Keywords
INTRODUCTION
Despite advances in its treatment, acute myocardial infarction (AMI) continues to be one of the main causes of death in industrialized countries.1 Patient prognosis depends on a number of factors such as age, history of coronary disease, concomitant disease, and the location of the infarction. However, the most important prognostic variables are related to the extent of the damage caused to the myocardium, the release of different enzymes, signs of heart failure, the size of the heart, and the ejection fraction (EF).2-5
Heart failure is an important factor that influences morbidity and mortality in both the short and long term.6-9 Earlier studies have shown the incidence of heart failure to be variable, ranging from 3%-22% in patients who have suffered their first infarction,10 and up to 33% in patients who have suffered a previous infarction.11,12 In the prethrombolytic era, in-hospital mortality was more than 3 times higher in patients with heart failure.1 Later, with the advent of thrombolysis, it was recorded as ranging between 15% and 40%, with an annual rate of 25%-55%.7,12-16 Early recognition of heart failure and its prevention might reduce morbidity and mortiality.9
Data are available on differences between Hispanic and non-Hispanic populations with respect to the clinical characteristics, progress, and long-term prognosis of patients with AMI.17-19 However, very few studies have focused on the development of heart failure in AMI patients in Latin America--and given that these populations are composed of different racial groups, the data for Hispanic patients are probably not applicable. The hypothesis of the present work was that, in a non-selected cohort of Latin American patients with AMI, those who develop heart failure are likely to experience more serious in-hospital and late outcomes than patients who do not develop heart failure, and that the determination of predictors of mortality should permit the early identification of those patients most at risk. The aim of the study was to determine the clinical progression characteristics and the long-term prognostic importance of the development of heart failure in patients hospitalized for AMI.
PATIENTS AND METHODS
Study Population
This work was designed as an observational, prospective study. The study subjects were 836 consecutive patients, all with a diagnosis of AMI, admitted to the intensive coronary care unit of the Instituto de Cardiología de Corrientes between 1 May 1990 and 1 March 2000. All patients were admitted within 24 h of the onset of symptoms and met the inclusion criteria outlined below.
Inclusion Criteria
All patients were required to have a diagnosis of AMI and to meet 2 of the following 3 criteria: a) typical precordial pain lasting more than 20 min; b) new or presumably new electrocardiographic changes consistent with an ST segment elevation of 0.2 mV in 2 or more contiguous leads or ≥0.1 mV in the limb leads, a persistent depression of the ST segment by ≥0.1 mV in 2 or more contiguous leads or in the limb leads, or finally, a new block of the left bundle branch or a persistent inversion (>24 h) of the T wave; c) an increased total creatine kinase (CK) level (≥ twice the normal value), or a CK-MB/ total CK ratio of >10%. The latter was necessary to confirm the diagnosis.
Exclusion Criteria
Patients with the following conditions were excluded from the study: those with cardiogenic shock at admission (defined as sustained hypertension with a systolic blood pressure of <90 mm Hg for more than 30 min with signs of peripheral hypoperfusion; patients that went into cardiogenic shock after 60 min were admitted), suspected myocarditis, pulmonary embolism, congenital disease, dilated cardiomyopathy, valve disease, or pericardial disease. Patients whose follow-up was difficult were also excluded.
Study Protocol
The study protocol was approved by the Teaching and Research Committee of our institution. All patients gave their written consent to be included in the study.
Patients were admitted to the cardiac intensive care unit. Their complete medical histories were recorded and all underwent a physical examination, a 12 lead electrocardiogram (ECG) at admission and 2 h after beginning the reperfusion strategy, a chest x-ray at admission and at 24 h post-admission, and CK and CK-MB) analysis at admission and again 2 h later, or at the beginning of the reperfusion strategy and then again at 6, 12, and 24 h followed by every 24 h until normalization was achieved. A two dimensional echocardiogram was performed within 24 h of admission by an experienced echocardiographer, using a Siemens Sonoline SI 1200 apparatus (Siemens Ultrasound Inc., San Ramon, California, USA). The ejection fraction (EF) was calculated in 745 patients using the Simpson method.
Definitions
Heart failure was defined as the presence of typical symptoms, rales during auscultation, a third heart sound with gallop, evidence of pulmonary congestion in chest x-rays (redistribution of fluid, interstitial and/or alveolar edema), plus the need to begin treatment with intravenous diuretics, vasodilators and/or inotropic drugs.
Q wave infarction was defined after 24 h according to the presence of new Q waves in the V1-V3 leads, or the development of Q waves of ≥0.03 s in leads I, II, aVL, aVF, V4, V5, and V6. When these conditions were not met, a diagnosis of infarction without Q wave was established.
