Blood pressure measurement methods and conditions are determinants of hypertension diagnosis. A recent British guideline recommends systematic 24-h ambulatory blood pressure monitoring. However, these devices are not available at all health centers and they can only be used by 1 patient per day. The aim of this study was to test a new blood pressure recording method to see if it gave the same diagnostic results as 24-h blood pressure monitoring.
MethodsOne-hour blood pressure monitoring under routine clinical practice conditions was compared with standard method of day time recording by analyzing the coefficient of correlation and Bland-Altman plots. The Kappa index was used to calculate degree of agreement. Method sensitivity and specificity were also analyzed.
ResultsOf the 102 participants, 89 (87.3%) obtained the same diagnosis regardless of method, with high between-method agreement (κ= 0.81; 95% confidence interval, 0.71-0.91). We observed robust correlations between diastolic (r=0.85) and systolic blood pressure (r=0.76) readings. Sensitivity and specificity for the new method for diagnosing white coat hypertension were 85.2% (95% confidence interval 67.5%-94.1%) and 92% (95% confidence interval, 83.6%-96.3%), respectively.
ConclusionsOne-hour blood pressure monitoring is a valid and reliable method for diagnosing hypertension and for classifying hypertension subpopulations, especially in white coat hypertension and refractory hypertension. This also leads to a more productive use of monitoring instruments.
Keywords
Hypertension (HT), smoking, and hypercholesterolemia are the three most common cardiovascular risk factors in Spain. Prevalence of HT in adults > 18 years is about 38% in men and 28% in women, and these figures increase as the population ages.1,2 From a macroeconomic point of view, direct health costs associated with HT account for 2.6% to 3.9% of total health expenditure in Spain.3 The consequences of such high prevalence are seen at primary care clinics, where HT is one of the leading reasons for consultation.3
Hypertension can be diagnosed by various methods, which vary according to how often blood pressure (BP) is measured. The PAPPS4 recommends measuring BP at 3 office visits at least a week apart, and this is standard practice worldwide. However, this method has significant limitations because it does not reflect BP fluctuations during the day, does not rule out white coat hypertension (WCH), and is of limited value as a cardiovascular risk predictor.5,6
The recently published NICE guidelines7 in the United Kingdom and the European Society of Hypertension/European Society of Cardiology Guidelines for the management of HT8,9 recommend 24-h electronic ambulatory blood pressure monitoring (ABPM) or, if this is not available, self-measured home blood pressure monitoring (HBPM) as valid methods for HT diagnosis and management. The advantage of HBPM is that patients record their own BP, thus avoiding factors associated with sudden fluctuations in BP. However, the validity of this method is compromised by BP variability itself, the reliability of the technique used, and the wide variety of calibration standards found in these devices.10–14 The advantages of ABPM include the possibility of analyzing circadian BP variability15–18 and it provides information on the BP pattern of nighttime dipping and morning elevations, which are associated with cerebrovascular disease.19–21 Using ABPM, patients can be categorized into normal, WCH, masked hypertension, and refractory hypertension (RH) subgroups. The prevalence of WCH is about 15%18 among grade I hypertensive patients, and in fact white coat effect is one of the main indications for ABPM. Despite these advantages, systematic implementation of ABPM in primary health care is limited because it can only be used by one patient per day. In addition, validated devices are expensive.
Studies investigating other ways of obtaining measurements similar to ABPM have produced mixed results.22–24 For this reason, the aim of this study was to validate a new method using 1-h blood pressure monitoring (1BPM) with a single ABPM device and to assess its efficacy in HT diagnosis and follow-up in hypertensive patient subgroups.
METHODSDesignA validation study for a new method (1BPM) to measure, record, and determine HT, comparing it with daytime recordings taken with the reference method (ABPM).
Study PopulationParticipants were recruited from a population of patients seen at an urban health center. Inclusion criteria were age > 18 years and indication for ABPM under real clinical practice conditions in one of three clinical situations: newly diagnosed HT, suspected WCH, and HT monitoring due to suspected masked HT or RH. We used the same exclusion criteria as recommended in the NICE7 and European8,9 guidelines (ie, atrial fibrillation or other heart rhythm disorders that could interfere with readings), and lack of cooperation as an additional exclusion criterion. Following the indications in the Catalonian “Practical Guide for Hypertension in Primary Care”25, we defined a valid 1BPM result as at least 70% correct readings. After completing both tests, participants were excluded if the percentages of correct 1BPM and ABPM readings were <70%.25,26
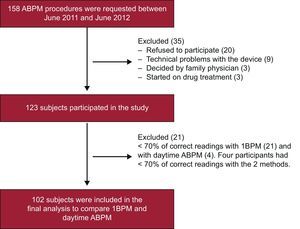
Participants were recruited between June 2011 and June 2012.
