Abnormal electrocardiographic findings are highly common. The aim of this study was to analyze the prevalence of abnormal electrocardiographic patterns in the general Spanish population aged 40 years or older.
MethodsThis subanalysis of the OFRECE study selected a representative sample of the Spanish population aged 40 years or older. Clinical data and electrocardiograms were available in all participants. The electrocardiograms were read centrally. Each electrocardiogram was independently assessed by 2 trained cardiologists and, if there was disagreement, a third was consulted to reach a consensus-based diagnosis. Prior to reading the electrocardiograms, diagnostic criteria were strictly defined for each of the abnormalities analyzed. We analyzed the prevalence and clinical factors associated with cavity enlargement, conduction disorders, repolarization abnormalities, pathological Q waves, atrial and ventricular premature beats, and pre-excitation.
ResultsA total of 8343 individuals were evaluated, (mean age, 59.2 years; 52.4% women). Only 4074 (51.2%) participants had a completely normal electrocardiogram. The most frequent abnormalities were nonspecific repolarization abnormalities (16%) associated with coronary heart disease and atrial fibrillation; right bundle-branch block (8.1%) associated with chronic pulmonary obstructive disease; left anterior hemiblock (6.5%) related to hypertension and congestive heart failure; and long PR interval (3.7%), which was associated with coronary heart disease.
ConclusionsElectrocardiographic abnormalities are very common in the general population aged 40 years or older. Only about half of the population had a completely normal electrocardiogram.
Keywords
Electrocardiography (ECG) is a valuable diagnostic test, used to detect heart disease in symptomatic patients and as a screening method in apparently healthy populations.1 In several studies, the prevalence of abnormal ECG findings have been evaluated in various population samples. Some of these studies were conducted in the work setting, where most of the participants were men,2 others focused on specific anomalies,3,4 and many were carried out between the 1960s and 1990s.5–7 There are no recent studies analyzing the prevalence of ECG changes in an unselected general population sample. The aim of this study was to determine the prevalence of abnormal ECG findings in the general population of Spain aged 40 years and older, and the clinical and epidemiologic factors potentially related to these findings.
METHODSThis is a substudy of the OFRECE project, which was approved by the Ethics Committee for Clinical Research of Hospital Universitario de Basurto and other hospital or regional committees, in accordance with local regulations. The main aim of the study was to determine the prevalence of atrial fibrillation (AF) and stable angina in the Spanish population 40 years of age and older. OFRECE was a cross-sectional study promoted by the Research Agency of the Spanish Society of Cardiology, conducted in persons at least 40 years of age assigned to a primary care physician. The methods used and the results obtained in OFRECE are described elsewhere.8,9 Sampling was carried out in 2 stages: First, a number of primary care physicians from each province of Spain were randomly selected to participate, and second, 20 individuals were randomly selected from the population assigned to each participating physician. In total, 11 831 individuals were chosen, and 11 055 were contacted and invited to participate by their primary care physician. Among those contacted, 76% agreed to participate (n=8400).
The most common reason for failure to participate was inability to contact the person (65.3%), followed by refusal to participate (33.5%). The flow chart depicting enrollment in the OFRECE study can be consulted in the previous articles.8,9 All those included gave written informed consent for enrollment. OFRECE was initiated throughout Spain in March 2010 and was completed in October 2012. The primary care physicians, cardiologists, and other collaborators in the study are listed in Appendix 1 of the supplementary data. All participants were examined by their primary care physician, who recorded information on demographics and various clinical variables for subsequent analysis, including obesity, overweight, hypercholesterolemia, diabetes mellitus, smoking, high blood pressure, history of stroke, peripheral artery disease, chronic pulmonary disease, thyroid disease, pacemaker or automatic defibrillator implantation, ischemic heart disease, heart failure, and AF. ECG was carried out, and the person's weight, height, and blood pressure were measured. Blood pressure was determined twice, in keeping with the recommendations of the World Health Organization, included in the current guidelines of the European Society of Cardiology.10 When suspicion of a previously unknown heart condition was raised during the study visit, the participant was referred to the coordinating cardiologist, and the need to perform additional tests was explained. The definitions of the various risk factors and medical background analyzed followed the predefined standards of the American College of Cardiology/American Heart Association11 (Appendix 2 of the supplementary data).
