To analyze differences between sexes in the clinical management of patients presenting with symptoms of chest pain and/or palpitations within a population-based study.
MethodsThe OFRECE study included a random sample of 8400 individuals from the Spanish population aged 40 years and older; 1132 (13.5%) had previously consulted for chest pain and 1267 (15.1%) had consulted for palpitations and were included in the present study. We calculated both the crude and adjusted odds ratios (OR) of undergoing certain tests and the results of consultations by sex. Adjustment was performed by classic cardiovascular risk factors, a personal history of cardiovascular disease, and a diagnosis of stable angina or atrial fibrillation confirmed in the OFRECE study in each case.
ResultsNo differences were observed in history of consultation for chest pain between women and men (13% vs 14.1%; P=.159) but differences were found in palpitations (19% vs 10.4%, respectively; P <.001). Women who had previously consulted for chest pain underwent fewer echocardiograms (32.5% vs 45.3%, respectively; P <.001), were less frequently referred to a cardiologist (49.1% vs 60.1%; P <.001), were less often admitted to hospital (20.1% vs 39.4%; P <.001), and less frequently received a confirmed diagnosis (60.9 vs 71, 9; P <.001). After full adjustment, all differences decreased and become nonsignificant echocardiograms: adjusted OR, 0.81; 95%CI, 0.60-1.09; referral to a cardiologist: adjusted OR, 0.86; 95%CI, 0.63-1.16; hospital admission: adjusted OR, 0.76; 95%CI, 0.54-1.09). For palpitations, crude differences were smaller and all became nonsignificant after adjustment.
ConclusionsThis study does not confirm the existence of sex-related bias in the management of chest pain and palpitations. However, such bias cannot be completely ruled out in diagnoses confirmed within the OFRECE study, which might limit its ability to detect sex-related differences in health care.
Keywords
The form of presentation of ischemic heart disease often differs between men and women. Chest pain is less common in women, but they show a greater presence of prodromal symptoms, such as shortness of breath or unusual fatigue for weeks or months before an acute ischemic event.1,2 Because the general public and physicians themselves have traditionally perceived that ischemic heart disease typically affects men, the clinical search for symptoms may lack a necessary female orientation. A delay in requesting assistance, together with an implicit bias unnoticed by physicians, may be the reason for delays in detecting ischemic heart disease and deficiencies in its management in women compared with men. These factors all have prognostic implications.3 In the past in Spain, delays in the diagnosis and less extensive use of diagnostic tests in women than in men were reported in the setting of acute coronary syndromes, which would partly explain the worse short-term prognosis.4
Nonetheless, more recently, in patients with confirmed ischemia referred for coronary angiography, no variation was found in the typical symptoms between men and women,5 thus contradicting the notion that the differences in management are based on the presenting symptoms. Furthermore, these differences have not only been described in ischemic heart disease. Women with arrhythmia detected in primary care (PC) are referred less often to a cardiologist, and women with atrial fibrillation (AF) receive a more conservative treatment approach.6,7
The OFRECE study8,9 was conducted to estimate the prevalence of stable angina and AF in 8400 individuals from the Spanish population aged 40 years and older. It included general questions related to symptoms of cardiac rhythm disorders and chest pain to investigate, as a secondary objective, potential health care inequalities between men and women. Hence, it has provided the opportunity to examine differences in the treatment approaches used between sexes based on a confirmed diagnosis of angina or AF.
MATERIAL AND METHODSCross-sectional study conducted in the PC setting of Spain. The main characteristics of the methods have been described previously.8,9 Briefly, the study included 8400 individuals randomly selected from the general Spanish population aged 40 years and older (random sampling in stages), using the health cards from individuals attended in 425 PC consulting rooms in 46 provinces of Spain. Information was collected on the family and personal history of disease, and cardiovascular risk factors, as well as data on AF and angina, obtained using specific questionnaires (London School of Hygiene and Tropical Medicine questionnaire).10 All participants underwent electrocardiography, and the results were centrally interpreted by a small group of cardiologists. Two cardiologists independently read each electrocardiogram, and when there were discrepancies, a third cardiologist participated to resolve them by consensus.11 Individuals with a new diagnosis of angina or AF were referred to a participating cardiologist to confirm the diagnosis and establish the clinical approach.
