Keywords
INTRODUCTION
Chest pain is one of the most common reasons for consulting in the emergency department and is present in 5%-20% of patients who go to the emergency room of a general hospital.1 One of the fundamental objectives of chest pain units (CPUs) is to identify rapid and efficiently low-risk patients who do not require hospitalization. Although the data on CPUs in Spain are still limited,2-5 these units attend to patients with chest pain or any other symptom indicating coronary ischemia, based on rapid classification into various risk groups.1-4,6-11
The medical history, physical examination, electrocardiogram (ECG), and chest x-rays are useful for assessing chest pain, although they have limitations.12 Resources are also limited and most centers are unable to carry out tests to detect ischemia in all candidate patients with chest pain, making it important to obtain the maximum prognostic value from the clinical information. Nevertheless, the usefulness of the various clinical variables and the way to include them in patient stratification is not well defined. Our principal aim was to assess the value of clinical variables for determining whether patients admitted to a CPU of a tertiary hospital might present coronary disease, and the secondary aim was to predict events during CPU admission and follow-up of these patients.
PATIENTS AND METHOD
We consecutively studied 379 patients admitted from July 2003 to September 2004 to the CPU of our center. The clinical data, including personal and medical history, characteristics of the pain and concomitant treatment were prospectively recorded during the CPU stay by means of a standardized form. Fourteen patients (3.7%) were excluded because of missing data; hence the final study population included 365 patients.
Criteria for CPU Admission
Patients were included if they had chest pain consistent with an acute coronary syndrome (ACS) without clinical or electrocardiographic criteria indicating high risk, and if they met the following criteria: 1) physical examination showing no evidence of ventricular dysfunction, heart failure or significant valvular disease; 2) ECG demonstrating no significant repolarization alterations or newly-developed complete left bundle-branch block; 3) pain duration <60 min; 4) initial analyses showing no significant anemia or abnormal in potassium concentration; 5) chest x-ray with no findings indicating aortic dissection or heart failure; and 6) informed verbal consent granted for admission to the CPU.
CPU Protocol
When a patient fulfilled the criteria, the cardiologist on call was notified to admit the patient to the CPU where he/she underwent continuous electrocardiographic monitoring. Subsequently, a single 300-mg dose of aspirin was administered, or in cases of allergy or contraindications, 150 mg of clopidogrel. An ECG was performed and troponin T concentrations were determined 6 and 12 h after the onset of chest pain.5 Patients without significant electrocardiographic changes or elevated troponin T values (<0.01 ng/mL) 12 h after the last episode of chest pain underwent a test to detect ischemia (treadmill stress testing or stress echocardiography) according to the criteria of the cardiologist in charge of the CPU, who also determined whether the patient would undergo coronary angiography. The stress test was considered positive, negative or inconclusive according to the Sociedad Española de Cardiología (Spanish Society of Cardiology) guidelines.13
Criteria of Coronary Disease
The presence of coronary disease was only assessed in patients who underwent a test for detection of ischemia (n=322, 88.2%). A patient was considered to present significant coronary disease when: 1) coronary angiography showed >70% stenosis of a coronary artery (in undetermined cases, intravascular ultrasound was performed following the criteria of the interventional cardiologist) (n=34, 10.6%), or 2) the ischemia detection test was positive in those who did not undergo coronary angiography (n=13, 4.0%). Patients who had a conclusive negative ischemia detection test were considered not to present coronary disease (n=236, 73.3%). Patients with a non-conclusive ischemia detection test were not included in the analysis for the presence of coronary disease (n=39, 12.1%).
Statistical Methods
Categorical values were assessed using a χ² test (or Fisher's exact text when indicated) and continuous variables using a Student s t test or ANOVA for trends, in the presence of a normal distribution; the confidence interval (CI) for the proportions was calculated using the exact method. To study the independent predictors of coronary disease, multivariate analysis was performed with logistic regression by backward stepwise elimination, including the following clinical variables: age >64 years, sex, cardiovascular risk factors, cardiovascular history, chest pain classified as typical by the attending physician, use of aspirin, and systolic arterial pressure and heart rate at the time of admittance. The odds ratio (OR) was expressed with the respective 95% CI. A score was developed with the independent predictors of coronary disease and post hoc assessment was done to determine the relationship between this score and the remaining variables. The statistical analyses were done with SPSS, version 11.0 for Windows (SPSS Inc., Chicago, Illinois, USA).