Fifty-seven patients were excluded from the analysis because key information was missing (n=4) or because the electrocardiogram was not assessable (n=53), which left a final sample of 8343 individuals for the analysis.
All ECG tracings were read centrally by a group of 9 cardiologists. Electrocardiograms were randomly assigned to each cardiologist for the first reading, and were independently reviewed by a second cardiologist. When there was a discrepancy between the 2 evaluations, a third cardiologist was consulted, and the final diagnosis was established by consensus.
The diagnostic criteria for each ECG abnormality analyzed were established according to the Minnesota Code12 in most cases, and are summarized in Appendix 3 of the supplementary data. In the present study, there are no data on ECG patterns related to sudden cardiac death, as these findings were the subject of another article.13
Statistical AnalysisDue to the nature of the sampling process, in which individuals within the population had different probabilities of being selected, each participant in the final sample was assigned a weight to reflect the number of people in the Spanish population of the same sex, and from the same age group and geographical area that the participant represented.14 Hence, the sum of all weights in the sample was equal to the size of the Spanish population aged 40 years and older. Weighting was complex and was done in 2 stages, according to the methods described in previous OFRECE studies.8,9 In the first stage, the weights to apply were defined, and in the second, the weights were calibrated according to the proposed procedure of Deville and Särndal15 using the calibrate instruction provided in the Stata v10.1 statistical software package. The 2011 municipal population census was used to adjust or calibrate the sample according to sex, age group, and geographic area.
All analyses took into account the sampling design of the study. The overall prevalence and specific prevalences by age and sex for all the variables analyzed were calculated with 95% confidence intervals (95%CI). When necessary, means or percentages were calculated, as appropriate, according to whether the variables were quantitative or qualitative.
To identify clinical factors associated with the ECG changes of interest, sex- and age-adjusted odds ratios (ORs) were estimated using logistic regression modeling. Subsequently, to identify factors independently associated with the conditions of interest, a multivariate model was constructed, including variables with p<0.1 in the previous bivariate analysis.
All the prevalence data presented in the results are weighted by sex and age (WP) with 95%CIs. Agreement between the first and second ECG reading was assessed using analysis of interobserver variance, applying Cohen's kappa coefficient to each of the variables analyzed.
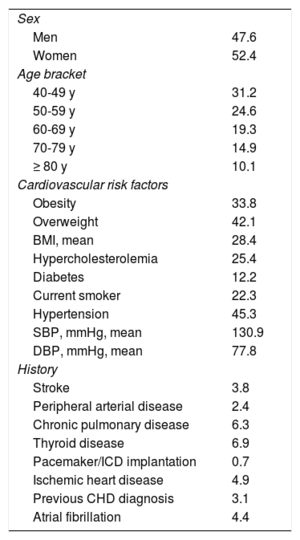
RESULTSIn total, 8343 individuals were analyzed (52.4% women) with a mean age of 59.2±13.5 years. The characteristics of the study participants, their cardiovascular risk factors, and their clinical background are shown in Table 1. Agreement between the first and second observer in the ECG reading was very high (> 95%). The kappa coefficient for each ECG finding is shown in Table 2. Additional information on the interobserver agreement can be found in Appendix 4 of the supplementary data.
Characteristics of the OFRECE Study Population (n=8343)
| Sex | |
| Men | 47.6 |
| Women | 52.4 |
| Age bracket | |
| 40-49 y | 31.2 |
| 50-59 y | 24.6 |
| 60-69 y | 19.3 |
| 70-79 y | 14.9 |
| ≥ 80 y | 10.1 |
| Cardiovascular risk factors | |
| Obesity | 33.8 |
| Overweight | 42.1 |
| BMI, mean | 28.4 |
| Hypercholesterolemia | 25.4 |
| Diabetes | 12.2 |
| Current smoker | 22.3 |
| Hypertension | 45.3 |
| SBP, mmHg, mean | 130.9 |
| DBP, mmHg, mean | 77.8 |
| History | |
| Stroke | 3.8 |
| Peripheral arterial disease | 2.4 |
| Chronic pulmonary disease | 6.3 |
| Thyroid disease | 6.9 |
| Pacemaker/ICD implantation | 0.7 |
| Ischemic heart disease | 4.9 |
| Previous CHD diagnosis | 3.1 |
| Atrial fibrillation | 4.4 |
BMI, body mass index; CHD, congestive heart disease; DBP, diastolic blood pressure; ICD, implantable cardioverter-defibrillator; SBP, systolic blood pressure.
