Atrial fibrillation occurs in 5%-15% of elderly patients and causes one-fourth to one-fifth of all cerebrovascular events. These patients are frequently asymptomatic. We conducted a public campaign aiming to evaluate the effectiveness of a program for information on and diagnosis of atrial fibrillation in individuals aged 65 years old or more from the primary care perspective.
MethodsWe sent letters containing informative materials and an invitation to attend a special nurse appointment to all individuals≥65 years old, without a previous diagnosis of atrial fibrillation or flutter. Patients were from 3 specific areas in Pontevedra province. The procedures were performed according to a specially designed program called “Pulse Week” within 5 working days. A group of trained nurses obtained a brief medical history and performed pulse palpation for 15 s and blood pressure measurement. A complete 12-lead electrocardiogram was performed if arrhythmic pulsations were detected.
ResultsA total of 8869 letters were sent. During the specified week, 1532 individuals were evaluated (877 women); the mean age was 72.5 (6.5) years old, 833 had hypertension (54%), 232 had diabetes (15%), 61 had previous stroke (4%) and 88 had had a myocardial infarction (6%). Electrocardiograms were performed in 187 patients. There were 17 patients with newly diagnosed atrial fibrillation.
ConclusionsA public, 5-day campaign based on pulse palpation and targeting elderly individuals had little impact on the detection of new cases of atrial fibrillation in our environment.
Keywords
Abbreviation
Atrial fibrillation (AF) is one of the main reasons for cardiology appointments and hospital admission and may also cause approximately one-fifth of acute cerebral infarctions. However, there is a substantial lack of awareness of this disease among the general population. Even though antithrombotic treatment may reduce embolic complications, there have been few campaigns for early diagnosis in Spain. It is estimated that AF is present in 0.5%-1.2% of the population, although that figure may be as high as 10% in those aged more than 70 years.1–5 In the PREV-ICTUS study,6 performed in Spain, the prevalence of AF according to chart review and examination of the electrocardiograms of 7108 individuals aged 60 years or more was 8.5% (4.2% aged 60-64 years and 16.5% aged more than 84 years).
AF increases the risk of stroke 5-fold. This relationship varies substantially with age and comorbid conditions. For example, between 50 and 59 years of age, AF may account for stroke in 1.5% of the cases, whereas between 70 and 79 years and between 80 and 89 years, that figure rises to 9.9% and 23.5%, respectively.7 In addition to the risk of embolism, several studies have shown that AF has a clear impact on cardiovascular morbidity and mortality.8–10 After intensive investigation with more than 60 000 participants in 33 randomized clinical trials, it was clearly established that anticoagulation therapy has a major impact on stroke in patients with AF, particularly in those aged more than 65 years and with a prior history of heart disease. Since many patients are asymptomatic, there is clear justification for systematic control of this arrhythmia, just as other risk factors such as blood pressure and dyslipidemia are monitored. Thus, the most recent guidelines for the primary prevention of stroke recommend active screening for AF in primary care for patients older than 65 years.11
We considered a program for education on and diagnosis of AF, aimed at persons over 65 years of age in 3 primary care clinics and a medical-surgical specialized clinic. The program consisted of 2 parts. The first was an educational program in which a leaflet was distributed to the target population attended in the health centers of Vigo (Pontevedra, Spain). Second, systematic screening was performed by palpation of the pulse of all volunteers aged 65 years or more who attended these clinics, as well as the medical-surgical specialized clinic of the referral hospital, in a given week. The objective of this second part was to obtain preliminary data for screening for new cases of AF among patients who might benefit from early treatment and primary prevention of cardiovascular disease.
MethodsStudy Design and ProceduresThe target population consisted of individuals≥65 years old, regardless of sex, the presence of other risk factors, or a history of cardiovascular disease. Patients with a history of AF or atrial flutter, as revealed by consultation of the computerized records, were excluded. Participants were mailed an information leaflet about AF and its potential harmful consequences for health (supplementary material), along with an invitation to attend a health center in a given week for palpation of the radial or humeral pulse by a trained nurse. During this week, the nurse was fully dedicated to this activity. During the visit, information was collected on vascular risk factors and prior symptoms. Blood pressure and heart rate were also recorded. The study activities were performed in 3 health centers in Vigo and the Morrazo Peninsula (Pontevedra, Spain), and the specialized center of the tertiary referral hospital. The information leaflet was distributed to patients and family members who were attending an appointment in the given week in this specialized center. Those aged over 65 years with no history of arrhythmia were invited to see the nurse in an office specially prepared for this activity. The specialized center is located in a separate building from the hospital and does not include cardiology appointments.