The PC questionnaire included specific questions related to the history of previous consultations for chest pain or palpitations, and the results of these visits. The content of the questionnaire is shown in Table 1of the supplementary data. Individuals with a history of consultations for the above-mentioned causes are the subject of the present study.
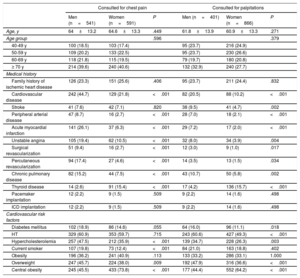
Characteristics of men and women with a history of previous consultations for chest pain or palpitations
| Consulted for chest pain | Consulted for palpitations | |||||
|---|---|---|---|---|---|---|
| Men (n=541) | Women (n=591) | P | Men (n=401) | Women (n=866) | P | |
| Age, y | 64±13.2 | 64.6±13.3 | .449 | 61.8±13.9 | 60.9±13.3 | .271 |
| Age group | .596 | .379 | ||||
| 40-49 y | 100 (18.5) | 103 (17.4) | 95 (23.7) | 216 (24.9) | ||
| 50-59 y | 109 (20.2) | 133 (22.5) | 95 (23.7) | 230 (26.6) | ||
| 60-69 y | 118 (21.8) | 115 (19.5) | 79 (19.7) | 180 (20.8) | ||
| ≥ 70 y | 214 (39.6) | 240 (40.6) | 132 (32.9) | 240 (27.7) | ||
| Medical history | ||||||
| Family history of ischemic heart disease | 126 (23.3) | 151 (25.6) | .406 | 95 (23.7) | 211 (24.4) | .832 |
| Cardiovascular disease | 242 (44.7) | 129 (21.8) | <.001 | 82 (20.5) | 88 (10.2) | <.001 |
| Stroke | 41 (7.6) | 42 (7.1) | .820 | 38 (9.5) | 41 (4.7) | .002 |
| Peripheral arterial disease | 47 (8.7) | 16 (2.7) | <.001 | 28 (7.0) | 18 (2.1) | <.001 |
| Acute myocardial infarction | 141 (26.1) | 37 (6.3) | <.001 | 29 (7.2) | 17 (2.0) | <.001 |
| Unstable angina | 105 (19.4) | 62 (10.5) | <.001 | 32 (8.0) | 34 (3.9) | .004 |
| Surgical revascularization | 51 (9.4) | 16 (2.7) | <.001 | 12 (3.0) | 9 (1.0) | .017 |
| Percutaneous revascularization | 94 (17.4) | 27 (4.6) | <.001 | 14 (3.5) | 13 (1.5) | .034 |
| Chronic pulmonary disease | 82 (15.2) | 44 (7.5) | <.001 | 43 (10.7) | 50 (5.8) | .002 |
| Thyroid disease | 14 (2.6) | 91 (15.4) | <.001 | 17 (4.2) | 136 (15.7) | <.001 |
| Pacemaker implantation | 12 (2.2) | 9 (1.5) | .509 | 9 (2.2) | 14 (1.6) | .498 |
| ICD implantation | 12 (2.2) | 9 (1.5) | .509 | 9 (2.2) | 14 (1.6) | .498 |
| Cardiovascular risk factors | ||||||
| Diabetes mellitus | 102 (18.9) | 86 (14.6) | .055 | 64 (16.0) | 96 (11.1) | .018 |
| HT | 329 (60.9) | 353 (59.7) | .715 | 243 (60.6) | 427 (49.3) | <.001 |
| Hypercholesterolemia | 257 (47.5) | 212 (35.9) | <.001 | 139 (34.7) | 228 (26.3) | .003 |
| Current smoker | 107 (19.8) | 73 (12.4) | <.001 | 84 (21.0) | 163 (18.8) | .402 |
| Obesity | 196 (36.2) | 241 (40.9) | .113 | 133 (33.2) | 286 (33.1) | 1.000 |
| Overweight | 247 (45.7) | 224 (38.0) | .009 | 192 (47.9) | 316 (36.6) | <.001 |
| Central obesity | 245 (45.5) | 433 (73.8) | <.001 | 177 (44.4) | 552 (64.2) | <.001 |
HT, hypertension; ICD, implantable cardioverter-defibrillator
Results are expressed as the mean±standard deviation or No. (%).
