Cardiovascular disease is the leading cause of death in the world, affecting not only industrialized but, above all, low- and middle-income countries, where it has overtaken infectious diseases as the first cause of death and its impact threatens social and economic development. The increased prevalence of cardiovascular disease in recent years together with projected mortality for the coming decades constitute an irrefutable argument for the urgent implementation of well-planned interventions to control the pandemic of cardiovascular diseases, especially in the more economically deprived countries. The combination of behavioral, social, environmental, and biological factors, and others related to health care systems, that contribute to the development of cardiovascular diseases requires a multi-sector strategy that promotes a healthy lifestyle, reduces cardiovascular risk factors, and cuts mortality and morbidity through quality health care services. These proposals should be guided by leaders in the scientific community, government, civil society, private sector, and local communities.
Keywords
The world population continues to grow at an unstoppable rate. Simultaneously, the population is aging and we are witnessing an alarming increase in specific cardiovascular risk factors (CVRF), like bad nutrition habits and obesity, with an unquestionable impact on the state of health of the population at large. And so we find ourselves facing a cardiovascular disease (CVD) pandemic that has complex multi-factor causes in which different sectors of society are implicated. Cardiovascular health promotion should extend throughout the life of the individual from infancy, when heart–healthy habits are acquired, to old age. In Revista Española de Cardiología, the present “Focus on” article presents new data obtained from scientific studies capable of making an impact on population-wide cardiovascular health.
In the last 20 years, CVD—eminently in response to the increased prevalence of less–than–healthy lifestyles—has expanded worldwide in parallel with the phenomenon of globalization, practically becoming endemic in the industrialized countries and significantly attacking less well-off countries, to become the leading cause of death in the world.1,2 The effect of CVD is especially cruel in low–middle income countries where mortality and morbidity are making such an impact that the social and economic development of several of these countries is actually under threat. Not only has the global CVD problem grown substantially, but action is urgently needed because recognizing the extent of CVD worldwide has always lagged behind the pandemic itself. In the 1980s, the World Health Organization (WHO) denounced the alarming increase in the rate of ischemic heart disease in developing countries.3 In 2004, Leeder et al4 predicted the devastating impact of CVD, especially in the working population (aged between 35 and 64 years) of low–middle income countries in 2030. In 2007, Fuster et al5 warned of the lack of attention that the scientific and political community gave to noncommunicable diseases (NCD) despite the fact that, as early as 2001, CVD had become the leading cause of death in the world—particularly in developing countries, where the growth of the disease was already alarming.
In response to the global increase in CVD, the US Institute of Medicine constituted a committee of experts whose objective was to prepare a document analyzing strategies to counter the CVD tsunami that was beginning to devastate the developing countries. The report, entitled “Promoting Cardiovascular Health in the Developing World”, was published in 2010 and presents 12 recommendations to reduce the global burden of CVD, with an emphasis on developing guidelines for collaboration between public and private entities committed to development and world health.6
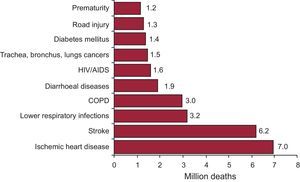
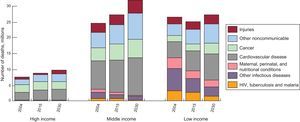
The April 2011 WHO report on the global status of NCD7 showed that these have become the leading cause of death in the world, responsible for 64% of deaths in 2011. The data leave no room for doubt: more than 36 million people died of NCD in 2011, principally due to CVD (ischemic heart disease and cerebrovascular disease), cancer, chronic respiratory diseases and diabetes mellitus (Figure 1). More than 9 million of these deaths occurred in patients<60 years of age and were, in the main, avoidable. Moreover, the report highlighted the fact that most deaths due to NCD (> 80%) occurred in low–middle income countries. In fact, various studies predict that these are the countries where CVD incidence is increasing most9 (Figure 2). The WHO report broke new ground as it provided a cross-sectional view of the CVD situation worldwide, calculating the impact on health and on social and economic development, especially in low- and middle-income countries. Similarly, it offered a structure to monitor NCD, associated risk factors, outcomes (morbidity and mortality), and the response capability of different health systems faced with this pandemic.