Values are expressed as percentages unless otherwise indicated.
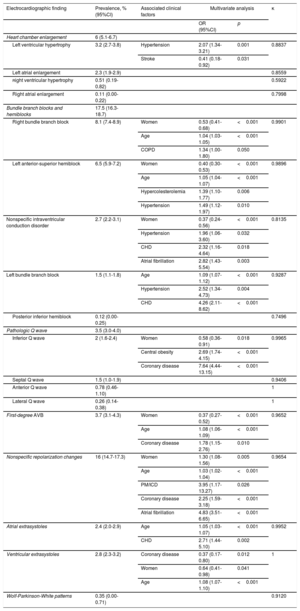
Results: Prevalence of Abnormal Electrocardiographic Findings and Related Clinical Factors
| Electrocardiographic finding | Prevalence, % (95%CI) | Associated clinical factors | Multivariate analysis | κ | |
|---|---|---|---|---|---|
| OR (95%CI) | p | ||||
| Heart chamber enlargement | 6 (5.1-6.7) | ||||
| Left ventricular hypertrophy | 3.2 (2.7-3.8) | Hypertension | 2.07 (1.34-3.21) | 0.001 | 0.8837 |
| Stroke | 0.41 (0.18-0.92) | 0.031 | |||
| Left atrial enlargement | 2.3 (1.9-2.9) | 0.8559 | |||
| Right ventricular hypertrophy | 0.51 (0.19-0.82) | 0.5922 | |||
| Right atrial enlargement | 0.11 (0.00-0.22) | 0.7998 | |||
| Bundle branch blocks and hemiblocks | 17.5 (16.3-18.7) | ||||
| Right bundle branch block | 8.1 (7.4-8.9) | Women | 0.53 (0.41-0.68) | <0.001 | 0.9901 |
| Age | 1.04 (1.03-1.05) | <0.001 | |||
| COPD | 1.34 (1.00-1.80) | 0.050 | |||
| Left anterior-superior hemiblock | 6.5 (5.9-7.2) | Women | 0.40 (0.30-0.53) | <0.001 | 0.9896 |
| Age | 1.05 (1.04-1.07) | <0.001 | |||
| Hypercolesterolemia | 1.39 (1.10-1.77) | 0.006 | |||
| Hypertension | 1.49 (1.12-1.97) | 0.010 | |||
| Nonspecific intraventricular conduction disorder | 2.7 (2.2-3.1) | Women | 0.37 (0.24-0.56) | <0.001 | 0.8135 |
| Hypertension | 1.96 (1.06-3.60) | 0.032 | |||
| CHD | 2.32 (1.16-4.64) | 0.018 | |||
| Atrial fibrillation | 2.82 (1.43-5.54) | 0.003 | |||
| Left bundle branch block | 1.5 (1.1-1.8) | Age | 1.09 (1.07-1.12) | <0.001 | 0.9287 |
| Hypertension | 2.52 (1.34-4.73) | 0.004 | |||
| CHD | 4.26 (2.11-8.62) | <0.001 | |||
| Posterior inferior hemiblock | 0.12 (0.00-0.25) | 0.7496 | |||
| Pathologic Q wave | 3.5 (3.0-4.0) | ||||
| Inferior Q wave | 2 (1.6-2.4) | Women | 0.58 (0.36-0.91) | 0.018 | 0.9965 |
| Central obesity | 2.69 (1.74-4.15) | <0.001 | |||
| Coronary disease | 7.64 (4.44-13.15) | <0.001 | |||
| Septal Q wave | 1.5 (1.0-1.9) | 0.9406 | |||
| Anterior Q wave | 0.78 (0.46-1.10) | 1 | |||
| Lateral Q wave | 0.26 (0.14-0.38) | 1 | |||
| First-degree AVB | 3.7 (3.1-4.3) | Women | 0.37 (0.27-0.52) | <0.001 | 0.9652 |
| Age | 1.08 (1.06-1.09) | <0.001 | |||
| Coronary disease | 1.78 (1.15-2.76) | 0.010 | |||
| Nonspecific repolarization changes | 16 (14.7-17.3) | Women | 1.30 (1.08-1.56) | 0.005 | 0.9654 |
| Age | 1.03 (1.02-1.04) | <0.001 | |||
| PM/ICD | 3.95 (1.17-13.27) | 0.026 | |||
| Coronary disease | 2.25 (1.59-3.18) | <0.001 | |||
| Atrial fibrillation | 4.83 (3.51-6.65) | <0.001 | |||
| Atrial extrasystoles | 2.4 (2.0-2.9) | Age | 1.05 (1.03-1.07) | <0.001 | 0.9952 |
| CHD | 2.71 (1.44-5.10) | 0.002 | |||
| Ventricular extrasystoles | 2.8 (2.3-3.2) | Coronary disease | 0.37 (0.17-0.80) | 0.012 | 1 |
| Women | 0.64 (0.41-0.98) | 0.041 | |||
| Age | 1.08 (1.07-1.10) | <0.001 | |||