The results are reported as the mean±standard deviation or percentage, depending on the type of variable. Comparisons between men and women were made with the Student t test for quantitative variables and the chi-square test for qualitative variables. Independent logistic regression models were performed for patients with a history of consultations for chest pain or for palpitations or dizziness to study the relationship between patient sex (female) and the outcome of the visit (eg, complementary tests, treatment changes). Crude and adjusted odds ratios (OR) were calculated with 95% confidence intervals (95% CI). The simplest adjustment was by age and classic cardiovascular risk factors, whereas the more complex ones included the presence of other conditions and the true clinical situation (diagnosis of angina or AF in each patient).
The OFRECE study was approved by the Clinical Research Ethics Committee of Hospital Universitario de Basurto.
RESULTSOf the 8400 participants included in the OFRECE study, 1132 (13.5% of the total; 48% men and 52% women) had consulted previously for chest pain, with no differences between sexes (14.1% men vs 13.0% women, P=0.159). Furthermore, 1267 (15.1% of the total; 32% men and 68% women) had consulted for palpitations or dizziness, with a significant difference between sexes (10.4% men and 19% women; P<.001). The characteristics of these groups are shown in Table 1. Men and women in the 2 groups differed in almost the same aspects. In particular, diseases and risk factors were more frequent in the personal histories of men, with the exception of thyroid disease and central obesity, which were more common in women.
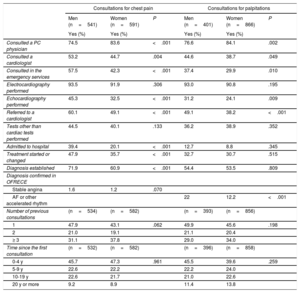
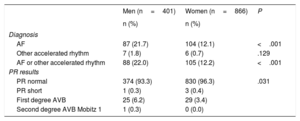
The frequency, type, and outcome of the previous consultations for chest pain and for palpitations or dizziness are summarized by sex in Table 2. With regard to chest pain, there were no differences in the percentage of women and men who had undergone a previous visit for this reason, but women consulted more frequently with a PC physician and men with a cardiologist or in the emergency department. In addition, men underwent a larger number of tests and received a diagnosis more frequently. The prevalence of stable angina confirmed by the OFRECE cardiologist was 1.6% in men and 1.2% in women who had consulted in the past for chest pain (P=.070). As to palpitations and dizziness, the prevalence of a previous consultation for this purpose was almost twice as high in women as in men. As occurred with chest pain, women consulted more often with a PC physician and less often with a cardiologist or in the emergency department, and they underwent fewer tests of certain types (eg, echocardiography) than men, although the differences were less marked than in the case of chest pain. In contrast to the chest pain findings, there were no differences in other outcomes of the previous consultations (hospitalizations, treatment changes, or receiving a diagnosis). Finally, the prevalence of AF and other accelerated rhythms confirmed by the study cardiologist was 22% in men and 12.2% in women previously consulting for palpitations (P<.001).
