Keywords
INTRODUCTION
Bifurcated coronary lesions are frequent, representing approximately 10%-12% of all coronary interventions.1 In percutaneous treatment, initial procedure success is lower and the restenosis rate is higher than in nonbifurcated lesions.2 Many approaches to these lesions have been described,3,4 but none of them has gained popularity enough to be considered definitive. Broadly speaking, they divide into 2 groups: simple techniques, with a single stent implanted in the main vessel (MV), and complex techniques, with a stent implanted in the side branch (SB). The literature5-7 suggests simple techniques are superior, so a philosophy based on implanting a single stent whenever possible seems adequate. We follow a stepwise strategy8 using SB dilatation, when the SB is affected or plaque displacement occurs on MV stent deployment, and only implant a second stent in the SB when results are less than optimal. In earlier series, this occurred in <10% of bifurcations treated. Some in vitro studies9 show stent distortion occurs in the segment immediate to SB origin when the SB is dilated—we call this segment the "lower diamond"—and that this can be corrected with the simultaneous inflation of 2 superimposed balloons (KB). On the basis of these studies, some groups propose systematic, procedure-final KB dilatation.10,11 However, the behavior of a stent implanted in the wall of a vessel with atheroma plaque can differ from its in vitro behavior and clinical information on this in patients treated with a simple approach (ie, a single stent) is unavailable. The objective of the present study is to determine in vivo the changes in the geometry of stents implanted in the MV after balloon dilatation, through the stent cells, in the SB, and after performing procedure-final KB.
METHODS
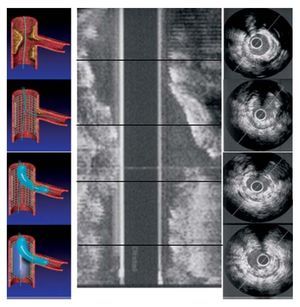
We conducted a prospective observational study in 23 consecutive patients with coronary lesions affecting a bifurcation, excluding those with SB diameter <2.5 mm. Baseline clinical data are summarized in Table 1. Most patients were men, with high blood pressure, smokers; more than half presented in an unstable situation. Baseline angiographic characteristics (Table 2) indicate 35% of lesions were calcified and the most frequent location was at the level of the left anterior descending coronary artery with the diagonal. We used Medina's classification12 to define the segments of the bifurcation that are compromised. In 14 (60%) patients the 3 segments of the bifurcation were affected and in 5 (24%) the SB became affected following MV stent deployment. All stents were drug-eluting. Intracoronary ultrasound (IVUS) studies (Atlantis SR, Boston Scientific 2.5 F, 40 MHz) were performed after administering a 200 µg nitroglycerin bolus, with motorized withdrawal at 0.5 mm/s. In 12 (52%) patients a baseline IVUS was conducted. All patients underwent IVUS after MV stent implantation, SB balloon dilatation, and simultaneous inflation of 2 superimposed balloons in KB. The balloon used for SB dilatation was chosen as a function of vessel diameter and inflated at 6-8 atm; we observed no residual stenosis in any patient. In KB dilatation, in MV we used the stent balloon or another of a similar diameter, reaching inflation pressures of 12-14 atm; in SB, we used the balloon previously employed in the isolated SB dilatation, with inflation pressures of 6-8 atm. In each case we measured stent area and symmetry index (minimum stent diameter/maximum stent diameter) in the segment proximal to the stent, at SB origin level, in the segment immediate to SB origin, and in the segment distal to the stent. We determined area gain or loss and the changes produced in stent geometry after each maneuver performed (Figure 1). We also measured the angle between SB and MV, and correlated this with the degree of distortion produced in the lower diamond after isolated SB dilatation. Measurement was offline by 2 expert interventional cardiologists.
Figure 1. Ultrasound study protocol. On the left, you can see each of the conditions under which IVUS was conducted and on the right, the stent segments studied at each stage.
We used the Kolmogorov-Smirnov test to show sample distribution was normal. Quantitative variables are expressed as mean (SD). We used ANOVA and the Bonferroni test to compare multiple means. Linear associations were calculated using the Pearson correlation. A P value less than .05 was considered significant. Statistical analysis was with SPSS 12.0.