ProcedureWe used the same device (Spacelabs® 90207)27 for BP measuring and recording in both methods (1BPM and ABPM). This device has a standard cuff that is adjusted to fit the participant's arm and is inflated at programmable intervals. It also has a portable unit that records and stores the data.
For the ABPM method, we programmed the device to record the participant's BP every 20 min and 30min during the day and night, respectively.28 Participants were advised to carry on with their normal daily activities, avoiding any intense physical exertion, and to remain at rest when their BP was being measured. We compared 1BPM with the daytime ABPM values (taken between 8:00 am and 8:00 pm). The 1BPM method was performed 24 h to 48h after the ABPM recording. We checked that there had been no changes in the participant's baseline conditions during this period. For the 1BPM, measurements were programmed at 6-min intervals over 1 h. Two extra recordings taken at the start and end of this period were discarded. All 1BPM procedures were performed at morning appointments, between 9 am and 1 pm. Patients were given information about the study, they were told about the procedure at their family physician's office, and BP was measured in a quiet room at the same health center.
Study VariablesThe primary endpoint was patient classification by HT subpopulation with the following groups: normal (office BP <140/90mmHg and ABPM or 1BPM<135/85mmHg); WCH (office BP ≥ 140/90mmHg and ABPM or 1BPM<135/85mmHg); masked hypertension (office BP<140/90mmHg and ABPM or 1BPM ≥ 135/85mmHg), and RH (office BP ≥ 140/90mmHg and ABPM or 1BPM ≥ 135/85mmHg). If an office BP recording was not available, the mean of the 3 most recent patient-reported HBPM recordings was used. There were 19 such cases.
The following sociodemographic variables were taken from the patient's medical record: age, sex, weight, height, body mass index, history of cardiovascular risk factors, smoking status, alcohol consumption, sedentary lifestyle, diabetes mellitus, dyslipidemia, and obesity.
Sample SizeAssuming that about 90%22 of patients would be correctly classified with 1BPM compared with ABPM in terms of HT subpopulation, with a 5% precision, 90% confidence level, and 20% loss rate, we estimated that a minimum sample size of 98 participants would be needed for the study.
Ethical AspectsThis study was approved by the Ethics Committee for Clinical Research at Hospital Clínic, under registration no. 2011/6743. Patients who agreed to participate were duly informed and provided their signature on the informed consent form. Study procedures were in compliance with all the clauses in the Declaration of Helsinki regarding the conduct of biomedical research and respect for human rights.
Statistical AnalysisCategorical variables were expressed as an absolute frequency (%). Continuous variables were described as mean (standard deviation) or median [interquartile range]. We used the Shapiro-Wilk normality test to check for normal variable distribution.
We used the Pearson's r to calculate the coefficient of correlation between 1BPM and ABPM, and the Bland-Altman method29 to plot range correlations (differences between the measurements against the mean) to confirm independence of the differences obtained with each method and the magnitude.
We calculated the prevalence of WCH, masked hypertension, and RH. The percentage of participants correctly classified with 1BPM according to ABPM results was estimated, and the Kappa index30 was used to measure the degree of agreement between the two methods when classifying participants by HT subpopulation. We calculated the sensitivity, specificity, and positive and negative predictive values for the diagnoses of WCH, RH, and masked hypertension. All agreement and correlation parameters were based on the mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) readings for each patient.
We performed a sensitivity analysis to compare the baseline characteristics of included and excluded patients in the final analysis (< 70% correct readings with 1BPM and ABPM.) Statistical significance was defined as P<0.05. We calculated 95% confidence intervals (95%CI). The statistical analysis was performed using the R statistics program version 2.15.1 for Windows.31
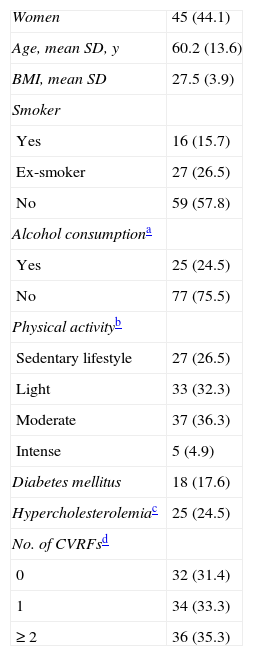
RESULTSParticipant CharacteristicsA total of 158 ABPM procedures were requested, 123 (77.8%) of which were included in the study. Figure 1 shows the participant inclusion flowchart, with reasons for exclusion. Of the 102 patients in the final analysis, 45 (44.1%) were women, the mean age was 60.2 years (13.6) years, and body mass index was 27.5 (3.9). Table 1 shows patients’ baseline characteristics at inclusion. Indications for ABPM were distributed as follows: 49 (48.0%), HT diagnosis; 36 (35.3%), HT follow-up; 12 (11.8%), suspected WCH; and 5 (4.9%), other reasons. The sensitivity analysis did not reveal statistically significant differences between included and excluded patients in the final analysis in terms of baseline characteristics.
