To the Editor,
The MELAS syndrome (mitochondrial encephalopathy, lactic acidosis and stroke-like episodes) is a mitochondrial disease with heart manifestations in which conduction alterations and hypertrophic (more frequent) or dilated cardiomyopathy are the most outstanding.
A pregnant 23-year-old female undergoes, neurology and cardiology consultations for possible mitochondrial disease (short of height, deaf and with asymptomatic Wolff-Parkinson-White syndrome). On ECG concentric ventricular hypertrophy and normal ventricular function were found, with no other cardiovascular history. Her mother had died at 42 years of age diagnosed with MELAS syndrome, with hypertrophic cardiomyopathy, multiple episodes of acute lung oedema, deafness and repeat ictus. Her grandmother had died in the fourth decade of life due to non-specified heart causes.
From the 20th week of gestation on she began to have episodes in which she had difficulty breathing accompanied occasionally by typical chest pain. During week 23 she had a new episode of dyspnoea, with coughing and right hemithorax pain of pleural characteristics, which caused her to come in to maternity emergency and after which she remained hospitalized.
During physical exam paleness, jugular ingurgitation, tachycardial tones without murmurs and bilateral crepitant rale on auscultation were found. The ECG showed a sinus rhythm with 130 beats/min, a PR interval of 0.04 seconds and a delta wave. Analysis showed: creatinine, 1.4mg/ dl; troponin I, 4.42 ng/mL; WBC, 14 370/µL (neutrophils, 13 520/µL, without band neutrophils). Basal blood gasses showed pCO2, 24 mmHg; pO2, 45 mmHg, and pH, 7.44.
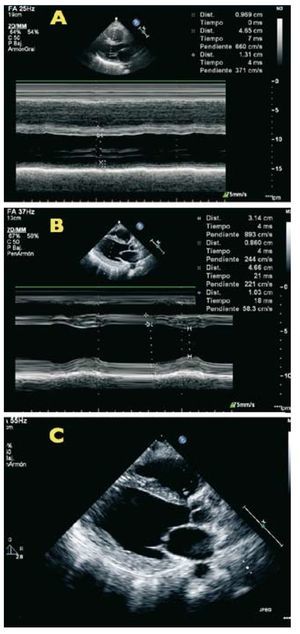
Twenty-four hours after admission the patient worsened and a chest x-ray showed a pattern of acute lung edema requiring orotracheal intubation and invasive mechanical ventilation. A heart US was performed (Figure 1) and concentric hypertrophy of the left ventricle was seen with a severely depressed systolic function (EF, 30%). Treatment with furosemide, nitroglycerine and dopamine at diuretic doses was initiated.
Figure 1. Echocardiogram images during an acute event, it is possible to see the significant improvement in systolic function. A: during admittance, in M mode; B: after hospital discharge, in M mode; C: after discharge in 2D mode.
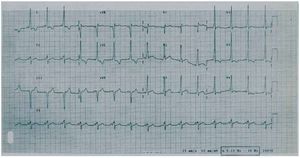
Four days after admission to the intensive care unit (ICU), fetal death was determined and expulsion took place, subsequently the placenta was extracted and curettage performed. On the tenth day the patient was extubated. The follow-up cardiac echocardiogram showed improvement of ventricular function (EF 45%). The ECG showed a sinus rhythm with 90 beats/min, a PR interval of 0.04 seconds and a delta wave (Figure 2).
Figure 2. Electrocardiogram with the typical delta wave pattern seen in Wolff-Parkinson-White syndrome.
After discharge, the haematology service continued an ambulatory study of the patient, and found presence of lupic anticoagulant and resistance to activated protein C. At the same time, in the neurology external consulting offices the genetic study was completed and the diagnosis of MELAS syndrome confirmed with the finding of mutation A3243G in the mitochondrial DNA (blood sample). After 5 years of follow-up in cardiology consulting offices, ventricular function has remained normal (EF >55%) with no new signs of heart failure.The combination of mitochondrial myopathy, encefalopathy, lactic acidosis and ictus type episodes constitute a mitochondrial disease known as MELAS.1 It is exclusively inherited from the mother and 80% of cases are due to a mutation of the A3243G gene of the tRNA of mitochondrial DNA. Other clinical signs are deafness, diabetes, dystonia, short height, and cardiovascular symptoms including dilated and hypertrophic cardiomyopathy, alterations of conduction and Wolff-Parkinson-White2 syndrome.
It is well-known that there are metabolic and haemodynamic changes during pregnancy that lead to an increase in mitochondrial function to generate more energy.3 In patients with mitochondrial dysfunction, this is exacerbated, and there is clinical worsening; in the case of this patient this caused heart failure with ventricular dysfunction that resolved progressively after foetal death and expulsion.
The relation between lupic anticoagulant and abortion in this type of patient is not clear.4 However, some studies have shown an increase in oxidative stress in the presence of these molecules,5 which increases the unfavourable conditions when there is coexistence with a mitochondrial disease such as MELAS.
There are very few cases described of worsening of mitochondrial diseases during pregnancy,3 and pregnancy must be considered a high risk factor in these patients.