Follow-up and End Point
Final data analysis was performed 2 months after the inclusion of the last patient. This involved the use of our institution's medical records. Patients were assessed by their hospital cardiologist (53%), by their referring cardiologist (34%), by telephone interview, or by their personal physicians at other centers (13%). Mean follow-up time was 43±33 months (range, 0.3-130 months); median follow-up time was 37 months (interquartile range, 25-75 months) The end point was death by any cause during follow-up.
Statistical Analysis
The Pearson *2 test was used to compare the categorical variables (expressed as percentages) of patients with and without heart failure. Quantitative variables were expressed as means ± standard deviation (SD) and were analyzed using the Student t test when their distribution was normal, and by the Mann-Whitney test when not. Kaplan-Meier survival curves were plotted and compared using the log-rank test. Significance was set at P<.05. The Cox proportional test was used to identify independent predictors of mortality; the variables included were age, sex, EF, blood pressure at admission, leukocyte count, glycemia at admission, and heart failure. All calculations were performed using SPSS 10.0 software for Windows (SPSS Inc., Chicago, Illinois, USA).
RESULTS
Patient Characteristics
Of the 836 patients included in the study, 263 (31.5%) developed heart failure. The latter patients (group 1) were significantly older and a significantly greater number were diabetic or had suffered prior heart failure. In addition, significantly more of these patients used angiotensin converting enzyme inhibitors (ACEI) and diuretics (Table 1).
Group 1 patients also had a faster heart rate and less pain at admission. The location of the infarction was more frequently anterior in these patients. The percentage of patients with infarction with Q wave was similar in both groups (Table 2).
Treatment
In patients with AMI with Q wave, reperfusion through the use of thrombolytic agents was more common among those who did not have heart failure. The number of patients in both groups who received primary angioplasty was similar. Patients with heart failure were more commonly administered nitroglycerine, furosemide, ACEI, and heparin, and were more commonly prescribed oral beta-blockers (Table 3).
Laboratory and Echocardiogram Results
No significant differences were seen between the 2 groups with respect to hematocrit levels. However, significant differences were observed in maximum CK levels, leukocyte count, and glycemia at admission. The EF was lower in patients with heart failure (Table 4).
In-Hospital Progress and Long-Term Survival
In-hospital mortality among the patients with heart failure was 6 times greater (15.6% vs 2.3%; P<.001). Complications were more common in group 1 patients, who suffered a greater incidence of postinfarction angina (26.8% vs 19.6% in those who did not develop heart failure; P=.02), pericarditis (17.5% vs 6.3%; P<.001), complex arrhythmias (37.3% vs 27.3%; P=.01), atrial fibrillation (12% vs 5%; P<.01), complete right bundle branch block (13.6 vs 3.6%; P<.01), and left anterior hemiblock (6.6 vs 2%; P=.02).
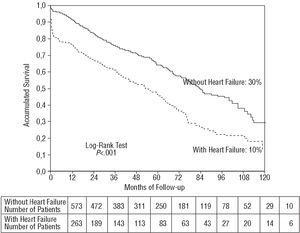
Survival at 120 months was 10% among patients with heart failure and 30% among those without this complication (P<.001; Figure). A wide separation was seen between the survival curves in the first 6 months, which was maintained.
Figure. Ten year survival of patients with and without heart failure.
Prognostic Predictors
The Cox proportional test (which included the variables age, sex, EF, blood pressure at admission, leukocyte count, glycemia at admission, and heart failure) showed the following to be independently associated with mortality during follow-up: age (hazard ratio [HR]=1.022), glycemia (increase in HR of 1.748 for every 1.0 g/L), leukocyte count at admission (increase in HR of 1.035 for every 1000 cells/μL), and development of heart failure (HR=1.308) (Table 5).
DISCUSSION
The results of this study show that heart failure occurs frequently during the acute phase of AMI and that this negatively affects both in-hospital and long-term prognosis. The appearance of heart failure, age, glycemia at admission, and the leukocyte account were all found to be independent predictors of mortality during later follow-up.
Proportion of Patients With Heart Failure
In the prethrombolytic era, it is reported that early development of heart failure occurs in 10%-19% of patients, whereas this develops in 30% during the first year of follow-up.2,7,16 The incidence of this problem is most likely related to the delay between the onset of symptoms and medical consultation, the location of the infarction, and in the case of randomized trials and registries, the time between symptom onset and inclusion. In clinical trials with strict inclusion criteria, the incidence of heart failure appears somewhat lower, from 11.5% in the early phase and 12.5% in the late phase in the GISSI study,6 to 19% in the TAMI subanalysis.11 However, one third of patients in the 4 randomized trials on thrombolytic therapy developed this problem (32.5% in the USA and 26.9% in the remaining countries).20 The 31.5% incidence recorded in the present work is greater than that in previous studies due to the use of non-selected patients, all of whom were admitted within 24 h of symptom onset.