Comparison of consultations for chest pain or palpitations between men and women, with the outcomes
| Consultations for chest pain | Consultations for palpitations | |||||
|---|---|---|---|---|---|---|
| Men (n=541) | Women (n=591) | P | Men (n=401) | Women (n=866) | P | |
| Yes (%) | Yes (%) | Yes (%) | Yes (%) | |||
| Consulted a PC physician | 74.5 | 83.6 | <.001 | 76.6 | 84.1 | .002 |
| Consulted a cardiologist | 53.2 | 44.7 | .004 | 44.6 | 38.7 | .049 |
| Consulted in the emergency services | 57.5 | 42.3 | <.001 | 37.4 | 29.9 | .010 |
| Electrocardiography performed | 93.5 | 91.9 | .306 | 93.0 | 90.8 | .195 |
| Echocardiography performed | 45.3 | 32.5 | <.001 | 31.2 | 24.1 | .009 |
| Referred to a cardiologist | 60.1 | 49.1 | <.001 | 49.1 | 38.2 | <.001 |
| Tests other than cardiac tests performed | 44.5 | 40.1 | .133 | 36.2 | 38.9 | .352 |
| Admitted to hospital | 39.4 | 20.1 | <.001 | 12.7 | 8.8 | .345 |
| Treatment started or changed | 47.9 | 35.7 | <.001 | 32.7 | 30.7 | .515 |
| Diagnosis established | 71.9 | 60.9 | <.001 | 54.4 | 53.5 | .809 |
| Diagnosis confirmed in OFRECE | ||||||
| Stable angina | 1.6 | 1.2 | .070 | |||
| AF or other accelerated rhythm | 22 | 12.2 | <.001 | |||
| Number of previous consultations | (n=534) | (n=582) | (n=393) | (n=856) | ||
| 1 | 47.9 | 43.1 | .062 | 49.9 | 45.6 | .198 |
| 2 | 21.0 | 19.1 | 21.1 | 20.4 | ||
| ≥ 3 | 31.1 | 37.8 | 29.0 | 34.0 | ||
| Time since the first consultation | (n=532) | (n=582) | (n=396) | (n=858) | ||
| 0-4 y | 45.7 | 47.3 | .961 | 45.5 | 39.6 | .259 |
| 5-9 y | 22.6 | 22.2 | 22.2 | 24.0 | ||
| 10-19 y | 22.6 | 21.7 | 21.0 | 22.6 | ||
| 20 y or more | 9.2 | 8.9 | 11.4 | 13.8 | ||
AF, atrial fibrillation; PC, primary care;
Data are expressed as percentages unless otherwise indicated.
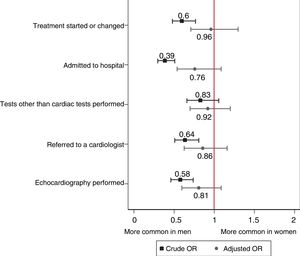
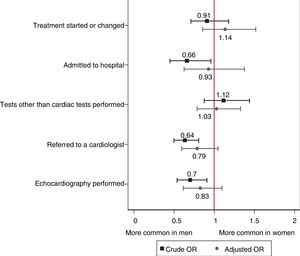
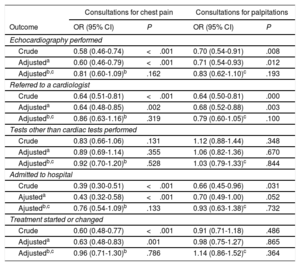
The OR values for performing certain tests in women vs men are shown in Table 3. When no other characteristics were taken into consideration, women had a lower probability of being referred to a cardiologist, receiving an indication for echocardiography, and even being hospitalized. It was also less likely that they would be started on treatment or have their treatment changed. These differences remained after adjustment for the presence of cardiovascular risk factors, but they disappeared when the overall clinical situation was taken into account in the analysis of each case, including the personal history of cardiovascular disease and the confirmed diagnosis of stable angina, AF, or other accelerated rhythms (Figure 1 and Figure 2). The diagnoses confirmed in OFRECE in patients with a previous consultation for palpitations are shown in Table 4.