Baseline Characteristics of the 102 Study Subjects
| Women | 45 (44.1) |
| Age, mean SD, y | 60.2 (13.6) |
| BMI, mean SD | 27.5 (3.9) |
| Smoker | |
| Yes | 16 (15.7) |
| Ex-smoker | 27 (26.5) |
| No | 59 (57.8) |
| Alcohol consumptiona | |
| Yes | 25 (24.5) |
| No | 77 (75.5) |
| Physical activityb | |
| Sedentary lifestyle | 27 (26.5) |
| Light | 33 (32.3) |
| Moderate | 37 (36.3) |
| Intense | 5 (4.9) |
| Diabetes mellitus | 18 (17.6) |
| Hypercholesterolemiac | 25 (24.5) |
| No. of CVRFsd | |
| 0 | 32 (31.4) |
| 1 | 34 (33.3) |
| ≥ 2 | 36 (35.3) |
BMI, body mass index; CVRF, cardiovascular risk factor; SD, standard deviation.
Data are expressed as No. (%) or mean (standard deviation).
Question on weekly alcohol intake (Systematic Interview of Alcohol Consumption); yes, >1 weekly drink; no, no weekly drink.
Intense: lifting heavy objects, digging, aerobics, or fast bicycling; moderate: carrying light loads, bicycling at a regular pace, or playing tennis doubles; light: housework, walking to get from one place to another or any other walking solely for recreation, sport, exercise or pleasure; sedentary lifestyle: regular physical activity does not involve activities from the other categories, time sitting at work, at home, studying, and at leisure.
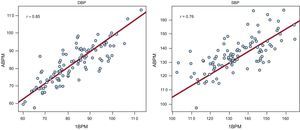
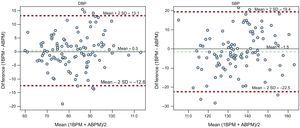
The ten 6-min-interval readings recorded for DBP and SBP using 1BPM had a homogenous distribution (Figure 2). We verified a normal distribution of the mean readings for DBP and SBP for both 1BPM and ABPM. High correlation was observed between DBP (r=0.85) and SBP (r=0.76) using daytime ABPM and 1BPM (Figure 3). However, correlations were lower when comparing nighttime ABPM (DBP [r = 0.72] y SBP [r = 0.50]) with 1BPM. The differences between 1BPM and ABPM were independent of the DBP mean figure (r=0.125; P=.213), and there was a weak but statistically significant correlation in the case of the SBP (r=0.253; P=.010). Overall, 93.1% and 95.1% of the values fell within the confidence interval for DBP and SBP, respectively. The DBP and SBP confidence interval ranges (±12mmHg and ±20mmHg, respectively) were acceptable, and therefore we can confirm that the results are clinically relevant (Figure 4).
Distribution of diastolic blood pressure and systolic blood pressure readings using 1-h blood pressure monitoring. The dashed green lines show the normal cut-offs for the test (diastolic blood pressure, 85mmHg; systolic blood pressure, 135mmHg). The initial reading (I) was taken when the device was put in position and the final reading (F) was taken when it was removed (pre- and post-test). DBP, diastolic blood pressure; SBP, systolic blood pressure.
Diastolic blood pressure and systolic blood pressure comparison of 1-h blood pressure monitoring and ambulatory blood pressure monitoring. The points represent the mean diastolic blood pressure (or systolic blood pressure) recorded by 1-h blood pressure monitoring (horizontal axis) and by ambulatory blood pressure monitoring (vertical axis). The red lines show the correlations between these values, and r shows the coefficient of correlation. ABPM, ambulatory blood pressure monitoring; 1BPM, 1-h blood pressure monitoring; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Bland-Altman plots; the horizontal axis shows the mean determinations using the 2 methods and the vertical axis shows the difference between the methods. The dashed green lines show the mean differences and the dashed red lines show their confidence intervals. ABPM, ambulatory blood pressure monitoring; 1BPM, 1-h blood pressure monitoring; DBP, diastolic blood pressure; SBP, systolic blood pressure; SD, standard deviation.