RESULTS
Mean age was 62.3±13.5 years. The baseline characteristics of the patients are shown in Table 1. Mean duration of the stay in the emergency room-CPU was 21.1±6.5 h, with a median of 21.6 h. A total of 40 patients (11.9%) presented pain upon arrival to the emergency room and the median interval from the onset of pain to emergency room admittance was 2.5 h. Chest pain was classified as typical in 122 patients (33.4%), inconclusive in 169 (46.3%) and atypical in 74 (20.3%). The mean score of Geleijnse et al14 (Appendix 1) was 7.7±3.4, and the score for each of the above groups was 9.1±3.1, 7.0±3.4, and 6.6±3.2, respectively (P<.001). The drugs most frequently taken by the patients on a regular basis were aspirin in 124 (34.0%), angiotensin-converting enzyme inhibitors or angiotensin II receptor antagonists in 87 (23.8%), beta-blockers in 71 (19.5%), calcium channel blockers in 57 (15.6%), nitrates in 52 (14.2%), and clopidogrel in 31 (8.5%).
The reasons why ischemia detection tests were not performed in 43 patients (11.8%) during their CPU stay were: significant elevation of plasma troponin T concentrations (n=10, 2.7%), recurrent chest pain (n=9, 2.5%), changes in serial ECGs (n=5, 1.4%) or other reasons, including inability to perform the ischemia detection test due to logistics (n=19, 5.2%). Tests to detect ischemia included treadmill stress testing in 225 patients (69.9%) and stress echocardiography in 97 (30.1%). No major complications occurred during the CPU stay except for 2 cases of transient ST segment elevation (1 during dobutamine echocardiography and 1 after the treadmill test), which required admittance to the coronary care unit and urgent catheterization; there was no elevation of myocardial injury markers.
The treadmill test was performed according to the Bruce protocol and was clinically positive in 16 patients (7.1%) and electrically positive in 25 (11.1%), including the 16 patients mentioned plus other 9. Stress echocardiography was mainly performed with dobutamine (exercise echocardiography in 1 patient and dipyridamole stress in 5), with clinically positive results in 17 patients (17.5%), electrically positive results in 14 (14.4%), and positive echocardiography in 27 (27.8%).
A total of 79 patients (21.6%) were admitted to the cardiology ward. The average length of ward stay was 5.6±4.3 days, with a median of 4.4 days. Coronary angiography was performed in 69 patients (87.4% of hospitalized cases). Among them, 49 patients (75.4%) presented significant coronary disease: 23 single-vessel, 15 double-vessel, 7 triple-vessel, and 4 left main disease. In addition, 3 patients presented vasospasm confirmed by the ergometrine test. Among the 18 patients who underwent coronary angiography on the basis of a positive treadmill test, only 2 (11.1%) cases were false positives. Among the 25 patients who underwent coronary angiography on the basis of a positive stress echocardiography study, there were 7 (28.0%) false positives.