Principle causes of death in the world in 2011. COPD, chronic obstructive pulmonar disease; HIV, human infectious virus. Adapted from the World Health Organization.8
Projected deaths by cause, 2004, 2015, 2030. Countries are categorized according to World Bank guidelines, by gross national income per capita: low income (≤ 825 dollars), middle income (826-10 065 dollars) and high income (≥ 10 066 dollars). HIV: human immunodeficiency virus. Data adapted from World Health Organization.
Given the reality of the WHO data, this time the international community responded vigorously. Throughout its history, the United Nations has called 2 urgent, high-level meetings of the General Assembly on public health issues. The first, in 2001, assessed the effects and strategies to mitigate the human immunodeficiency virus and acquired immunodeficiency syndrome pandemic. The second, because of the WHO report data, in September 2011, centered on the global impact of NCD. The United Nations meeting presented evidence of the positive effects from interventions to reduce mortality due to NCD and of the viability and economic benefit of these interventions, even in the poorest countries.
GLOBAL DIMENSION OF CARDIOVASCULAR DISEASE: IMPACT ON HEALTH CARE AND THE ECONOMYThe health of the world population is at serious risk, given the universal presence of CVRF. The consumer society we live in does not encourage healthy living and the consequences of this are even more devastating if we bear in mind the social inequalities, economic context, and demographic explosion of the last 20 or more years. The growth of bad nutrition habits, obesity, and high blood pressure increasingly contributes to the expanding CVD epidemic. The factors influencing this deterioration of our health can be grouped into several categories. There are genetic risk factors and biological risk factors (high blood pressure, dyslipidemia, diabetes mellitus), the negative influence of which is modulated by behavioral factors (diet, physical activity, smoking); these, in turn, depend on structural factors (the changing demographic characteristics of the society we live in, economic development, the sociopolitical context, education, culture, and globalization). The pathologic expression of these risk factors takes the form of atherosclerotic and hypertensive diseases, mainly ischemic heart disease and cerebrovascular disease. It is estimated that in 2020 these two diseases will be the first and second causes of death, the first and third causes of lost life years, and the first and fourth causes of disability-adjusted life years.10–12 These risk factors not only induce CVD, but share a causal relationship with the remaining NCD (cancer, diabetes mellitus, and chronic obstructive pulmonary disease).13
In 1990, there were 26.6 million deaths due to NCD (57.2% of a total 46.5 million deaths), which in 2010 increased to 34.5 million (65.5% of 52.8 million deaths), converting it into the first cause of death everywhere on the planet—except Sub-Saharan Africa and southern Asia.14 The mortality projections are spine-chilling: the estimate is 56 million deaths in 2030.15 With respect to morbidity, the global burden of NCD has increased from 43% of total disability-adjusted life years in 1990 to 54% in 2010.16 The economic impact is equally alarming, given that a 10% increase in the NCD rate entails a fall in gross domestic product of 0.5%.17 In 2010, the cost of NCD was put at $6.3 trillion, with an estimated increase of more than 100% in 2030 (reaching $13 trillion). Worldwide, the projected loss of economic earnings accumulated between 2011 and 2030 due to the impact of NCD will be $46.7 trillion, of which $21.3 trillion (46%) will affect low–middle income countries.10 The overall NCD burden in these countries will have negative consequences for poverty and for the already tougher economic conditions caused by communicable diseases, which undoubtedly will hold back development. Moreover, very few countries possess the financial resources needed to face the health care, economic, and social burden they will have to carry as a consequence of CVD.