Adjunct Therapy
Anti-neuroendocrine treatment with beta-blockers and ACEI is associated with a significant reduction in mortality and morbidity in AMI.21 A metananlysis of studies investigating the use of ACEI showed a 28% reduction in mortality, infarction and admission to hospital for heart failure in patients with ventricular dysfunction following an AMI.22 The present work shows that ACEI were more commonly used in patients with heart failure, while in patients without this complication, their use was restricted to just one quarter. Clearly, this does not coincide with the recommendations of current treatment guides.23 However, this might be due to the time period over which this study was performed.
The use of beta-blockers provides greater benefits to patients with heart failure24,25; this is especially true with respect to carvedilol.26 In light of current recommendations,23 these agents were also underused in the group of patients who developed heart failure.
The use of reperfusion strategies was relatively low in both groups among patients with Q wave AMI. This might be explained by the late admission of patients referred from other centers, and by the inclusion period of the study (primary angioplasty has become more common since 1997).
In-Hospital and Long-Term Mortality
The in-hospital complication rate was higher among patients who developed heart disease. The in-hospital course of these patients was more serious, in agreement with the results of previous studies.16-27,28 In-hospital mortality in the present work was 6 times greater among patients with heart failure; in addition, their 10 year survival rate was only 10% compared to 30% for the patients without heart failure. In earlier randomized trials with follow-up periods of 10 years,29 mortality in general was 46%--much lower than that seen in the present study. This is probably due to differences in patient selection and patient characteristics.
Predictors of Late Mortality
A number of prognostic variables have been recorded for AMI patients during long-term follow-up.12 In the present study, the development of heart failure was found to be an independent marker of long-term mortality. Those patients with most severe heart failure had a greater number of comorbidities and showed a higher mortality rate.30 Regional differences in hospital management of these patients play a role in the progress of heart failure and therefore also in the in-hospital and long-term prognosis.30 In the PRIAMHO study, patients in Killip class III-IV had a 10-fold greater risk of death within 28 days of their infarction.32
Age was one of the most important short- and long-term predictors of mortality.11 In the GUSTO I trial, 30 day mortality rates of 3% were recorded for patients <65 years of age, whereas those aged 65-74 had a rate of 9.5%, those aged 75-84 had a rate of 19.6%, and those aged ≥85 had a rate of 30.3%.31 In the PRIAMHO study,32 age was also found to be an independent predictor of mortality, with results similar to those of the present study. The reasons for increased mortality among older patients might include: a greater prevalence of prior necrosis and more diffuse heart di sease, comorbidity, abnormalities in the microcirculation, increased pre-capillary resistance, reduced collateral circulation, and delay in seeking help due to atypical symptoms.33
Hyperglycemia is common in patients with AMI and is an independent predictor of cardiovascular risk.34 In the present work, for every increase in blood sugar of 1.0 g/L at admission, the risk of mortality rose by 1.7-fold during follow-up. A number of mechanisms might be responsible, such as an increase in noradrenaline and cortisol levels in the acute phase of the infarction; this would impede the insulin response. In addition, hyperglycemia can have toxic effects on cell function via the formation of free radicals (which can mediate vasoconstriction), on the activation of coagulation, and an increase in the expression of adhesion molecules. It may also have negative effects on endothelium-dependent vasodilation, leading to a worsening of ischemia symptoms.
An increased leukocyte count at admission (a marker of inflammation) is also associated with adverse progress at 30 days.35 In the present work, the leukocyte count at admission was found to be an independent predictor of late mortality, with a 3% increase in risk for every increase of 1000 cells/μL.
Limitations
The results of this single center study may not be extrapolated to the general population. The inclusion of patients with AMI up to 24 h post event might have influenced the use of reperfusion strategies. In addition, these results were collected between 1990 and 2002 and should be analyzed bearing in mind that primary and late angioplasty is far more common nowadays. Nonetheless, the results probably reflect the reality of many centers in Latin America. Due to the length of the study period, the AMI recorded were classified as being with or without a Q wave in ECG readings, rather than by the presence or absence of a raised ST segment.
Clinical Implications
This work confirms that heart failure occurs in up to one third of patients hospitalized with AMI, and that it is an important problem given its associated high in-hospital and 10 year mortality rates. It therefore precedes chronic heart failure.
The present findings point out the need to make an early diagnosis of AMI, to rapidly undertake reperfusion strategies,23 and to use therapies of known efficacy. These might reduce the prevalence of heart failure and its clinical consequences.
CONCLUSIONS
Heart failure is a common complication of AMI and is associated with high in-hospital and long-term mortality. Clinical and simple analytical variables such as the development of heart failure during hospitalization, age, and blood sugar level and the leukocyte count at admission, appear to be predictors of late mortality.
Correspondence: Dra. S.M. Macín.
Unidad de Cuidados Intensivos Coronarios. Instituto de Cardiología Juana F. Cabral.
Bolívar 1334. 3400 Corrientes. Argentina.
E-mail: macinucic@hotmail.com/smacin@gigared.com.ar