To the Editor,
Proximal pulmonary artery aneurysm (PAA) is defined as a dilation of the pulmonary artery trunk or its main branches. It is an infrequent disease of difficult diagnosis1 that is usually silent and is an autopsy finding. Occasionally, it causes severe complications such as airway compression,2 pulmonary artery (PA) dissection3 and intravascular thrombosis. Pulmonary hypertension (PH) is considered an important factor involved in its pathogenesis, and has mainly been described in patients with more severe PH such as is seen in the Eisenmenger syndrome. The incidence rate of these aneurysms in the population of patients with PH is low.
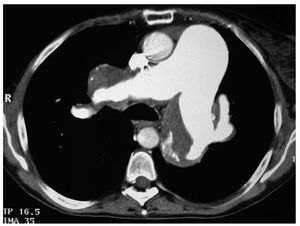
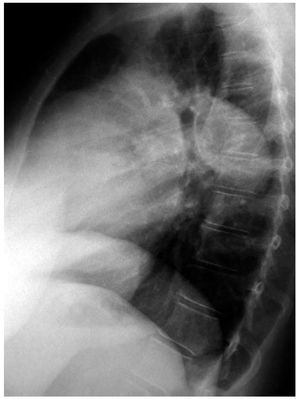
Of the 320 patients included in our pulmonary hypertension unit (mean PA pressure 56 mm Hg), we found 4 cases of proximal PAA diagnosed with chest CT after the appearance of complications. These 4 patients had severe PH (mean PA pressure 55 mmHg on catheterisation) of different aetiology (2 cases of idiopathic arterial PH and 2 cases of Eisenmenger syndrome). Before PAA diagnosis, the patients were in functional classes II-III of the WHO and in treatment with acenocoumarol and specific drugs for PH (2 patients with sildenafil and 2 patients with a combined therapy with sildenafil and subcutaneous teprostinil). Two of them came in to the emergency service with a persistent dry cough and one with compressive athelectasia. A chest CT showed an aneurysmatic dilation of the pulmonary trunk and its branches (PAA diameter 47-67mm) with non-occlusive thrombosis in its interior and bronchial compression (Figure 1). Perfusion gamma scintigraphy ruled out perfusion defects indicating lung thromboembolism. Thrombi are relatively frequent in PAA and make it necessary to carry out a differential diagnosis with chronic thromboembolic PH.4 The hypercoagulability study was normal and other causes associated with PAA were ruled out.5 In all patients specific treatment for PH was intensified, compressive symptoms disappeared and anticoagulation was maintained due to the risk of thrombosis in the PAA region. The patients have been reviewed every 3 months without recurrence of clinical symptoms seen (follow-up: 2-3 years). In the follow-up CT carried out, the persistence of aneurysms without complications was confirmed. The fourth patient was admitted with chest pain; a chest X-ray showed dilation of the main PA (Figure 2); chest CT showed an aneurysm of the PA trunk and its main branches of 46.6mm in diameter and a flap of the intima at the origin of the left PA. The lobular arteries arose out of the true artery lumen and were compressed by the false lumen of the aneurysm. No recent factors that could have precipitated dissection were found, except for the PH itself. The possibility of surgical treatment was ruled out due to the high risks of the intervention, as also was the possibility of percutaneous repair due to the risk of occlusion of the lobular arteries. Anticoagulant treatment was suspended and specific PH treatment intensified. In the follow-up CT, it was seen that the dissection had not progressed. The patient has worsened clinically and is currently on the waiting list for cardiopulmonary transplant.
Figure 1. Chest computed tomography: aneurysmatic dilation of the trunk and main branches of the pulmonary artery.
Figure 2. Chest x-ray. Lateral projection: aneurysmatic dilation of the main pulmonary artery.
In our experience, intensification of specific PH treatment improves airway compression, which was the most frequently seen complication in our patients. Maintenance of anticoagulation, although controversial, is usually necessary due to the risk of PAA thrombosis, although it may be necessary to suspend it in cases of haemoptysis, progressive growth of the PAA or if there is concomitant dissection.