As in other fields, understanding of vascular risk and rehabilitation is constantly improving. The present review of recent epidemiological update shows how far we are from achieving good risk factor control: in diet and nutrition, where unhealthy and excessive societal consumption is clearly increasing the prevalence of obesity; in exercise, where it is difficult to find a balance between benefit and risk, despite systemization efforts; in smoking, where developments center on programs and policies, with the electronic cigarette seeming more like a problem than a solution; in lipids, where the transatlantic debate between guidelines is becoming a paradigm of the divergence of views in this extensively studied area; in hypertension, where a nonpharmacological alternative (renal denervation) has been undermined by the SYMPLICITY HTN-3 setback, forcing a deep reassessment; in diabetes mellitus, where the new dipeptidyl peptidase-4 and sodium-glucose cotransporter type 2 inhibitors and glucagon like peptide 1 analogues have contributed much new information and a glimpse of the future of diabetes treatment, and in cardiac rehabilitation, which continues to benefit from new information and communication technologies and where clinical benefit is not hindered by advanced diseases, such as heart failure. Our summary concludes with the update in elderly patients, whose treatment criteria are extrapolated from those of younger patients, with the present review clearly indicating that should not be the case.
Keywords
Cardiovascular (CV) prevention befits advanced societies that not only act before disease appearance, but adopt more demanding criteria when the disease is already present. In keeping with the times, the concepts of effectiveness, efficiency, pharmacoeconomics, opportunity cost, and general health economics are interwoven in our daily work.1 Interventions in primary CV prevention have a lower individual cost than those of the disease stages, but are applied to such broad swathes of the public that they end up costing much more and require a more thorough analysis, which is far from being well established. The present article covers the most important update of the past year in vascular risk and rehabilitation, with an effort made to summarize the developments most relevant to clinical practice.
EPIDEMIOLOGICAL ASPECTSJust a century ago, CV disease caused less than 10% of all deaths. Propelled by industrialization, urbanization, and lifestyle changes, the 20th century saw an unprecedented increase in life expectancy, with a radical change in the causes and rates of mortality. Now the number one cause of death, CV disease is responsible for more than 30% of deaths worldwide, with a preferential distribution in economically developed countries.2 Given the modifiable character of certain known risk factors, the efficient application of preventive strategies and therapies might alter the natural course of the epidemiological transition worldwide and thereby reduce the global impact of CV diseases. However, we are far from reaching excellence in this regard.
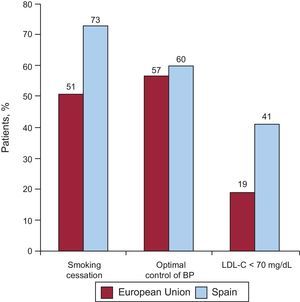
The data of the EUROASPIRE IV registry3 showed that only 51% of patients had stopped smoking between 6 months and 3 years after a coronary event, 43% had blood pressure (BP) readings above target values, 81% failed to achieve the lipid control targets, and 59% had not participated in any CV risk prevention program.4 These data agree with results of the PURE study,5 conducted in patients with atherosclerotic CV or cerebrovascular disease. In this study, there was a low prevalence of healthy lifestyles, with only half quitting smoking, 39% following a suitable diet, and 35% performing physical activity. The Spanish data from the EUROASPIRE IV registry were slightly better than the European average (Figure 1), with 73% of patients quitting smoking, 40% with suboptimal control of BP, and 59% failing to achieve the target levels of low-density lipoprotein cholesterol, results that concur with those published in the ENRICA and BARBANZA group studies.6,7 Notably, a high percentage of patients in most studies were receiving the treatments recommended by the guidelines, but most patients failed to achieve the control targets for their risk factors, indicating the need to encourage both the attending physician and the patient to individualize the dose and type of drug, as well as to prompt lifestyle changes.
Distribution of patients with adequate control of cardiovascular risk factors after a coronary event, according to European Action on Secondary and Primary Prevention through Intervention to Reduce Events IV. BP, blood pressure; LDL-C, low-density lipoprotein cholesterol. Adapted with permission from Galve et al.9
The European guidelines on CV prevention are aware of this need, as well as the importance of tailoring the preventive strategy to the baseline patient risk.8 Accordingly, the guidelines establish specific recommendations for controlling each risk factor, stratifying the baseline risk in accordance with the SCORE (Systematic Coronary Risk Evaluation). system. Cardiac rehabilitation (CR) is currently a class I recommendation in all clinical practice guidelines, meaning that its use is based on a demonstrated benefit in multiple studies; nonetheless, CR continues to be underused. Thus, all of the data appear to support the need to strengthen comprehensive and multidisciplinary prevention programs in which both patients and their families participate, as well as ensuring an organizational model that integrates primary and specialized care.9
DIET AND WEIGHTThe review of Arós and Estruch10 on the Mediterranean diet is recommended nutrition-related reading because it summarizes the global impact of the Spanish PREDIMED study.11 This trial has indisputably emerged as a benchmark in CV prevention and the researchers involved continue to publish data on the preventive aspects of the diet (30 articles already on PubMed from 2014 and more than 110 overall).12 Similarly, the SUN study,13 showed a reduced incidence of metabolic syndrome with a “pro-vegetarian” diet.
