To the Editor,
In transcatheter aortic valve implantations (TAVI), temporary transvenous pacing is essential for rapid pacing as well as for backup pacing. The use of a temporary ventricular pacing wire may be associated with lead displacement and right ventricular perforation, and limits patient mobilization in case of femoral access. We hereby report our experience using a temporary pacing strategy in TAVI that allows immediate patient mobilization and potentially safer prolonged temporary pacing.
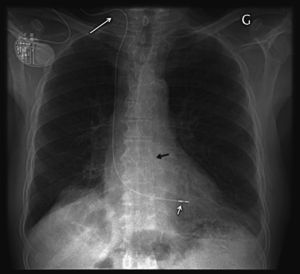
A 58-cm bipolar screw-in lead (Tendril 1888 TC, St Jude Medical) is inserted under aseptic conditions via the internal jugular vein through a peel-away introducer (FlowGuard 7F-sheath, Enpath Medical Inc) and subsequently advanced to the right ventricle under fluoroscopic guidance using a preshaped stylet. The helical screw is extended using the fixation tool provided with the lead, with confirmation of helix extension by fluoroscopy. Satisfactory electrical parameters are capture threshold <1.5V/0.5ms and R-wave sensing amplitude >4mV. The lead is then fixated to the skin using the suture sleeve, and sterile dressing is placed over the insertion site. High-rate pacing is achieved using crocodile clips connected between the lead and a pacemaker analyzer. For prolonged backup pacing, the pacemaker lead is connected (Figure 1) to an explanted conventional permanent pacemaker (<3years old), retrieved from deceased patients or from those requiring device upgrade. Prior to use, explanted pacemakers are thoroughly cleaned but not sterilized, as they remain outside the sterile field. The pacemaker is programmed for backup single chamber ventricular pacing according to the patient's needs. Interrogation of the pacemaker memory allows analysis of heart rate histograms and quantification of ventricular pacing (available information varies according to pacemaker models). Lead explantation can be performed simply at the patient's bedside (after screwing back the helix).
Figure 1. Chest X-ray after CoreValve implantation (black arrow). A screw-in lead was inserted via the right internal jugular vein (long white arrow), fixated to the right ventricle apex (short white arrow), and connected to an explanted permanent pacemaker.
We have used this pacing strategy in 20 patients (12 males, mean age 85±5.7years, left ventricular ejection fraction 50.5±12.9%, logistic EuroSCORE 28.6±15%) undergoing TAVI with the Medtronic CoreValve system, both preprocedure for delivering high-rate pacing during balloon valvuloplasty (100% successful 1/1 180-bpm rapid pacing) as well as for postprocedure backup pacing recommended for a minimum 48h. We explanted temporary leads after 5.6±1.9days (mean±SD), whereas intensive care unit stay was only 1.8±1.1days (in-hospital days: 11.3±4.7). Permanent pacemakers were implanted in 30% and 30-day mortality was 10%. Our experience has shown the pacing technique to be reliable, with no significant complications (no pneumothorax, pericardial effusion, or neck hematoma requiring compression).
This approach has several potential advantages over the use of temporary wires. First, active fixation leads may decrease the risk of accidental lead displacement that is observed with temporary pacing wires. This is important to ensure backup pacing in the advent of atrioventricular block, but also during high-rate pacing at the time of deployment of the balloon-expandable Edwards-SAPIEN aortic valve, as failure of 1:1 ventricular capture - common above 150 bpm with a floating temporary lead1 -may result in valve migration with serious consequences. Second, since permanent leads are more flexible than temporary wires, the risk of right ventricular perforation is expected to be lower. The risk of perforation is even lower if the lead is implanted on the interventricular septum. Third, this strategy allows immediate mobility and early discharge from a telemetry unit. Fourth, the percentage of ventricular pacing and rate histograms stored in the pacemaker memory may help in deciding whether a permanent pacemaker is indicated, especially if the patients are discharged to wards without telemetry.
The higher cost of a pacemaker screw-in lead compared to a temporary wire (500 versus 90 Euros) is a drawback, but the cost difference is compensated by a reduced length of stay in a monitored unit. Chihrin et al.2 showed cost equivalence after only 18h and cost saving thereafter when active fixation leads are used instead of conventional temporary leads. Earlier patient mobility and a potentially decreased risk of complications (lead displacement or perforation), may also improve outcome and save costs.
This strategy, using an explanted permanent pacemaker connected to a regular screw-in lead, may also be of interest in other procedures at risk of inducing atrioventricular block (eg, alcohol septal ablation) or in clinical settings requiring prolonged temporary pacing.3
Corresponding author: haran.burri@hcuge.ch