The study was approved by the Clinical Research Ethics Committee of Galicia (registry number 2011/065).
Training of Nursing StaffTwo nurses were assigned per center to participate directly in the project. The nurses had received prior training consisting of a 3-h course in which they listened to a presentation about AF (2h) and participated in a practical workshop on the methods for palpating the pulse and measuring blood pressure according to current clinical practice guidelines (1h).
Taking the PulsePrevious studies found a sensitivity in the range of 90%-95% for detecting AF by careful examination of the patient's pulse.12 According to these studies, the negative predictive value is close to 99%. The specificity is low, around 70%-75%, and consequently electrocardiographic confirmation is required. For the present study, it was recommended that the radial or humeral pulse was palpated for at least 20s. The rhythm was classified as: 1, normal; 2, at least 1 irregular beat; 3, more than 1 irregular beat, and 4, clearly irregular. Patients with pulse types 2, 3, or 4 according to this classification underwent 12-lead electrocardiography during the visit to the center.
After the training course, a validation study was performed in 26 patients admitted to the cardiology or internal medicine wards. Eleven of these patients had AF. The 11 nurses who participated in the activity were unaware of the patients’ baseline electrocardiographic rhythm. Immediately after palpating the pulse, the nurses filled out a form with the classification using 1 of the 4 categories. A complete electrocardiogram was then performed. Considering type 3 or 4 pulses as suspicious of AF, a sensitivity of 90.1% (4.9%) and a specificity of 82.4% (12.4%) were obtained, with a positive predictive value of 80.6% (12.5%) and a negative predictive value of 91.9% (4%). Based on these results, patients with pulse types 2-4 (any irregularity in the pulse) were selected to undergo electrocardiogram evaluation during “Pulse Week.”
Blood Pressure Reading and Medical HistoryAfter palpating the pulse, blood pressure was taken with an appropriately validated oscillometric device or by using a manual method if the pulse was markedly irregular. Assessment of blood pressure followed the guidelines published by the American Heart Association.13 During the visit, patients were questioned briefly to enable a short medical history to be taken.
Criteria for Referral to the PhysicianPatients with an arrhythmic pulse underwent an electrocardiogram which was interpreted in the presence of a family physician who participated in the activity. In the event that AF or atrial flutter was detected, the patient was sent to the referral cardiology department for the study. Patients with undiagnosed or uncontrolled hypertension received advice about maintaining a healthy lifestyle to reduce cardiovascular risk and were referred to their family physician.
Sample Size CalculationAccording to the estimates, the participating health centers attended 9435 individuals aged≥65 years old. The prevalence of AF determined by consultation of the databases was 6% of the patients and consequently the invitations to attend the center would not be applicable in 566 patients. In addition, in a standard working week, a total of 995 patients aged more than 65 years are attended in the specialized center of the referral hospital for our area. Therefore, the target population would consist of at least 9864 individuals. According to an arbitrary approximate estimate of a favorable response by 15% of those contacted, we calculated that with these postal invitations, we could obtain at least 1330 patients during the evaluation week in the health centers and a further 150 patients in the specialized center. A total number of 1580 participants would yield a precision of 0.45% in the event that the prevalence of undiagnosed AF was 1%, with a level of certainty (1 – α) of 95%.
Statistical AnalysisA common database was produced for all the participating centers for direct data collection during the appointment and for subsequent analysis. Numerical variables were expressed as means (standard deviations) and discontinuous variables as percentages. The differences between variables were calculated with Student t test and discontinuous variables with Fisher exact test. The SPSS statistical package, version 15.0, was used for the analysis.