Crude and adjusted probabilities of the various outcomes between men and women
| Consultations for chest pain | Consultations for palpitations | |||
|---|---|---|---|---|
| Outcome | OR (95% CI) | P | OR (95% CI) | P |
| Echocardiography performed | ||||
| Crude | 0.58 (0.46-0.74) | <.001 | 0.70 (0.54-0.91) | .008 |
| Adjusteda | 0.60 (0.46-0.79) | <.001 | 0.71 (0.54-0.93) | .012 |
| Adjustedb,c | 0.81 (0.60-1.09)b | .162 | 0.83 (0.62-1.10)c | .193 |
| Referred to a cardiologist | ||||
| Crude | 0.64 (0.51-0.81) | <.001 | 0.64 (0.50-0.81) | .000 |
| Adjusteda | 0.64 (0.48-0.85) | .002 | 0.68 (0.52-0.88) | .003 |
| Adjustedb,c | 0.86 (0.63-1.16)b | .319 | 0.79 (0.60-1.05)c | .100 |
| Tests other than cardiac tests performed | ||||
| Crude | 0.83 (0.66-1.06) | .131 | 1.12 (0.88-1.44) | .348 |
| Adjusteda | 0.89 (0.69-1.14) | .355 | 1.06 (0.82-1.36) | .670 |
| Adjustedb,c | 0.92 (0.70-1.20)b | .528 | 1.03 (0.79-1.33)c | .844 |
| Admitted to hospital | ||||
| Crude | 0.39 (0.30-0.51) | <.001 | 0.66 (0.45-0.96) | .031 |
| Ajusteda | 0.43 (0.32-0.58) | <.001 | 0.70 (0.49-1.00) | .052 |
| Ajustedb,c | 0.76 (0.54-1.09)b | .133 | 0.93 (0.63-1.38)c | .732 |
| Treatment started or changed | ||||
| Crude | 0.60 (0.48-0.77) | <.001 | 0.91 (0.71-1.18) | .486 |
| Adjusteda | 0.63 (0.48-0.83) | .001 | 0.98 (0.75-1.27) | .865 |
| Adjustedb,c | 0.96 (0.71-1.30)b | .786 | 1.14 (0.86-1.52)c | .364 |
95% CI, 95% confidence interval; BMI, body mass index; HT, hypertension; OR, odds ratio.
Crude and adjusted odds ratios (ORs) with 95% confidence intervals for the various outcomes in women vs men consulting for chest pain. *Adjusted by age, diabetes, hypertension, hypercholesterolemia, smoking, body mass index, central obesity, family history of ischemic heart disease, stroke, peripheral arterial disease, and diagnosis of stable angina.
Crude and adjusted odds ratios (ORs) with 95% confidence intervals for the various outcomes in women vs men consulting for palpitations. *Adjusted by age, diabetes, hypertension, hypercholesterolemia, smoking, body mass index, central obesity, family history of ischemic heart disease, cardiovascular disease, thyroid disease, and a diagnosis of atrial fibrillation or other accelerated rhythm.
Electrocardiography findings in men and women consulting for palpitations
| Men (n=401) | Women (n=866) | P | |
|---|---|---|---|
| n (%) | n (%) | ||
| Diagnosis | |||
| AF | 87 (21.7) | 104 (12.1) | <.001 |
| Other accelerated rhythm | 7 (1.8) | 6 (0.7) | .129 |
| AF or other accelerated rhythm | 88 (22.0) | 105 (12.2) | <.001 |
| PR results | |||
| PR normal | 374 (93.3) | 830 (96.3) | .031 |
| PR short | 1 (0.3) | 3 (0.4) | |
| First degree AVB | 25 (6.2) | 29 (3.4) | |
| Second degree AVB Mobitz 1 | 1 (0.3) | 0 (0.0) | |
AF, atrial fibrillation; AVB, atrioventricular block; PR, PR interval.