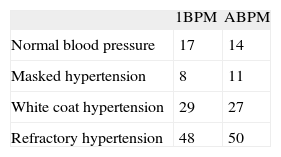
With regard to hypertension subpopulation classification, 89 (87.3%) of the 102 participants received the same classification using daytime ABPM and 1BPM (Table 2). There was high agreement between the two methods: κ=0.81 (95%CI, 0.71-0.91).
Comparison of Daytime Ambulatory Blood Pressure Monitoring and 1-h Blood Pressure Monitoring in Hypertension Subpopulation Classification
| 1BPM | ABPM | |
| Normal blood pressure | 17 | 14 |
| Masked hypertension | 8 | 11 |
| White coat hypertension | 29 | 27 |
| Refractory hypertension | 48 | 50 |
ABPM, ambulatory blood pressure monitoring; 1BPM, 1-h blood pressure monitoring.
A total of 89 participants (14 with normal blood pressure, 8 with masked hypertension, 23 with white coat hypertension, 44 with refractory hypertension) were classified in the same subgroup using daytime ambulatory blood pressure monitoring and 1-h blood pressure monitoring.
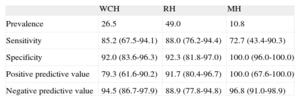
The WCH prevalence was 26.5% with ABPM. Results showed 85.2% (95%CI, 67.5%-94.1%) sensitivity and 92% (95%CI, 83.6%-96.3%) specificity when 1BPM was used to diagnose WCH. We observed an even higher prevalence of RH (49%) using ABPM, with 88% (95%CI, 76.2%-94.4%) sensitivity and 92.3% (95%CI, 81.8%-97.0%) specificity when 1BPM was used to diagnose RH. Masked hypertension had the lowest prevalence (10.8%), with 1BPM sensitivity and specificity of 72.7% (95%CI, 43.4%-90.3%) and 100.0% (95%CI, 96.0%-100.0%), respectively (Table 3).
Prevalence, Sensitivity, Specificity, Positive Predictive Value, Negative Predictive Value, and the Corresponding 95% Confidence Intervals in the Diagnosis of White Coat Hypertension, Refractory Hypertension, and Masked Hypertension
| WCH | RH | MH | |
| Prevalence | 26.5 | 49.0 | 10.8 |
| Sensitivity | 85.2 (67.5-94.1) | 88.0 (76.2-94.4) | 72.7 (43.4-90.3) |
| Specificity | 92.0 (83.6-96.3) | 92.3 (81.8-97.0) | 100.0 (96.0-100.0) |
| Positive predictive value | 79.3 (61.6-90.2) | 91.7 (80.4-96.7) | 100.0 (67.6-100.0) |
| Negative predictive value | 94.5 (86.7-97.9) | 88.9 (77.8-94.8) | 96.8 (91.0-98.9) |
WCH, white coat hypertension; MH, masked hypertension; RH, refractory hypertension.
In 87.3% of cases, the 1BPM method results in the same classification as 24-h ABPM. In addition, 1BPM shows high correlations with ABPM for both SBP (r=0.76) and DBP (r=0.85), and high sensitivity and specificity for diagnosing WCH and RH.
The simplicity and reproducibility of this new recording method will optimize the use of ABPM in primary care. In the search for new BP measuring methods to simplify ABPM, a recent study conducted in The Netherlands22 recorded BP every 5min for a total 30min in 84 subjects, and compared results with 24-h ABPM. This method classified 87% of subjects in the same way as the reference method, and these results are almost identical to those observed in our study. It seems clear that BP measurements recorded with simplified methods closely match the results of daytime ABPM. However, because there is some variability, there is limited consensus on the minimum BP recording period that will provide sufficient agreement with daytime ABPM. Wong and Yeo32 studied subjects with sleep disturbance and nighttime BP dipping, but with longer recording periods. They compared 24-h daytime ABPM recordings vs office-hour BP monitoring (from 8:00 am to 6:00 pm), and drew the same conclusions regarding agreement. Sheps et al33 compared 6-hour BP recording with 2 or 3 BP recordings per hour in healthy volunteers and patients with mild-moderate HT. Again, there were positive results with regard to agreement. However, a 6-h method may be too lengthy for implementation in real clinical practice conditions in primary care.