Another interesting publication is the epidemiological study Di@bet.es, which showed a high percentage of obesity (body mass index > 30) in people older than 18 years in Andalusia (37%), a significantly higher rate than the rest of Spain (27%).14 Another Spanish weight-related study, REDINSCOR,15 showed improved survival in heart failure patients with higher BMIs (until a certain limit). Recently, Spanish groups have also studied the prevalence of infant obesity (which, although high, seems to have stabilized in the last decade) and its hemodynamic consequences.16,17
Among the relevant international studies, one with strong results analyzed 20 studies in obese patients (body mass indez > 40), showing a life expectancy 10 years shorter due to death from any cause, not just CV related.18 The Swedish Obese Subjects study caused great commotion; after a long follow-up, the study showed the tremendous benefits of bariatric surgery on diabetes mellitus and macrovascular complications.19 The CARDIA study20 analyzed the influence of 5 lifestyle measures (obesity, low alcohol intake, a healthy diet, physical activity, smoking) in Americans aged between 18 and 30 years at baseline, finding a clear relationship with subclinical atherosclerosis parameters 20 years later.
Regarding nutritional supplements, it seems that studies of multivitamins have been put on hold following the negative results of the Physicians’ Health Study II.21 Studies of ¿-3 fatty acids limp onward, fanning continued controversy; due to recent failures to link them to prevention of atrial fibrillation, attention has lately turned to their preventive effects on CV mortality.22
One important study was the Cochrane review of nutritional supplements in familial hypercholesterolemia; as expected with such a high bar (short-term mortality and ischemia heart disease), there were no important findings.23
EXERCISE AND VASCULAR RISKSedentary lifestyles and excess weight are first-order health care problems that explain the high levels of hypertension (HT), diabetes mellitus, and hypercholesterolemia in both developed and developing countries. Physical exercise (PE) is implicated in the onset and development of vascular risk factors and is thus a cornerstone of their control. Accordingly, PE is recommended in all clinical practice guidelines. However, despite the unanimity concerning its importance, the adoption of heart-healthy lifestyles that include habitual PE remains a pending issue.
An important part of the work of health care professionals should be to help people to achieve long-term lifestyle changes. On one hand, this approach would require specific training for professionals to establish a monitoring strategy in the population habitually practicing PE, above all in the important subgroup of individuals that practice amateur sport but at high intensity, which carries risks of arrhythmic and ischemic complications and even sudden death. In this context, it is important to identify the at-risk individuals, to guide training to optimize cardiac adaptation, and to differentiate between normal and pathological cardiac adaptation.24
On the other hand, the “prescription” of PE should be made in a structured manner. Generic and empirical recommendations are habitually made, although they generally are abandoned. First of all, the terminology should be defined. Physical activity, PE, and sport are wrongly considered synonymous:
- •
Physical activity: combination of body movements produced by the contraction of skeletal muscles that expend energy.
- •
Physical exercise: planned, structured, and repetitive physical activity that has as intermediate and final objectives an improvement or maintenance of physical fitness and an increase in the functional capacity of the body.
- •
Sport: the practice of PE according to certain playing rules and a competition-oriented system.
Although PE prescription manuals and studies use the terms physical activity and PE interchangeably, it is more correct to speak of PE because not all physical activity positively stimulates health. The objective of a PE prescription is to obtain greater health benefits with fewer risks, while considering any specific and individual needs.
These aspects have been addressed in the past year by 2 publications. The PE prescription guidelines25 aim to promote the correct and individualized prescription of PE for healthy persons and patients with CV risk factors, based on the latest scientific evidence, and to provide health care support professionals with the format for its correct prescription. In addition, the ninth edition of the “Guidelines for exercise testing and prescription” of the American College of Sports Medicine was published,26 which reviewed the indications for the testing of individuals performing sporting activities and the guidelines for their correct prescription.