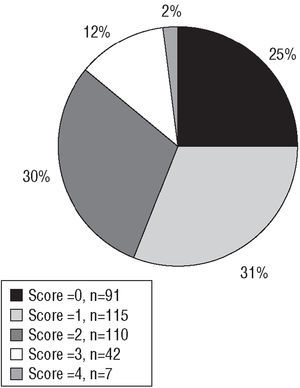
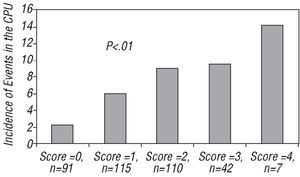
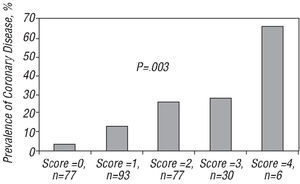
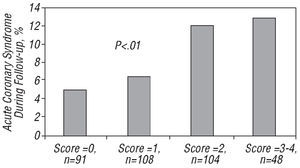
The variables associated with the presence of coronary disease (significant stenosis on coronary angiography or positive ischemia test without coronary angiography) are shown in Table 2. Multivariate analysis confirmed the predictive value of the presence of typical chest pain, use of aspirin, diabetes, and age >64 (Table 3). By combining and adding up these four variables we obtained a risk score ranging from 0 to 4 (Figure 1). The risk score presented a direct relationship with: 1) events during CPU stay, which ranged from 2.2% in patients with a score of 0 (95% CI, 0.3%-77.1%) to 14.3% in patients with a score of 4 (95% CI, 0.6%-80.5%) (Figure 2); 2) presence of coronary disease, which ranged from 3.9% in patients with a score of 0 (95% CI, 0.8%-13.4%) to 66.7% in patients with a score of 4 (95% CI, 22.2%-95.6%) (Figure 3); and 3) false-positive results on the stress echocardiogram: 2 (67%) in patients with a score of 0, 2 (40%) in patients with a score of 1, and 3 (30%) in patients with a score of 2, whereas the 7 positive results in patients with a score of 3 or 4 were true positives (P<.001).
Figure 1. Distribution of the risk score (consisting of a combination of the following variables: typical chest pain, use of aspirin, diabetes, and age >64 years and quantified from 0 to 4) in 365 patients admitted to a chest pain unit.
Figure 2. Incidence of electrocardiographic changes, recurrent chest pain, or elevated troponin T concentrations during the observational phase in the chest pain unit (CPU), according to the number of risk variables present: (typical chest pain, use of aspirin, diabetes, and age >64 years) in the 365 patients studied.
Figura 3. Prevalence of coronary disease according to the number of risk variables present (typical chest pain, use of aspirin, diabetes, and age >64 years) in the 283 patients who had a conclusive ischemia detection test in the chest pain unit.
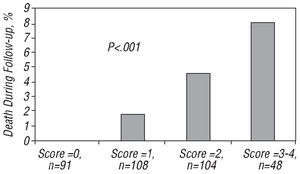
Telephone follow-up over a period of at least 3 months was performed in 351 patients (96.1%); mean follow-up time was 9.1±3.1 months and the median was 9.2 months. A total of 11 patients (3.1%) died during follow-up: 8 due to non-cardiac causes, 1 due to heart failure, 1 after myocardial infarction, and 1 due to sudden death. The risk score was associated with mortality by any cause during follow-up (Figure 4). The death after myocardial infarction and the sudden death occurred in patients with scores of 3-4 and the death due to heart failure in a patient with a score of 2. In 30 patients an ACS was observed during follow-up (8.5%). The risk score was also associated with development of an ACS during follow-up (Figure 5).
Figure 4. Overall mortality during follow-up according to the number of risk variables present (typical chest pain, use of aspirin, diabetes, and age >64 years) in the 351 patients followed-up for at least 3 months.
Figure 5. Incidence of acute coronary syndrome during follow-up according to the number of risk variables present (typical chest pain, use of aspirin, diabetes, and age >64 years) in the 365 patients followed-up for at least 3 months.