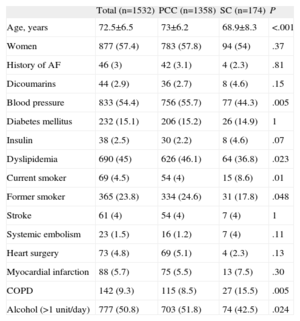
ResultsFor the 5 consecutive working days of “Pulse Week,” 1532 individuals were attended by the study nurses (heath center A, 591; health center B, 410; health center C, 357, and the specialized center, 174). The baseline characteristics of the population are summarized in Table 1. The subgroup of individuals included through the campaign of the specialized center had different characteristics, with a clearly lower mean age, lower prevalence of hypertension and dyslipidemia, a higher proportion of smokers, and a higher proportion of prior diagnosis of chronic obstructive pulmonary disease.
General Characteristics of the Population.
| Total (n=1532) | PCC (n=1358) | SC (n=174) | P | |
| Age, years | 72.5±6.5 | 73±6.2 | 68.9±8.3 | <.001 |
| Women | 877 (57.4) | 783 (57.8) | 94 (54) | .37 |
| History of AF | 46 (3) | 42 (3.1) | 4 (2.3) | .81 |
| Dicoumarins | 44 (2.9) | 36 (2.7) | 8 (4.6) | .15 |
| Blood pressure | 833 (54.4) | 756 (55.7) | 77 (44.3) | .005 |
| Diabetes mellitus | 232 (15.1) | 206 (15.2) | 26 (14.9) | 1 |
| Insulin | 38 (2.5) | 30 (2.2) | 8 (4.6) | .07 |
| Dyslipidemia | 690 (45) | 626 (46.1) | 64 (36.8) | .023 |
| Current smoker | 69 (4.5) | 54 (4) | 15 (8.6) | .01 |
| Former smoker | 365 (23.8) | 334 (24.6) | 31 (17.8) | .048 |
| Stroke | 61 (4) | 54 (4) | 7 (4) | 1 |
| Systemic embolism | 23 (1.5) | 16 (1.2) | 7 (4) | .11 |
| Heart surgery | 73 (4.8) | 69 (5.1) | 4 (2.3) | .13 |
| Myocardial infarction | 88 (5.7) | 75 (5.5) | 13 (7.5) | .30 |
| COPD | 142 (9.3) | 115 (8.5) | 27 (15.5) | .005 |
| Alcohol (>1 unit/day) | 777 (50.8) | 703 (51.8) | 74 (42.5) | .024 |
AF, atrial fibrillation; COPD, chronic obstructive pulmonary disease; PCC, primary care center; SC, specialized center.
Data are expressed as mean±standard deviation or no. (%).
Some patients had a history of AF despite the prior filter of the invitations (n=46). These patients were explained the nature of the campaign in detail and were invited to return to the center according to their usual follow-up schedule. However, some of the patients with previously diagnosed AF did not disclose this condition during the nursing visit and they were only identified and reclassified in the database after seeing the physician and after the electrocardiogram was performed (n=14).
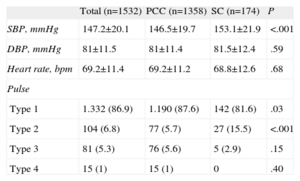
Blood Pressure and Pulse ClassificationThe blood pressure data and pulse analysis are shown in Table 2. A blood pressure above 140/90mmHg was found in 953 patients (62.2%). Of the 922 patients with systolic blood pressure>140mg, 369 (40%) did not have a prior diagnosis of hypertension.
Data From the Appointment With the Nurse.
| Total (n=1532) | PCC (n=1358) | SC (n=174) | P | |
| SBP, mmHg | 147.2±20.1 | 146.5±19.7 | 153.1±21.9 | <.001 |
| DBP, mmHg | 81±11.5 | 81±11.4 | 81.5±12.4 | .59 |
| Heart rate, bpm | 69.2±11.4 | 69.2±11.2 | 68.8±12.6 | .68 |
| Pulse | ||||
| Type 1 | 1.332 (86.9) | 1.190 (87.6) | 142 (81.6) | .03 |
| Type 2 | 104 (6.8) | 77 (5.7) | 27 (15.5) | <.001 |
| Type 3 | 81 (5.3) | 76 (5.6) | 5 (2.9) | .15 |
| Type 4 | 15 (1) | 15 (1) | 0 | .40 |
DBP, diastolic blood pressure; PCC, primary care center; SBP, systolic blood pressure; SC, specialized center.