SMOKINGOne notable psychosocial work on the impact of warning labels (which some consider of neutral or transitory effectiveness) showed that such labels can support smoking cessation by prompting smokers to consider the risks of smoking; the more striking and eye-catching the labels, the more effective they are.27
Many people believe that it is almost impossible to get adolescents to stop smoking. One study28 identified predictors of smoking cessation in nascent adolescent smokers. During follow-up, 40% quit smoking. Male sex, age, and the practice of sport were associated with greater abstention, whereas substance abuse, excess weight, and family stress were related to greater difficulty in smoking cessation.
The relationship between sexual orientation and smoking was studied in 28 198 participants in Sweden.29 The authors hypothesized that there would be a higher prevalence of smoking in sexual minorities, partly because they have less social capital (understood as structures, networks, and social relationships) due to discriminatory societal attitudes: although it was confirmed that homosexual and bisexual people smoke more, the trend persisted after adjusting for social capital, indicating the involvement of other factors.
In a Cochrane review30 of antidepressants and smoking (quitting can trigger depressive episodes), bupropion (44 trials) and nortriptyline (6 trials) significantly improved long-term abstinence; the mechanism appears to be independent of their antidepressant effect. There was no efficacy with reuptake serotonin inhibitors or monoamine oxidase inhibitors.
The growing social phenomenon of electronic cigarettes should now be considered a threat to public health in Spain because of the lack of evidence for their usefulness in smoking cessation or reducing tobacco risk and because they are tending to normalize smoking behavior, threatening the as-yet unconsolidated achievements of legislation.31
LIPIDSPublished at the end of 2013, the new guidelines of the American Heart Association/American College of Cardiology on dyslipidemia clearly recapitulate the new update in this field.32 The guidelines recommend intensive treatment with statins for patients with atherothrombotic CV disease or at high risk of it, which marks a clear difference from the European guidelines33 that identify some specific cholesterol targets for each risk category. The American guidelines base their risk estimation on 4 key points: presence of CV disease, low-density lipoprotein cholesterol ≥ 190mg/dL, diabetes mellitus, and estimated 10-year risk based on a custom scale (Figure 2). Because this scale had not been validated, it has been widely criticized.34 Moreover, a combined analysis of 3 prospective studies of primary prevention showed that the risk equation proposed by the American guidelines overestimates the risk by between 75% and 150% and increases the number of patients that should begin statin therapy by between 40% and 50%.34 However, the approach of the American guidelines appears correct for secondary prevention. Finally, the debate over the ideal treatment for dyslipidemia continues, as shown by an initiative to improve the treatment and evaluation of dyslipidemia.35
Results of the Control de Hiperglucemia y Actividad Plaquetaria en Pacientes con Síndrome Coronario Agudo. study. Platelet reactivity in patients intensively treated with insulin vs conventional therapy. At the moment of hospital discharge. A: patients with worse glycemic control (glycated hemoglobin > 6.5%). B: patients with better glycemic control (glycated hemoglobin > 6.5%). C: One-year follow-up. ADP, adenosine diphosphate; GPIIb/IIIa, glycoprotein IIb/IIIa; PRI, platelet reactivity index; TRAP, thrombin receptor activating peptide. Reproduced with permission from Vivas et al.47,48.
As already mentioned, a subanalysis of the PREDIMED study has shown benefits of a diet supplemented with nuts and olive oil on total cholesterol and low-density lipoprotein cholesterol, as well as on BP and blood sugar.36
HYPERTENSIONAfter almost 11 years, the latest report of the JNC 837 on the management of HT in adults appeared in 2014, offering 9 recommendations based on scientific evidence (Table).