A systematic review of 16 clinical trials compared the performance of HBPM with different oscillometric devices and ABPM.11 There was moderate agreement in terms of diagnosis of WCH, RH, and masked hypertension. However, the same authors conducted a study called MEDIT-HABP with 1441 patients and found 86% diagnostic agreement between ABPM and HBPM for WCH.34 Many different BP measuring devices and methods have been tested. One of the most commonly-used devices is the automated oscillometric BpTRU (with a protocol involving 5 readings over 25min at 5-min intervals). However, this method has produced contradictory results. Culleton et al23 used it in a trial with 107 participants and found only 48% agreement with ABPM. In contrast, García-Donaire et al24 achieved better results in a comparison with office BP readings (3 taken at 3-min intervals), with some changes to the BpTRU protocol (using the arithmetic mean of 5 readings taken at 2-min intervals).
In addition, the use of an automated device reduced the white-coat effect that occurs in an office setting. As in the MEDIT-HABP study, Myers et al35 found that measuring BP in an office when the patient is alone reduces the white coat effect from 55% with routine BP recording to 16% with a 20-min BP recording. They also reported good correlation between ABPM and the 20-v recording. Many studies have compared ABPM with office BP readings when analyzing WCH. Recently, De la Sierra et al36, in a study with 68 045 hypertensive patients (8295 of whom had RH), reported that more than a third of participants initially classified as having RH actually had WCH or isolated RH with normal ABPM values. A more affordable method, such as 1BPM, could be used in this case to prevent overdiagnosis (or misdiagnosis) of RH.
The European Society of Hypertension8,9 acknowledges that HBPM can provide information that is as reliable as single office BP recordings for predicting cardiovascular morbidity and mortality. It proposes a number of very specific, methodological aspects that are necessary for the diagnostic evaluation of HT using HBPM: BP should be measured on an indeterminate number of occasions for at least 7 consecutive days, in the mornings as well as in the evenings. Although the guideline acknowledges that HBPM is as reliable as office BP recordings, it also notes that patient-reported values may not always be reliable, do not reflect very short-term BP variability, and may not reflect a patient's real routine.
Currently all large multinational clinical trials on HT screen patients with a diagnosis criterion based on the triple office BP recording. However, there is also an intense, on-going debate in routine clinical practice about which patients are true hypertensives, and what is the best diagnostic and monitoring method. A dynamic relationship has recently been found between mortality and BP values. This means that the traditional SBP reference value of 140mmHg may not be suitable for diagnostic purposes or as a therapeutic target.37 Recording methods such as 1BPM could support the decisions of the clinicians who embrace such methods and also convince patients who are labeled as hypertensive and will probably be medicated for life. Until clinical trials require ABPM, HBPM, or 1BPM as an inclusion criterion, it will be hard to quantify their influence on cardiovascular morbidity and mortality.
LimitationsDespite its good results, 1BPM has some limitations. The most obvious limitation is that 1BPM does not provide nighttime BP data, which is relevant in a global assessment of cardiovascular risk. The moderate level of correlation observed between 1BPM and nighttime ABPM shows that 1BPM cannot substitute 24-h ABPM for describing nighttime BP patterns, which is one of its possible applications. Our study was conducted at a single health center, and with a relatively small population sample. In addition, 1BPM is performed over 1 h at 6-min intervals, so if one of the readings is not recorded correctly, there is only a very small window for repeating it. Finally, for logistic and organizational reasons at our health center, we were not able to randomize the order of the tests, which would have prevented any potential order effect on the degree of agreement. It is difficult to extrapolate to what extent the 1BPM limitations are relevant in the prognostic assessment of risk and whether there is repercussion in target organ damage, compared to 24-h ABPM. However, the results of our study confirm that 1BPM may be a valid and effective diagnostic alternative that is acceptable for patients and easily implemented in HT studies, which would lead to a more generalized, efficient, and productive use of ABPM devices.
CONCLUSIONSOne-hour blood pressure monitoring shows high sensitivity and specificity in WCH and RH diagnosis. This new method has shown to be as useful as 24-h ABPM in the diagnosis and follow-up of different HT subpopulations. Its applicability in real clinical practice gives it the potential to make 1BPM the diagnostic gold standard at all levels of health care.
FUNDINGThis study was funded through a 2011 Beca Fin de Residencia (End of Residency Grant) provided by Consorci d’Atenció Primària de Salut de l’Eixample.
CONFLICTS OF INTERESTNone declared.
We are grateful to the study participants (patients at Primary Care Center Les Corts) for their cooperation, and to the entire Primary Care Team of Les Corts (Barcelona), and especially the nursing staff, who performed the BP monitoring.