| Wolf-Parkinson-White patterns | 0.35 (0.00-0.71) | 0.9120 | |||
95%CI, 95% confidence interval; AVB, atrioventricular block; CHD, congestive heart disease; COPD, chronic obstructive pulmonary disease; κ, Cohen's kappa coefficient; PM/ICD, pacemaker or implantable cardioverter-defibrillator; OR, odds ratio
ECG findings were considered to be strictly normal in only 4074 participants (WP, 51.2%; 95%CI, 49.5%-52.9%). Most individuals (n=8310) showed a natural heart rhythm, 25 had pacemaker-mediated rhythm, and 8 an alternating rhythm. Sinus rhythm was the most common in those with a natural rhythm (8011 participants; WP, 96.6%; 95%CI, 96.1%-97.2%). The second most common natural rhythm was AF (252 participants; WP, 2.80%; 95%CI, 2.30%-3.30%). Other findings such as flutter or wandering atrial rhythm were very infrequent. The prevalence of the various ECG findings and the clinical and epidemiologic factors found to be associated with them on multivariate analysis are shown in Table 2. The analysis was carried out with variables showing a high prevalence or having the greatest clinical relevance. Data from the univariate analysis and the distribution by sex and age for each abnormality are included in Appendix 5 of the supplementary data.
The most highly prevalent abnormalities were bundle branch blocks and hemiblocks, present in 17.5% of the study population. In general and with the exception of left bundle branch block, these disorders were more prevalent in men. The most common was complete or incomplete right bundle branch block (WP, 8.1%; 59.9% of cases in men), which was not associated with heart disease, but instead, with chronic obstructive pulmonary disease. The second most common conduction disorder was left anterior-superior hemiblock (WP, 6.5%; 63.4% in men), which was associated with hypertension and hypercholesterolemia. Nonspecific intraventricular conduction disorder (WP, 2.7%; 68% in men), usually given little importance, was related to a higher cardiovascular risk burden. The independent predictors of this disorder were hypertension, AF, and heart failure. Patients with pacemaker rhythms were excluded from the prevalence analysis of left bundle branch block. This disorder showed a low prevalence (1.5%) and a strong association with hypertension and heart failure. There were no significant differences regarding the distribution by sex, but age was an independent predictive factor, as was seen in the other conduction disorders.
Nonspecific repolarization changes were the most prevalent findings detected alone (16% of the study population). Only participants without left bundle branch block were included in the analysis (n=8184). These changes were associated with coronary disease, AF, and having an implanted pacing device, and were more common in women (58.1% of individuals with this finding).