Summary of the Recommendations of the Eighth Joint National Committee
| 1 | In the general population older than 60 years, pharmacological treatment is initiated with SBP > 150mmHg or DBP > 90 mmHg; target BP, SBP < 150mmHg and DBP < 90mmHg (A) |
| 2 | In the general population younger than 60 years, pharmacological treatment is initiated with DBP > 90 mmHg; target BP, DBP < 90mmHg (A). |
| 3 | In the general population younger than 60 years, pharmacological treatment is initiated with SBP > 140 mmHg; target BP, SBP < 140mmHg (E). |
| 4 | In the population older than 18 years with chronic kidney disease, pharmacological treatment is initiated if SBP is > 140mmHg or DBP is > 90 mmHg; target BP, SBP < 140mmHg and DBP < 90mmHg (E). |
| 5 | In the general population older than 18 years with diabetes mellitus, pharmacological treatment is initiated with SBP > 140mmHg or DBP > 90 mmHg; target BP, SBP < 140mmHg and DBP < 90mmHg (E). |
| 6 | In the general nonblack population, including those with diabetes, the initial treatment should include thiazides, calcium antagonists, ACE inhibitors, or ARB (B). |
| 7 | In the general black population, including those with diabetes, the initial treatment should include thiazides or calcium antagonists (B). |
| 8 | In the population older than 18 years with chronic kidney disease and HT, the initial treatment (or second drug) should include ACE inhibitors or ARB to improve renal function (this is applicable to all patients with HT, regardless of race or diabetes status) (B). |
| 9 | Management strategy: if the BP targets are not met following 1 month of treatment, the drug dose should be increased or a second drug should be added (thiazides, ACE inhibitors, ARB or calcium antagonists). If the BP targets are not reached with the second drug, a third should be added, without using ACE inhibitors + ARB. If the BP targets are not reached with the 4 recommended drugs (whether due to a contraindication or because more than 3 drugs are needed), other antihypertensives can be used. Patients should be referred to a specialist if the BP targets cannot be achieved despite following all these indications and after all therapeutic steps (E). |
ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blockers; BP, blood pressure; DBP, diastolic blood pressure; HT, hypertension; SBP, systolic blood pressure.
The capital letter at the end of each recommendation denotes the strength of the recommendation, from A (maximum evidence) to E (only expert opinion).
Adapted with permission from James et al.37
The SYMPLICITY HTN-338 study heralded a radical change in HT interventionism. Previously, the clinical approach relied on unblinded studies showing that renal artery denervation reduced BP in resistant HT. However, the publication of a more rigorous study (blinded and with a sham control arm) revealed unexpected results: there were no significant differences in systolic BP and outpatient BP monitoring at 6 months in 535 patients. The earlier success could be explained by a placebo effect or other circumstances (eg, the Hawthorne effect), or treatment adherence, or perhaps because the treated HT was not actually refractory. This result sullies the once-promising future of the technique. The problem may be patient selection (to define whether a certain subgroup benefits), the technique used, or the suitability of the denervation device.
In this respect, a Spanish cross-sectional study (with its inherent limitations) has been published on primary care for resistant HT (63 167 patients), showing that 1 out of 4 patients is older than 80 years (associated with female sex, obesity, diabetes mellitus, heart disease, and kidney disease), whereas in those younger than 50 years this form of HT was associated with male sex, obesity, stroke, and kidney disease.39 In addition, 2 prognostic studies have been published. The first publication showed that a morning increase in systolic BP > 23mmHg in elderly patients with treated hypertension was an independent factor for stroke in individuals with a circadian dipper rhythm, but not in those with a non-dipper rhythm.40 The second study analyzed 1.25 million people without CV disease (20% on antihypertensive therapy), with a 5.2-year follow-up; the group with lower risk had a systolic BP between 90 and 90-114 mmHg and a diastolic BP between 60 and 74 mmHg without a J-shaped curve.41
Finally, an intriguing and useful study in 102 patients showed that outpatient monitoring of BP for only 1 h during daytime hours is valid for HT diagnosis and subpopulation classifications (white coat, refractory).42
DIABETES MELLITUSThe debate continues over the CV safety of the new antidiabetics, beyond their effectiveness in controlling hyperglycemia. Various related meta-analyses have been published in the last year. Increased heart failure has been shown in patients treated with dipeptidyl peptidase-4 inhibitors (odds ratio = 1.19; P < .015)43; this finding is based only on studies designed with CV endpoints and it had not been seen in a meta-analysis prior to the publication of the SAVOR and EXAMINE studies.44
Glucagon-like peptide 1 agonists have been evaluated in 37 trials. In low-risk patients, a reduction was seen in CV events with these drugs vs placebo and vs pioglitazone, as well as a favorable trend (although nonsignificant) vs dipeptidyl peptidase-4 inhibitors,45 but we have to wait for ongoing trials with CV endpoints to confirm the results (the first results will be available in 2015).9
Sodium-glucose cotransporter-2 inhibitors have shown a good safety profile and lipid-lowering efficacy (reduction of glycated hemoglobin, 0.5%-0.6%) and additional benefits such as weight loss, reduced BP, and increased high-density lipoprotein cholesterol; however, development of mild genitourinary infections was reported.46 Nonetheless, we have to wait for the results of two trials with CV endpoints, CANVAS (CANagliflozin cardioVascular Assessment Study) with canagliflozin in 2017 and DECLARE-TIMI 58 (Dapagliflozin Evaluation of Cardiovascular Events-Thrombolysis In Myocardial Infarction 58) with dapagliflozin in 2019.