CARDIOVASCULAR DISEASE IN LOW–MIDDLE INCOME COUNTRIESAccording to a study published in The Lancet, 80% of the burden of chronic diseases and 70% of deaths due to NCD in individuals aged < 70 years occur in only 23 countries.18 To illustrate what is behind this trend, let us take the example of India, where more than 1 billion inhabitants have rates of cardiovascular morbidity and mortality that are increasing more rapidly and affecting younger individuals than in the western countries.19 The country's economic growth, with rates among the highest in the world, is raising living standards for millions of citizens, who thus join a constantly expanding middle class. As in other Asian countries, like China and Indonesia, the growth of gross domestic product is helping tens of millions of people to move beyond the poverty threshold, promoting local development and raising living standards. However, this rapid economic growth creates economic and social tensions, like migration from rural areas to urban centers, inadequate infrastructure (transport, health, food, housing), as well as disturbing family and social structures and heightening income inequalities. Improved sanitation, hygiene, vaccination, and the control of communicable diseases increase life expectancy, but consequently, the number of individuals at risk of having chronic diseases grows, too. Moreover, urbanization brings with it important lifestyle changes, such as the reduction in physical activity and in expenditure of energy, increased consumption of a pro–atherogenic diet, and tobacco use.20 In this context, the INTERHEART and INTERSTROKE studies showed that all over the world ischemic heart disease and stroke share many risk factors: smoking, obesity, high blood pressure, dyslipidemia, diabetes mellitus, scarce consumption of fruit and vegetables, and physical inactivity.19,21 The rapid development of a region and the resulting social and economic changes create an environment that facilitates and promotes the appearance of CVRF; their impact on the population is causing the epidemic of CVD and of other chronic diseases in low- and middle-income countries. Unfortunately, the increased prevalence of these diseases, as well as the age group they affect (mainly<60 years) will, in the final instance, hold back the economic growth of developing countries due to the damaging effect that premature deaths and disability will have on productivity and the working class. Moreover, the increasing cost of health care will worsen the poverty rate because families will have to pay for longer periods of health care, drug treatments, and rehabilitation. In turn, these costs will put additional pressure on limited resources for national health care programs. Therefore, it is sadly paradoxical that more than 50 years of fighting against CVD in most of the Western world will be overshadowed by the rapidly increasing rate of CVD-related mortality in low–middle income countries, precisely because they have adopted Western lifestyles. At the same time, the aging of the population implies that health care systems will have to provide a response to individuals with heart disease, cancer, or cerebrovascular disease, and moreover that the rate of individuals with multiple chronic diseases will increase too. This multimorbidity disproportionately affects the poorer strata of society. Finally, nearly 9 million people in low–middle income countries who now benefit from antiretroviral therapy, with a marked improvement in survival, are beginning to develop comorbidities such as diabetes mellitus or CVD. Hence, health care systems will have to manage new patterns of disease coexistence, in which infectious diseases combine with NCD (a phenomenon termed the “double burden of disease”).12
STRATEGIES AND OPPORTUNITIES IN CONTROLLING THE CARDIOVASCULAR DISEASE EPIDEMIC: CARDIOVASCULAR HEALTH PROMOTIONCardiovascular prevention can be focused on the individual or the population. At the individual level, a stratification strategy is used, in which individuals undergo a study of the presence of risk factors and those identified as being above a cutoff point receive treatment. The advantage of this strategy is that the subject receives individualized treatment that optimizes the risk:benefit ratio. However, screening costs are very high and the risk prediction of most of the tools currently used (PROCAM, Framingham) remains imprecise and might not reflect real long-term risk.22,23 Moreover, using qualitative variables ignores the fact that the relation between most of the risk factors (blood pressure, low-density lipoprotein cholesterol, smoking) and CVD is continuous and linear. Therefore, we are facing what Rose termed the “prevention paradox”: when we intervene in high-risk individuals (who are a minority in the population), we miss our chance of intervening in intermediate-risk individuals—the majority of the population that presents with cardiovascular events.24 Therefore, the strategy for high-risk individuals should be accompanied by a population-wide strategy aimed at reducing CVRF levels in the entire population.25 Hence, it is important to apply 2 different large-scale intervention strategies: health promotion and disease prevention. Cardiovascular health promotion is based on promoting and maintaining low cardiovascular risk. However, preventing CVD centers on patients with high cardiovascular risk of having critical events—for example, acute myocardial infarction or stroke—and interventions to palliate the impact of these events on health. Thus, health promotion generally entails population-wide interventions, whereas CVD prevention is individual.
Which, then, is the better strategy? Primordial prevention seems to be the better choice in the long term.26 This involves preventing risk factors from occurring by optimizing lifestyles associated with good control of blood pressure, low concentrations of cholesterol, ideal body weight, the practice of physical exercise, and abstinence from tobacco use. An intervention of this kind requires mitigating CVRF, promoting health, implementing healthy living policies, and creating a physical environment that leads to adopting and maintaining lifelong heart-healthy lifestyles, from infancy to old age.
We know that the classic risk factors are interrelated and also associated with psychosocial factors, factors related to health care systems (access to quality medicine, which includes prevention programs and early NCD detection), and inter–sector factors (agriculture, exports, development, commerce, transport, and so on). These decisive, interrelated factors provide a conceptual platform to develop an integrated long-term strategy for the prevention and control of CVD (Figure 3). To implement this strategy, we need a coordinated intervention throughout various sectors to integrate health promotion and disease prevention and treatment. Moreover, this strategy can theoretically induce positive synergies between multiple interventions, whether individual- or population-based, at 3 different levels: political, legislative and regulatory strategies; health promotion through advertising; and the development of quality health care systems.