The results of this subanalysis of the OFRECE study indicate that the prevalence of previous medical consultations for chest pain does not differ between men and women. They also show that when the clinical characteristics of these patients are not taken into consideration, medical visits in men generally lead to a larger number of cardiologic tests, specialist referrals, hospital admissions, and treatment changes than in women. In addition, diagnosis is reached more often, although women tended to have a larger number of consultations per person. In contrast, previous medical consultations for palpitations were much more common in women, and as occurred in patients with chest pain, differences were observed in referrals for certain tests (echocardiograms) and cardiology visits, whereas they disappeared for the remaining aspects. In addition, the results for both types of consultations confirmed that women make greater overall use of PC centers, as described previously.12
These differences, at times of considerable magnitude, remained virtually unchanged after adjustment for classic cardiovascular risk factors, whereas they became greatly attenuated and lost statistical significance after additionally adjusting for the cardiovascular disease history and the patient's confirmed diagnosis established in the study.
Differences between women and men regarding the care provided in the setting of coronary disease have been a subject of concern for years. Studies published at the beginning of the 1990s reported evident differences between men and women in the intensity of the diagnostic and therapeutic approaches used for this condition13,14 and stated that once coronary disease had been confirmed, men and women received the same type of management: That is, it was necessary to manifest the disease as a man for a woman to receive the same treatment.
In the case of ischemic heart disease—in particular, although not exclusively, acute coronary syndrome—it has be extensively reported1,15,16 that the forms of presentation of this condition differ between men and women. Whereas these differences may partly reflect pathophysiologic variation between the sexes,17 other factors may also have an influence, such as differences in the patients’ attitude when seeking medical attention for their symptoms, and possibly, even an unintentional implicit bias among health professionals, introducing gender differences beyond gender-related differences.3 This has generated constant concern and has led to far-reaching initiatives at several levels, including intensified research in the diagnosis, treatment, and prevention of ischemic heart disease in women,18,19 in-depth reflection and position-taking in scientific societies specifically addressing the particularities of this condition in women,20–24 and programs promoting awareness and information, such as Go Red for Women from the American Heart Association,25 which have improved the situation of ischemic heart disease in women.
In Spain, the strategy for ischemic heart disease includes among its aims promotion of a gender approach in all heart disease research.26 As the Spanish Society of Cardiology (SEC, Sociedad Española de Cardiología) responds to that same concern, the present article is a part of this objective, and it is a continuation of a broader initiative formulated some years ago.27 The disappearance of differences in the tests carried out between sexes as well as the success of the diagnostic process after adjustment for the true clinical situation (ie, confirmed diagnoses within the OFRECE study), indicate that there is very little or no gender bias in the diagnostic approach and decisions made for men and women consulting for chest pain in our setting. In general, these findings are also seen in the case of palpitations, a consultation in which the diagnosis, despite the differential data regarding arrhythmia in women, is less dependent on the patient's sex.28
The available information had some limitations for responding to the question formulated. The main limitation is that angina screening was first performed in the PC setting with the Rose questionnaire (which includes only chest pain) and a review of the patient's medical history. It could be that the diagnosis was better collected in the clinical history of men because of a more intense diagnostic effort in the past. In addition, the cardiologists participating in OFRECE, who were responsible for confirming the diagnoses later used for adjusting the models, may have been more stringent when “labelling” women than men, as the evaluation was in no way blinded. Chest pain is the most widely recognized symptom of myocardial ischemia. As mentioned, this symptom is found more often in men than in women,16 and this lower prevalence of chest pain at presentation is related to a worse prognosis, with a difference that decreases with age.29 However, it is possible that the methods used to identify the symptoms, in themselves, may be biased from the gender perspective. Several studies have reported no gender differences in the frequency of chest pain, and this absence of differences is much more common in studies that use open questions to identify symptoms than those with closed questions, as in check-lists, which admit only a series of prespecified symptoms.5 Regarding differences