Another important issue is the treatment of hyperglycemia in acute coronary syndrome. Platelet function is altered in diabetic patients and hyperglycemia-associated platelet hyperactivation is produced by multiple independent pathways of thromboxane A2. A beneficial relationship between intensive treatment with insulin and platelet reactivity was only found in patients with elevated glycated hemoglobin in the CHIPS study of Vivas et al47 (Figures 2A and B). In the 1-year follow-up, and despite continued significant differences in blood glucose control (104 mg/dL in the intensive treatment group vs 119 mg/dL), there was no significant difference in platelet aggregation between the groups (Figure 2C).48 An interesting finding of this study was that implementation of an aggressive protocol for long-term outpatient management of hyperglycemia in patients with acute coronary syndrome was feasible and potentially safe, with a low percentage of severe hypoglycemia, and may reduce renal deterioration progression compared with a conventional protocol.49
CARDIAC REHABILITATIONAs a general comment, we must highlight the abundance of publications on CR authored by nursing staff. Many studies have stressed the different characteristics of CR in different countries. The most-studied aspects are CR in heart failure and the use of smartphones.
A review of CR in cardiac surgery patients detailed all aspects of the multidisciplinary strategy used.50 The American registry of CR after myocardial infarction showed a progressive increase in the number of patients referred to these programs between 2007 and 2012.51
The Cochrane review of CR in heart failure52 supports the conclusions of an earlier review showing reduced hospital admissions and noteworthy improvements in quality of life. Another Cochrane review53 to promote patient approval and CR adherence found weak evidence for the effectiveness of interventions aimed at recruiting patients to CR.
The article of Ades et al54 reviewed the current evidence on the benefits and risks of exercise and self-care advice in patients with heart failure in CR, offered recommendations for patient selection, and discussed the role of CR in the promotion of self-care and behavioral changes. In the study of Völer et al,55 patients who underwent transcatheter aortic valve implantation benefited from CR despite their advanced age and comorbidity.
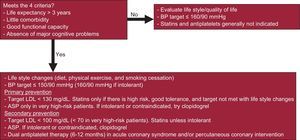
ELDERLY PATIENTSFor the first time in Spain, a consensus document has been published on the treatment of the vascular risk factors of octogenarians.56 The document stresses lifestyle modifications, a less stringent BP target (≤ 150/90mmHg or ≤ 160/90mmHg if there is intolerance or relevant comorbidity), and avoiding systolic BP < 120mmHg and diastolic BP < 80mmHg. The remaining recommendations are summarized in Figure 3. Physicians should determine if the octogenarian meets 4 criteria (life expectancy > 3 years, little comorbidity, good functional capacity, and absence of major cognitive problems). If so, the treatment can be more aggressive. A more conservative approach has to be adopted if any criterion is not met. In this document, as in other recent ones,57,58 primary prevention with statins is not recommended for octogenarians. The recommendation of a previous document59 was also ratified: for fragile and diabetic elderly patients, the blood glucose control targets should be lax (glycated hemoglobin < 8.5%) due to the known risks of overtreating diabetes mellitus in elderly patients, except in those with symptomatic hypoglycemia or hyperglycemia.60
Summary of the recently published recommendations on the treatment of cardiovascular risk factors of octogenarians. ASA, acetylsalicylic acid; BP, blood pressure; LDL-C, low-density lipoprotein cholesterol. *Low-dose (75-100 mg). Reproduced with permission from Gómez-Huelgas et al.56.
Regarding antihypertensive combinations, the APOLLO study61 in hypertensive elderly patients (mean age, 72 years) showed that combined treatment is safe and achieves greater BP reductions, with a trend toward a reduction in CV events. Having said that, a greater reduction in BP was accompanied by a risk of symptomatic hypertension and injurious falls.62
CONCLUSIONSBecause they concern the vast majority of the population, each year sees the appearance of broadly applicable findings in the broad network of areas comprising vascular risk and CR. The present article has summarized these results, emphasizing the most relevant. The developments have involved researchers, health care professionals, scientific societies, and health care authorities. A noteworthy effort has been made in the systemization and structuring of recent knowledge. The considerable accumulation of findings gives rise to reviews that continuously engender clinical practice guidelines and consensus documents, which help physicians in clinical practice. However, in an era marked by evidence-based medicine, clinical practice is seen as more fragile than previously thought, due to the divergences and controversies emanating from the standards and recommendations.63 However, knowledge is not monolithic, and even dissension is valuable.
CONFLICTS OF INTERESTNone declared.