With regard to enlargement of the heart chambers (WP, 6%), the most common was left ventricular hypertrophy, whose predictive factor was hypertension.
Pathologic Q wave in any location was found in 3.5% of the population. The most prevalent were inferior Q waves, which were associated with coronary disease, central obesity, and male sex (men accounted for 61.1% of participants with this finding).
Analysis of the prevalence of extrasystoles only included the population in sinus rhythm. Ventricular extrasystoles were found in 2.8%. Atrial extrasystoles showed a prevalence of 2.4% and were most commonly found in participants with heart failure.
Wolf-Parkinson-White patterns were very uncommon in the study population, occurring in only 0.35%.
DISCUSSIONThis study focuses on the prevalence of ECG findings in an unselected general population. We analyzed a large sample with considerable age variation and a more balanced distribution by sex than that of the most recent studies of this type. Our population has an advantage over the samples in these studies, where the information was often obtained from data collected in medical examinations performed in the work setting, the armed forces, etc. These population samples tend to include younger people and a high percentage of men. Thus, the results obtained may be influenced by a certain degree of selection bias. Furthermore, unlike other studies, we carried out univariate and multivariate analyses to establish which clinical and epidemiologic variables were associated with each of the ECG changes detected.
We recorded a high percentage (∼50%) of abnormal ECG findings, which has important clinical repercussions, not only because of the doubts they may generate, but because many are markers of cardiovascular disease. The percentage found is greater than the value reported in the most recent prevalence study by Rodríguez-Capitán et al.2 likely because our participants were, on average, 12 years older, and a higher presence of comorbidities would be expected. The most prevalent abnormalities found are analyzed individually below. As was mentioned, we have not provided data on the prevalence or factors associated with ECG patterns related to sudden cardiac death, as these findings were the subject of a more detailed previous study.13
Bundle Branch Block and HemiblocksThis group of disorders was the most prevalent (WP, 17.5%; 95%CI, 16.3%-18.7%), and the results concur with those of Rodríguez-Capitán et al.2 As these authors also noted, conduction disorders generally showed a higher prevalence in men and tended to be more frequent with aging.
Right bundle branch block (complete or incomplete) was the most common conduction disorder (WP, 8.1%; 95%CI, 7.4%-8.9%). The prevalence of this condition was somewhat higher than the values reported in other series, perhaps because we included both complete and incomplete blocks in the analysis. On multivariate analysis there was a significant association of right bundle branch block with pulmonary disease, but not with heart disease.
Left anterior-superior hemiblock was the second most common conduction disorder found (WP, 6.5%; 95%CI, 5.9%-7.2%). There are no data on the prevalence of this abnormality in the older series.5–7 The KORA study3 reported a prevalence of 0.16% and Rodríguez-Capitán et al. 0.5%,2 likely because of the greater presence of younger individuals in both these studies. In our series, left anterior-superior hemiblock was associated with a higher cardiovascular risk burden on multivariate analysis, which suggests that this finding, in itself, should lead us to consider more exhaustive risk stratification in these patients.
Intraventricular conduction disorder is a nonspecific ECG abnormality that is often dismissed or included within right or left bundle branch blocks. We consider this an error, as the criteria regarding these 3 conduction disorders are different and well defined.12 In the classic series, there is no mention of the prevalence of this finding. Only KORA3 and the study by Rodríguez-Capitán et al.2 specifically analyze the prevalence of intraventricular conduction disorder, but no data are provided on related clinical factors. In our population, it was the third most common conduction disorder and its presence identified patients with a high cardiovascular disease burden. On multivariate analysis, it showed a strong association with hypertension, heart failure, and AF. Of note, the association between intraventricular conduction disorder and hypertension yielded an OR of 1.96, a value similar to that of left ventricular hypertrophy and hypertension (OR=2.07) and greater than that of left anterior-superior hemiblock and hypertension (OR=1.49). Hence, ECG findings of nonspecific intraventricular conduction disorder should be taken into account in the clinical evaluation of patients with suspected structural heart disease.