The components of regulation strategies and health care policy and legislation, such as regulations, incentives, and guidelines, can directly affect individual outcomes by interventions in the context of environmental risk. Ideally, these interventions would be inter–sector, so they would affect health care policies and sectors with an impact on population health (like regulating the sale of manufactured foods rich in salt and saturated fats, agriculture, transport, urban development, and education), encouraging them to plan so that they do not decrease cardiovascular health (or at least not have a negative health effect). The second category of strategies involves health promotion through communication and education. Advertising campaigns in the workplace, schools, and communities have the potential to motivate change in risk behaviors. In a coordinated strategy, moreover, they can strengthen policies, norms, and clinical interventions coming from the health care system. The third component in this schema involves relying on a health care system capable of a top-quality clinical response for disease prevention, treatment, and management, not only to identify and treat high-risk individuals but also capable of intervening in risk behaviors and increasing adherence to medical recommendations. This integrated strategy represents an ideal view of a solution that is conceptually simple (follow a healthy diet, regularly participate in sports activities, not smoke, and have regular contact with the health care system). Reality, of course, complicates this ideal model considerably. Changing individual behavior is complex and individual choices are strongly influenced by social and environmental factors. Governments must balance priorities that compete for limited resources and, in this sense, chronic diseases have historically lost the battle against other health problems, precisely because of their long “incubation period”. Moreover, developing countries face the added lack of infrastructure and technical capabilities not only in health care programs but also in implementing legislation and regulations aimed at protecting the health of the population.
However, even when we cannot attain an ideal system, we can successfully make a significant impact on CVD. In a scenario of limited resources, we should adopt pragmatic strategies to prioritize elements that, based on the best evidence available, are economically feasible and have the greatest chance of successfully improving measurable indices of health.
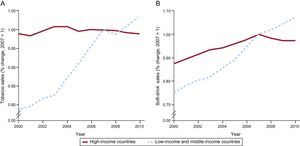
Therefore, cardiovascular prevention should include multiple strategies: changes in health care policy aimed at promoting and maintaining healthy lifestyles, reinforcement of individual behavior, and the use of safe, effective drugs to control CVRF. In theory, lifestyle interventions are attractive not only because this is a natural approach but because of the perceived low cost, simplicity, and inherent safety of this type of measure. However, despite the fact that CVD is largely part of the biological expression of an inappropriate lifestyle (therefore, of inappropriate behavior), interventions on behavior to modify lifestyle are generally very expensive. At best, they have a moderate effect that does not last and, in longitudinal studies, they have not been shown to reduce cardiovascular events. Hence, changes in health care policy, the environment, and sociocultural attitudes should have a greater impact on controlling exposure to CVRF. For example, it has been proven that anti-tobacco laws forbidding smoking in closed spaces, which several countries have adopted and in Spain came into force in January 2011, have had an impact on the reduction of cardiovascular events. The data published in Germany are encouraging, given that 1 year after implementing the law, the rate of hospitalizations for angina fell by 13.3% (95% confidence interval [95%CI], 8.2-18.4%) and hospitalizations for acute myocardial infarction fell by 8.6% (95% CI, 5.0-12.2%), reversing the growing trend in admissions for infarction seen in the years before the law came into force. The reduction in admissions for infarction was significantly greater among the young, with no difference between the sexes. In addition to the health care benefit, the cost of hospitalizations for angina fell by 9.6% (a €2.5 million savings) and the cost of acute myocardial infarction fell by 20.1% (a €5.2 million savings) after the law had been in force for 1 year.27 Nonetheless, this type of intervention has not been adopted by emerging countries where smoking (as well as other risk factors) continues to grow alarmingly20 (Figure 4). Therefore, and in line with the concept of implementing different actions at different levels, the use of safe, cheap pharmacologic therapies in a fixed combination, such as the “polypill”, is another promising strategy in CVD prevention.