in cardiovascular disease (also an adjustment variable in the present study), most dissimilarities between men and women were related to differences in acute myocardial infarction and unstable angina, conditions that require hospitalization. For this reason, although it is plausible that there could be gender differences in the diagnostic delay in these conditions, it is less likely that these differences would be present in the diagnosis at middle term. For its part, the Rose questionnaire shows greater sensitivity in women than men, although specificity is lower,30,31 and in this case it is not reasonable to consider that excessive adjustment could cancel out the differences. The prevalence of angina determined with the Rose questionnaire is higher in women than in men in a variety of countries and populations,15 and this was also seen in OFRECE,9 with differences that disappeared when the cardiologists’ confirmed diagnoses were taken into account, and these were the values used for adjusting the models.9 This approach is limited, however, as the diagnosis was confirmed at some time after the consultations for palpitations and chest pain with their outcomes; hence it can only be considered an approximation of the true situation of patients at the time of consultation. Furthermore, with regard to palpitations, the questionnaire used to collect the information in this study, focused on the diagnosis of AF, did not enable evaluation of the period before the diagnosis was established or provide information on whether women had a previous diagnosis of anxiety, as is often the case. The lack of suitable variables in the questionnaire also impeded adequate evaluation of the patients’ history of other arrhythmias; hence, adjusting of the models may have been incomplete.
In summary, in absolute terms, this study found that women are referred less often than men to a cardiologist and they undergo fewer tests when consulting for chest pain or palpitations, regardless of their cardiovascular risk. Nonetheless, after adjustment of these data by the final diagnosis, the results did not indicate gender bias in the care provided to patients with symptoms of chest pain or palpitations. The differences observed between men and women could be explained by the clinician's general consideration of the patient's profile, in a type of “self-fulfilling prophesy”. Doubts will always remain as to whether there could be a background gender bias, in which the participating cardiologists underdiagnosed the women in this study. It is desirable that the greater focus on reducing inequalities in health care to women in recent years from several viewpoints will decrease the gender differences found in the past. Similarly, it has been indicated that differences in prognosis, also noted in Spain at the end of the past century4 may be decreasing with generalized incorporation of cardiac revascularization as a standard treatment for acute coronary syndrome.32
Future studies that use a gender-conscious design and data analysis will help to elucidate how this factor influences patients and their attending medical professionals.
CONCLUSIONSThe results of his study do not confirm the existence of gender bias in the care of patients with symptoms of chest pain or palpitations, although gender bias in the diagnoses confirmed in the study cannot be completely ruled out. This latter element could limit the ability of the study to detect differences in the health care provided to these patients.
FUNDINGThis subanalysis of the OFRECE study was promoted by the SEC Women in Cardiology Working Group. The Prevalence Study of Atrial Fibrillation and Stable Angina in the General Population of Spain (OFRECE) is a project of the SEC Research Agency. It was funded by a grant from the Women's Observatory of the Quality Agency of the Ministry of Health (pilot phase) and with an unconditional grant from SANOFI, which did not participate in the design of the study, the data analysis, or preparation of the manuscripts.
CONFLICTS OF INTERESTThe institution where J. Muñiz works has received fees from the SEC for consulting related to statistical data analysis, preparation of preliminary versions of the manuscript, and administrative support in the publication process. J.J. Alonso Martín has received compensation from the SEC for traveling to meetings or other tasks related to this study.
- –
The form of presentation of ischemic heart disease differs between men and women, and there is a higher incidence of this condition in men. Consequently, a necessary female orientation may be lacking and lead to deficiencies in the management of this condition in women compared with men, as has been reported in the past.
- –
Similar differences have been observed in the case of arrhythmias, and it is important to determine whether this situation persists in Spain to guide the recommendations for these conditions.
- –
This study provides an updated population-based reassessment of potential gender bias in health care in Spain, which was not confirmed. The differences in care between men and women consulting for chest pain and for palpitations were explained by the clinical condition confirmed in the diagnosis.
Supplementary data associated with this article can be found in the online version available at http://dx.doi:10.1016/j.rec.2018.11.021.