The prevalence of left bundle branch block in our series (WP, 1.6%; 95%CI, 1.1%-1.8%) was higher than the values reported by Ostrander et al. (0.35%)5 and Rodríguez-Capitán et al.,2 likely because of the lower mean age of the participants in these studies. Our prevalence is similar to the values reported by Rose et al.6 (between 0.98 and 3.18%, depending on age group) and De Bacquer et al.7 (between 0.1 and 2.0%, depending on sex and age). As expected, left bundle branch block identified patients with a larger cardiovascular disease burden (hypertension, heart failure), which is in keeping with the traditional perception that detection of this disorder, even in an asymptomatic patient, requires consultation with a cardiologist. Unlike the other conduction disorders, distribution by sex of left bundle branch block showed no significant differences.
Nonspecific Repolarization AbnormalitiesAs in other series, nonspecific repolarization changes were the most common ECG abnormalities (16% of participants). These findings generate diagnostic uncertainty and, because of their high prevalence, may imply numerous visits to the cardiologist and even emergency room admittance. Usually these findings are considered “nonspecific” (as the name indicates) and they may be given little importance. Nonetheless, a higher cardiovascular disease burden was found in this group of participants. Multivariate analysis associated this finding with AF and a greater coronary heart disease burden. Thus, nonspecific repolarization changes are not irrelevant findings; they may help to identify patients with higher cardiovascular risk.
Left Ventricular HypertrophyLeft ventricular hypertrophy was detected in 3.2% of the study participants. This percentage is similar to the values reported by Ostrander et al. (4%)5 and Rodríguez-Capitán et al. (3.6%),2 which is surprising as different diagnostic criteria were used. We consider that the findings of Rose et al.6 and De Bacquer et al.7 are not comparable to ours, as these authors refer to the prevalence of “tall R waves” and not specifically to left ventricular hypertrophy. Other series, such as the one in KORA3 showed a low prevalence of this abnormality (1.74%). Overall, a very low percentage of abnormal ECG findings was detected in KORA, perhaps because of the method used (automatic ECG analysis) and the characteristics of the sample. On multivariate analysis in the present study, hypertension was an independent predictor of left ventricular hypertrophy and surprisingly, a history of stroke was a protective factor. This is a striking finding that does not have a clear explanation. A higher prevalence of left ventricular hypertrophy would be expected in stroke patients as an expression of a higher cardiovascular risk burden (eg, greater hypertension). It could be that stroke patients undergo more intensive control of cardiovascular risk factors, such as hypertension, and this could lead to a smaller percentage of left ventricular hypertrophy.
Atrioventricular BlockThe prevalence of first-degree atrioventricular block was 3.7%, similar to the values described in classic series,6 in which a higher prevalence of this abnormality was found in association with aging: 1.86% in the group aged 40 to 49 years and 3.39% in those aged 60 to 69 years. Although prolonged PR interval has been traditionally considered a benign finding, our results are more in agreement with those of Cheng et al.,16 who reported that prolonged PR is associated with AF, pacemaker implantation, and increased mortality. In our population, long PR was more prevalent in men (65.6% of the total with this finding) and was associated with a higher cardiovascular risk burden, which may indicate a need to change our view that prolonged PR is a minor finding. The very low prevalence of other, higher-grade atrioventricular blocks was surprising: There were only 3 Wenckebach blocks and no Mobitz II or complete blocks. In this line, Ostrander et al.,5 Rose et al.,6 and Rodríguez-Capitán et al.2 also found a very low prevalence of high-grade atrioventricular blocks.
Pathologic Q Wave in Inferior LeadsPathologic Q wave in an inferior location was present in 2% of participants, a somewhat higher value than has been reported in other series.2,5,6 The prevalence of pathologic Q wave in any location (anterior, inferior, lateral, etc.) in these reports ranges from 0.9% to 3.2%.2,5–7 As in other studies, inferior pathologic Q wave was the most prevalent and was associated with coronary artery disease (OR=7.64) and central obesity (OR=2.69). When inferior pathologic Q wave is detected, we should (of course) think of an underlying coronary substrate, but there is another possibility: a phenomenon related to horizontal positioning of the cardiac apex in persons with central obesity, in particular if the affected patient is a man.