Trends in tobacco sales and soft drinks sales, 2000-2010. Reproduced with permission from Yusuf et al.19
In the developed world, access to quality health care systems and therapies of proven effectiveness in reducing cardiovascular mortality has successfully mitigated the consequences of CVD and has increased survival. However, the worldwide reality is quite different. Half of all the world's patients with acute myocardial infarction do not receive cardioprotective therapy to avoid the recurrence of cardiovascular events, and only 13% of those in low–middle-income countries receive treatment.28 These figures can be explained in different ways: inadequate prescription, limited access to the health care system, and the cost of drugs are some of the obstacles to optimal management of patients. These obstacles are much more striking in low–middle-income countries and in more deprived populations in high-income countries. Moreover, even when medication is available, patients tend not to adhere to clinical recommendations. The phenomenon of adherence, which has been studied in depth, is complex, but we know that one of the factors that most influence adherence is the complexity of treatment and the number of pills taken per day.29 Therefore, the strategy of just once a day taking a single drug that combines different active ingredients that intervene simultaneously on the CVRF (“polypill”) could theoretically have a very significant impact on reducing CVD in the world.
Approximately half of the reduction in cardiovascular mortality observed in the developed world in the last 20 years is due to drug treatment.30 It has been shown that acetylsalicylic acid, beta blockers, statins, and renin-angiotensin system blockers (angiotensin-converting enzyme inhibitors and angiotensin receptor blockers) reduce cardiovascular mortality in secondary prevention. Despite the available evidence, the number of patients receiving appropriate treatment is alarmingly low, and the reasons for this are complex and multi-factor. Firstly, treatments with proven efficacy are not prescribed to patients when indicated. Specifically, in secondary prevention of coronary heart disease in Europe, the EUROASPIRE III study found high prevalence of smoking (17%), obesity (35%), high blood pressure (56%), and high levels of cholesterol together with low density lipoproteins (25%) in patients with ischemic heart disease; treatment with statins and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, although better by comparison with previous studies, remained at suboptimal levels of 71% and 78%, respectively.31 In emerging countries, the outlook is desperate: data from the PURE study28 have recently been published and show the disparities of treatment and control of high blood pressure between the developed world and low- or middle-income countries (36.9% vs 31.7% respectively). The WHO has studied this in its WHO-PREMISE registry,32 conducted in 10 low–middle-income countries, finding that acetylsalicylic acid was correctly prescribed in 81.2% of patients with ischemic heart disease and 70.6% of patients with cerebrovascular disease; beta-blockers, in 48.1% and 22.8%; angiotensin-converting enzyme inhibitors in 39.8% and 37.8%, and statins in 29.8% and 14.1%, respectively. A recent study in rural India found that among patients with ischemic heart disease, only 14% were being treated with acetylsalicylic acid, 41% with antihypertensive agents, and 5% with statins.33 Given that population growth is greatest in low- and middle-income countries, which represent 80% of the world population, and that the predictions of increased CVD incidence are greater in those geographic areas,34 we are facing a problem of global magnitude, where access to treatment is more precarious and disease is going to affect, above all, patients<60 years of age. This will undoubtedly have devastating consequences on the potential socioeconomic development of these countries. Secondly, we know that adherence to long-term treatment is not good; often fewer than half of patients adhere to drug treatment—principally due to social, cultural, psychological, economic, and clinical reasons related to the patient, physician, health care system, and the interrelations between them.35 The lack of adherence has significant consequences, as the interruption of medical treatment is associated with an increased rate of recurrent cardiovascular events and mortality in patients with CVD. Finally, we should consider the cost:effectiveness ratio and the fact that medicines should be accessible. Although these drugs have been proved to be cost-effective, they remain inaccessible to most subjects in low–middle-income countries today.36
The strategy of using a single pill that combines generic preparations of proven efficacy to reduce cardiac events in secondary prevention (“polypill”) represents a potential solution to some of the causes of the failure in secondary prevention.
CONCLUSIONSThe scientific societies are under an obligation to use their knowledge and experience in the worldwide fight against CVD and chronic conditions. Recently-proposed innovations include strategies to control tobacco and reduce dietary sodium, which could prevent > 1 million deaths per year in the emerging countries, at a cost of approximately $0.50 per person per year.37,38
The use of cheap, safe pharmacologic therapies in fixed combinations, like the “polypill”, represents another promising strategy in CVD prevention. Recent reports have made low-cost public health recommendations that could make a substantial impact, like controlling dietary sodium intake and implementing measures to control smoking. The task ahead will be arduous, or so it seems, but we are morally obliged to support the worldwide fight against CVD, the pandemic of our age.
CONFLICTS OF INTERESTNone declared.