Type of pulse: 1, normal; 2, at least one irregular beat; 3, more than 1 irregular beat; 4, clearly irregular.
Data are expressed as mean±standard deviation or no. (%).
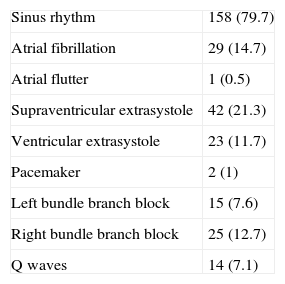
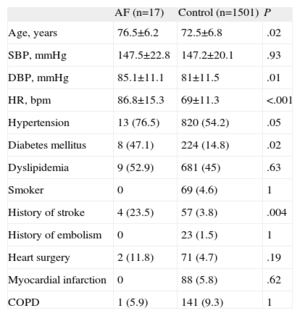
According to the protocol for pulse analysis, 197 electrocardiograms were performed (Table 3). Of the electrocardiograms, 165 were performed in primary health care clinics and 32 in the specialized clinic (12% and 18% of the individuals who visited these centers, respectively; P=.03). Only 1 patient did not agree to undergo an electrocardiogram in 1 of the health centers. AF or atrial flutter was detected in 30 (15%) of the traces (28 in primary health care clinics and 2 in the specialized center; P=.57), but only 17 (1.1%; 95% confidence interval, 0.7%-1.8%) were considered new cases of arrhythmia after chart review. Of the patients newly diagnosed with AF, 15 were detected in primary health care clinics (1.1%) and 2 in specialized center (1.1%); P=1. Of these patients, 1 had paroxysmal AF, only detected in the trace during the campaign, and sinus rhythm in an individual appointment. The remaining 16 patients were classified as having permanent AF. Patients in AF had a higher mean age, greater heart rate during the appointment, and a greater prevalence of hypertension and diabetes mellitus (Table 4). Notably, 4 of the 17 patients (23.5%) had a history of stroke compared with 57 of the remaining 1501 patients without AF (3.8%; P=.004).
Electrocardiographic Findings (n=197).
| Sinus rhythm | 158 (79.7) |
| Atrial fibrillation | 29 (14.7) |
| Atrial flutter | 1 (0.5) |
| Supraventricular extrasystole | 42 (21.3) |
| Ventricular extrasystole | 23 (11.7) |
| Pacemaker | 2 (1) |
| Left bundle branch block | 15 (7.6) |
| Right bundle branch block | 25 (12.7) |
| Q waves | 14 (7.1) |
Data are presented as no. (%).
Comparison Between the Patients With Newly Diagnosed Atrial Fibrillation and the Remaining Population.
| AF (n=17) | Control (n=1501) | P | |
| Age, years | 76.5±6.2 | 72.5±6.8 | .02 |
| SBP, mmHg | 147.5±22.8 | 147.2±20.1 | .93 |
| DBP, mmHg | 85.1±11.1 | 81±11.5 | .01 |
| HR, bpm | 86.8±15.3 | 69±11.3 | <.001 |
| Hypertension | 13 (76.5) | 820 (54.2) | .05 |
| Diabetes mellitus | 8 (47.1) | 224 (14.8) | .02 |
| Dyslipidemia | 9 (52.9) | 681 (45) | .63 |
| Smoker | 0 | 69 (4.6) | 1 |
| History of stroke | 4 (23.5) | 57 (3.8) | .004 |
| History of embolism | 0 | 23 (1.5) | 1 |
| Heart surgery | 2 (11.8) | 71 (4.7) | .19 |
| Myocardial infarction | 0 | 88 (5.8) | .62 |
| COPD | 1 (5.9) | 141 (9.3) | 1 |
AF, atrial fibrillation; COPD, chronic obstructive pulmonary disease; DBP, diastolic blood pressure; HR, heart rate; SBP, systolic blood pressure.
Data are expressed as mean±standard deviation or no. (%).
