreased risk of death or myocardial infarction (HR = 0.3; 95%CI, 0.2-0.9) after 3 years of follow-up. Pooled data from 8 clinical trials conducted between 1994 and 2008 that included more than 30 000 patients showed that the absence of significant coronary stenosis in patients with non—ST-segment elevation ACS protected against reinfarction or death at 6 months.11
Although the findings of this study are not directly comparable with those of previous ones, mainly due to differences in design, the finding of the elevated death rate in patients with NSTEMI and with nSCL and the lower incidence of reACS agrees with the findings of a recent substudy of the ACUITY clinical trial.18 However, unlike the ACUITY substudy, this study provides information on the survival index. Furthermore, the larger sample allowed comparisons between the effect of the absence of significant coronary lesions in different subgroups of patients with a varying extent and severity of coronary artery disease. In fact, the results suggest that mortality rates in patients with NSTEMI and nSCL are greater than in patients with 1-vessel disease, similar to those with 2-vessel disease, but lower than those with 3-vessel disease or LCA disease. These results are in line with those reported by Larsen et al.9 Despite their finding that mortality was significantly lower after 3.3 years of follow-up in patients with acute myocardial infarction and nSCL, this difference disappeared after stratifying the sample for patients with completely normal coronary arteries (4% mortality), coronary with < 50% lesions (2.9% mortality), and significant lesions in 1 or 2 vessels (3.3% mortality). Larsen et al9 also found that mortality in patients with 3-vessel disease or LCA disease, as in this series, was the only scenario in which long-term mortality exceeded that of patients with nSCL.
The results of this study, the ACUITY clinical trial substudy,18 and the study by Larsen et al9 suggest that coronary angiography alone is not an effective tool for defining risk, particularly that of mortality, among patients with NSTEMI and nSCL.
It is difficult to explain the poor prognosis of patients with NSTEMI and nSCL. Coronary angiography may underestimate the presence of significant atherosclerotic burden because this technique cannot detect the eccentric expansion of atherosclerotic plaque.4,5 Histological studies may show small plaque ruptures or even erosion in the absence of significant coronary stenosis.6,7
Moreover, a coronary thrombosis already resolved by the time of angiography, especially in the context of antithrombotic multitherapy, may appear as nonsignificant vestigial stenosis despite its instability. Although often benign, coronary spasm can also play a causative role in NSTEMI and nSCL and may be associated with mortality.19
The fact that these patients did not receive adequate secondary prevention therapy may have affected their prognosis. In this series, patients with nSCL received fewer class I drugs16 (antiplatelet agents, statins, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers). Unfortunately, etiological factors related to NSTEMI and the absence of significant coronary lesions can only be found in a minority of cases.20 This study suggested slow flow, suspected spasm, milking, and tako-tsubo syndrome as possible mechanisms underlying NSTEMI and nSCL. The effect of tako-tsubo syndrome on patient prognosis is known to be benign21 and does not seem to explain the high death rate in the nSCL group observed in this study.
The results of this study may have clinical implications. The high mortality of patients with NSTEMI and nSCL indicates that this clinical entity should be treated with caution and that a detailed epidemiologic study should be performed. Imaging studies to characterize and quantify atherosclerotic plaques, such as intravascular echocardiography22,23 or coronary computed tomography angiography,24 functional angiography studies,25 and possibly magnetic resonance imaging should be part of the battery of diagnostic tests to differentiate small plaque rupture or erosion from other ACS entities, such as aortic dissection or pulmonary thromboembolism.
The stratification for risk of death or reACS in this subgroup of patients is of particular interest, given the difficulty in real life of reaching an accurate diagnosis, which would identify patients who would benefit from therapeutic measures and closer monitoring.
Furthermore, although the patients with nSCL received fewer drugs of proven prognostic efficacy at discharge, it remains unknown whether the prognostic benefit of these drugs is similar to what is expected for all patients with ACS. Future studies should resolve this issue.
LimitationsThis study was retrospective and has the limitations inherent to this type of study. Catheterization was indicated at the discretion of the attending cardiologist and patients with a history of coronary revascularization were excluded, which may have influenced the prevalence of NSTEMI and nSCL. However, it is important to note that the aim of the study was not to determine the prevalence, care burden, and predictors of nSCL. Propensity score analysis is more robust than classic regression analysis, but it has certain weaknesses; for example, unmeasured confounding factors cannot be corrected. Although this study excluded patients with type 2 acute myocardial infarction and unconfirmed ACS at discharge, secondary causes associated with poor prognosis cannot be completely ruled out.8 Although some of the patients included in this study were diagnosed with NSTEMI, they may have had ischemic symptoms with elevated troponin for reasons other than an ACS. Finally, coronary lesions were quantified by visual analysis rather than by quantitative analysis, although this approach reflects clinical practice in many centers worldwide. Unfortunately, the diagnostic approach used in this study did not include data derived from functional testing or intracoronary imaging, and neither was magnetic resonance imaging performed to characterize myocardial tissue.
Finally, due to the lack of data on treatment during follow-up, it cannot be ruled out that the observed differences between the 2 groups could be at least partly due to differences in the treatment they received.
CONCLUSIONSIn this contemporary registry of patients with ACS, long-term mortality after discharge in this subgroup of patients is alarming in terms of a disproportional level of severity or risk into which they can be classified. Mortality or reACS in patients with NSTEMI and nSCL can be similar to that of patients with significant 1-vessel disease, but less than that in patients with disease in 2 or more vessels.
CONFLICTS OF INTERESTNone declared.
We would like to thank all the staff of the cardiology department at the Complejo Hospitalario Universitario de Santiago de Compostela for their excellent clinical work and involvement. Special thanks to the coronary care unit nurses Isabel Arufe and Belen Outes for their contribution to this work.