Atrial ExtrasystolesAtrial extrasystoles were found in 2.4% of participants, a value higher than the 0.3% reported by Rodríguez-Capitán et al.,2 perhaps because our population sample was older. This abnormality was associated with a higher percentage of heart failure, which contradicts the traditional consideration that atrial extrasystoles are an ECG finding devoid of interest.
Ventricular ExtrasystolesThe prevalence of extrasystoles was 2.8%, a higher value than that reported by Rodríguez-Capitán et al.2 On multivariate analysis, no significant correlation was found with heart failure or other cardiac conditions. On the contrary, participants with ventricular extrasystoles showed a lower prevalence of coronary disease, which is difficult to explain, unless it results from greater use of beta-blockers in this group.
Wolf-Parkinson-White PatternsAs in previous studies, there were very few examples of Wolf-Parkinson-White patterns in our population sample (prevalence, 0.35%). This value is comparable to the figures cited by De Bacquer et al.7 and Rodríguez-Capitán et al.,2 and somewhat higher than the prevalence reported by Rose et al.6 (0.02%).
LimitationsThe design of the study (cross-sectional with a population older than 40 years) implies that conclusions regarding the true prognosis of the ECG findings could not be obtained, and that information on individuals younger than 40 years was unavailable. In addition, it was not possible to verify that the electrocardiograms had been acquired according to proper quality standards (application of filters, adequate voltage and paper speed, etc.). These factors could not be controlled, and the analysis necessarily involved ECG studies performed with different electrocardiographs. This may have had an impact on some diagnoses, but a more rigorous design would have been complex and costly, threatening the feasibility of the study. An advantage of these technical considerations is that they rendered the study more similar to actual clinical practice. Some of these limitations were partly corrected by centralizing the electrocardiogram analysis. With regard to the ECG criteria used, it would have been of interest to differentiate between complete and incomplete bundle branch blocks. These were grouped together to simplify the huge amount of information managed in the study. For the same reason, we did not differentiate between Q wave duration greater or less than 0.04 s. Another important limitation is that complete data were not available for the pharmacological treatment that may have been used by participants, which could have had an impact on the appearance of certain ECG abnormalities: repolarization changes, conduction disorders, etc. The only information in this line was related to antiarrhythmic drug use in participants with AF.
CONCLUSIONSThe prevalence of abnormal ECG findings in an unselected Spanish population sample was very high, around 50%. The most commonly found abnormalities were conduction disorders. Right bundle branch block, the most prevalent in this group, was not associated with heart disease. The remaining conduction disorders were found to be associated with cardiovascular risk factors, at the least. Because of the high prevalence of these findings, all physicians performing ECG examinations (primary care physicians, anesthesiologists, internal medicine specialists, etc.) should undego adequate training in the use of this valuable diagnostic tool.
FUNDINGThe OFRECE study was sponsored by the Research Agency of the Spanish Society of Cardiology. The study was funded by a grant from the Women's Observatory of the Quality Agency of the Ministry of Health and by an unrestricted grant from SANOFI, which did not participate in the study design, data analysis, or manuscript preparation.
CONFLICTS OF INTERESTNone declared.
- –
Few recent population studies have focused on the prevalence of electrocardiographic findings.
- –
Most available studies have an important selection bias: the data are often derived from medical check-ups carried out in the work setting, in which young men are the most highly represented population.
- –
The prevalence data provided by these studies depend to a large extent on the type of population analyzed.
- –
This is the first study conducted in Spain investigating electrocardiographic findings in an unselected population.
- –
The prevalence of disorders is very high. Only half the population studied had strictly normal ECG features.
- –
Multivariate analysis showed that most of the ECG findings analyzed were significantly associated with heart disease or cardiovascular risk factors.
- –
Follow-up studies are needed to determine the true prognostic value of these findings.
Supplementary data associated with this article can be found in the online version, at https://doi.org/10.1016/j.rec.2019.01.001.