After the “Pulse Week” campaign, the number of appointments for AF in the referral cardiology department increased. Thus, 45 patients (5.6% of the 810 visits) were attended with AF as the chief complaint in the preceding 3 months whereas 51 patients were seen in the 3 months after the campaign (8.6% of a total of 595 visits; P=.03). This increase in the number of visits for AF was in line with the number of new cases diagnosed. There were no significant differences in the other reasons for the visit, such as palpitations (8.4% vs 8.7%; P=.89), an abnormal electrocardiogram (12.5% vs 12.5%; P=.99), dyspnea (12% vs 10.1%; P=.3), or chest pain (13% vs 11.3%; P=.38).
DiscussionThe present study describes the results of a campaign designed to detect newly diagnosed AF in an elderly population and to increase the awareness of the general public and nursing staff of the consequences of this arrhythmia for cardiovascular health. By means of pulse palpation by nurses, only 17 new cases of AF were detected among more than 1500 patients examined.
The usual strategies employed in our clinical practice for the detection of AF include assessment of patients with indicative symptoms such as dyspnea, palpitations or dizziness, or an opportunistic case finding of arrhythmia. However, many patients are asymptomatic and do not attend their physician for assessment. Asymptomatic patients or those with paroxysmal episodes of AF have the same thromboembolic risk and may not be represented in the published series.
Some studies have compared a systematic screening strategy for AF with other forms of case finding.14–16 Two randomized studies produced not too different results. A study by Morgan et al.15 published in 2002 compared the effectiveness of 2 techniques: pulse palpation by a nurse after en mass distribution of an invitation and opportunistic screening. A total of 3001 patients aged 65-100 years were included. Many more patients in the arm randomized to invitation by letter and assessment by nurses were examined, and 3.5 times more cases of AF were detected in this subgroup. Nevertheless, most of the patients diagnosed by the nurses already had a history of AF. In 2007, Fitzmaurice et al.16 randomized patients to systematic screening, opportunistic screening, and no specific strategy in a population of more than 16 000 subjects in the United Kingdom. Detection of new cases of AF was similar in the groups systematically analyzed after invitation (1.62%/year) and the arm with opportunistic screening (1.64%/year).
The findings of our study, with only 1.1% of new cases diagnosed despite assessment of more than 1500 patients, and the experience in clinical practice in the United Kingdom indicate that opportunistic screening for arrhythmias is more efficient for detecting new cases of AF. However, the “Pulse Week” campaign may be beneficial in ways that are difficult to quantify. For example, the population may be better informed, thereby helping to improve therapeutic adherence and facilitating the detection of new cases if, after the campaign, suggestive symptoms occurred. Indeed, our impression was that after the week in question, more patients attended primary care appointments for assessment of cardiac rhythm. Such an effect could be considered negative if there were more appointments, but this was not the case. In addition, the experience of coordination among nurses, family physicians, and cardiologists led to more favorable outcomes beyond the results of new diagnosis of AF. Another positive effect of the “Pulse Week” was that a considerable number of patients who had uncontrolled blood pressure despite prior treatment were detected and referred.
LimitationsThis study does not allow the prevalence of AF to be estimated in our population. The sample may have been biased in that patients with greatest risk of AF attended the appointment because they had symptoms or prior cerebrovascular accidents. Nevertheless, one of the objectives was to inform our patients of the implications of an arrhythmia as frequent as AF and to try to increase the practice of an examination as simple and safe as pulse palpation among nurses.
Taking the pulse is not a specific method for detecting AF and certainly not for detecting atrial flutter. However, the sensitivity recorded in our series was close to 90% and was similar to that reported by other studies. Systematic performance of electrocardiograms in the entire population invited for appointments would be impractical in a single campaign week. The inclusion of patients with any irregularity in the pulse probably helped limit the number of false negatives in our study. Another limitation is that AF is often transient and therefore it might not be present at the time of the examination or during the electrocardiogram. Patients with intermittent symptoms and suspicion of paroxysmal AF should be referred for further studies, such as with a Holter device or an event recorder.
ConclusionsAfter inviting almost 1500 elderly individuals by letter for an appointment with a nurse, relatively few undocumented cases of AF were diagnosed. The results of this campaign for education on and diagnosis of AF indicate that opportunistic screening is the best strategy in our practice for the early detection of this arrhythmia.
Conflicts of interestNone declared.
We are particularly grateful to the Povisa Nursing School for their invaluable collaboration in this campaign.
This initiative received a prize within the campaign “1 Mission 1 Million,” funded by Boehringer Ingelheim.