DISCUSSION
Chest pain units were created to reduce the number of patients hospitalized for chest pain of non-coronary origin15 as well as the number of discharges of patients with an ACS,16-19 and to optimize the cost of care for this population.20,21 In patients with a normal ECG or one that is non-diagnostic for ischemia, and in whom a coronary origin cannot be definitively ruled out, a fast diagnostic approach is adopted, with additional tests that allow the presence of heart disease to be confirmed or excluded.1-4,6-11 These tests generally consist in assessment of markers of myocardial injury (usually troponin5) and a test to detect ischemia.6-11 When one of these tests is positive, the patient is usually hospitalized, whereas when both are negative6 or indicate low risk,4 the patient is discharged from the emergency room. However, this strategy requires availability and a degree of organization that is not within the reach of all centers, or is not available to all candidate patients; such as, those who go to the emergency room with chest pain and suspected ACS, but have no high-risk criteria. Moreover, this approach does not take into account clinical variables that may also be useful in the decision-making process, and although the number of unnecessary hospitalizations and inappropriate discharges of patients with ACS has decreased, both figures are still higher than 5%.11
The present study analyzes a population of patients admitted to a CPU with a mean Geleijnse score14 of 7.7, a figure similar to the 8.6 reported by Sanchis et al2 in another CPU in Spain. In the setting of patients typically admitted to a CPU, we found that four clinical variables quite readily obtained when recording the medical history (typical chest pain, chronic use of aspirin, diabetes, and age >64 years) each increased by two- or three-fold the possibility of presenting coronary disease in patients with chest discomfort consistent with an ACS, but with a normal or nondiagnostic ECG for ischemia. Assessment of whether chest pain was typical or atypical was performed subjectively, in most cases by physicians who were not cardiologists. Nonetheless, the clear difference observed in the mean Geleijnse score, 9.0 for patients with typical pain and 6.7 for those with atypical pain, suggests that the assessment is valid. Chronic use of aspirin coincides in many cases with a history of prior cardiovascular disease, but the slightly higher percentage of patients using aspirin with respect to those with a ca rdiovascular history shows that this variable also allowed patients in whom the drug was used for primary prevention to be included. With regard to diabetes and age, classically related to the presence of coronary disease, these factors were included as dichotomous variables with the aim of obtaining a simple score with possible clinical utility.
The combination of these 4 variables in a score allowed detection of patients with a low probability of presenting coronary disease; i.e., those with non-characteristic chest pain, age <65 years, non-diabetic and not taking aspirin regularly. These patients had a <4% prevalence of coronary disease. Of note, this group was quite numerous (n=91), comprising a quarter of the series and these patients did not present any event during their CPU stay, and angiography revealed coronary disease in only 2 patients, both cases being single-vessel disease. Moreover, in one patient angiography only showed a radio-opaque image consistent with a thrombus in one diagonal branch, which had disappeared on repeat coronary angiography after 5 days. In this group, positive ischemia detection tests must be interpreted with caution, since, as was seen in the stress echocardiography results, up to 2 out of every 3 positive tests can be false positives. In fact, it may be questionable that a patient with a risk score of 0 will benefit from the CPU stay (Table 4). None of these patients presented events during their time in the CPU, nor did any of them die during follow-up. At the other end of the spectrum are the 44% of patients with a risk score of 2-4 and a probability of coronary disease of 27%-67%. Physicians should be particularly cautious before proceeding to discharge these patients.
Limitations
The data presented reflect the daily clinical practice in a CPU. We do not know whether the score described will be useful in other populations. In addition, because the variables forming the basis for the score were obtained from an analysis of our data, definitive validation of the score should be performed in another population. Moreover, there was some selection bias, since we only analyzed CPU patients. Since coronary angiography was not available in all the patients, it is possible that some of those included in the coronary group did not have coronary disease, and vice versa. Lastly, the small number of patients in each subgroup made the estimations imprecise, particularly in those with a risk score of 4.
CONCLUSION
In a population of patients admitted to a CPU with a normal or nondiagnostic electrocardiogram, the following factors were associated with an higher probability of presenting coronary disease: typical chest pain, chronic use of aspirin, diabetes, and age >64 years. The combination of these 4 variables in a risk score could be useful for clinical purposes or for resource management related to these patients.
ACKNOWLEDGEMENTS
We wish to thank all the physicians and nurses in the cardiology and emergency services who were directly involved in the CPU, in patient follow-up and monitoring, and in conducting the tests for ischemia detection.
Correspondence: Dr. H. Bueno.
Servicio de Cardiología. Hospital General Universitario Gregorio Marañón.
Dr. Esquerdo, 46. 28007 Madrid. España.
E-mail: hecbueno@jet.es