RESULTS
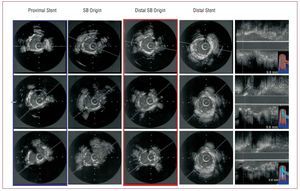
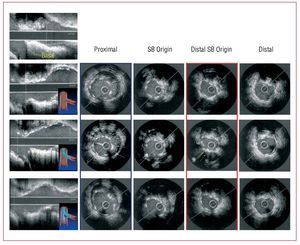
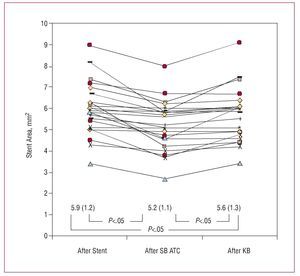
We achieved initial procedure success in all patients. One patient (4%) needed a second stent implant in the SB as postdilatation results were suboptimal. Tables 3 and 4 summarize ultrasound findings of the segments analyzed at each stage. In the segment proximal to the stent and at the level of the SB origin a significant increase of area and a loss of stent geometry occurred after KB inflation (Figures 2 and 3). In the segment immediate to SB origin, some degree of distortion and loss of area occurred after SB dilatation. Following KB, area increased slightly without regaining baseline values despite MV stent balloon diameter being greater than that of the SB stent and inflation being performed at higher pressure (12-14 atm in MV vs 6-8 atm in SB). Figure 4 illustrates individual changes in stent area in this segment after each intervention. We found no correlation between SB angle and the degree of distortion produced in the lower diamond after isolated SB dilatation. We identified no significant differences in the distal stent at any stage.
Figure 2. Ultrasound study of the main vessel after stent implantation, following side branch dilatation, and after kissing balloon inflation. The proximal segment of the stent appears in a blue box, where you can see the increase in the area and the distortion of stent geometry following kissing balloon inflation. The distal segment at the origin of the side branch appears in a red box and does not vary in the different stages.
Figure 3. Ultrasound study of the main vessel after stent implantation, after side branch dilatation, and after kissing balloon inflation. The proximal segment of the stent appears in a blue box, showing lack of apposition (white arrows), which was corrected after kissing balloon inflation. The distal segment at side branch origin appears in a red box; this is distorted after side branch dilatation (note the distortion indicated with yellow arrows on the long axis), and improves after kissing balloon inflation although it does not fully recover its baseline state.
Figure 4. The figure shows individual changes in the stent area at the lower diamond level after each intervention. The lower part of the figure reflects mean (SD) and statistical significance of the differences between means. KB: kissing balloon; SB: side branch.
DISCUSSION
Bifurcated coronary lesions continue to challenge the interventional cardiologist. In recent years, the approach to the SB after implanting a stent in the MV has raised controversy although a conservative attitude (do not dilate if the result is optimal or dilate the SB with a balloon instead of deploying a second stent) apparently offers the best results.
Consequently, in vitro results obtained in series of tests9 show that after SB dilatation a distortion of stent geometry occurs in the lower diamond, immediate to SB origin, and that this distortion is corrected with simultaneous dilatation of 2 balloons. However, in an earlier observational study13 we indicated that distortion produced in the lower diamond in sirolimus-eluting stent implantation did not significantly influence the of restenosis rate at follow-up.
In the present study, we use ultrasound to determine the behavior of the different segments of the stent after balloon dilatation of the SB and subsequent simultaneous inflation of two balloons in KB.
If we analyze the proximal segment of the stent, we find no modification occurs after SB dilatation (baseline 7.3 [1.9] mm2 vs 7.2 [1.9] mm2 after SB dilatation; nonsignificant difference). After KB, a significant increase in stent area occurs (from 7.3 [1.9] mm2 to 9.3 [2.9] mm2; P<.01) and a significant reductuion of the index of symmetry (IS) with respect to the baseline stage and after isolated dilatation of the SB, with a geometrically circular cross-section becoming oval (baseline IS, 0.88; IS after KB, 0.78; P<.001). The inflation of 2 superimposed balloons in the proximal segment of the stent produced the same change in the 23 patients.
In 1 (4%), we found a lack of stent apposition in the proximal segment after implantation and after SB dilatation, but achieved correct apposition after KB (Figure 3). Therefore, KB reduced the chance of bad proximal stent apposition, although this defect was infrequent in our series. However, we should recall the increased area and distortion produced by KB in the era of drug-eluting stents, given they may affect polymer structure with the consequent loss of benefits of this type of stent.
If we analyze the segment immediate to the origin of the SB, we find stent geometry distortion occurs (IS falls from 0.82 to 0.74; P<.01) and area at that level diminishes slightly, from 5.9 (1.2) to 5.23 (1.1) mm2 (P<.05), amounting to a 12% loss in stent area. However, stent distortion in the lower diamond is substantial and ranges from patients with no modification at all (Figure 2) to others with marked distortion (Figure 3). Perhaps the diameter of the balloon used in SB dilatation, the angle or the metallic foot the guidewire passes through and the balloon modify the degree of distortion in the lower diamond, and it would be interesting to determine factors that may influence this in future studies. In our study we found absolutely no correlation between SB angle and the degree of distortion in the lower diamond (r=0.32; P=.1). Moreover, we divided patients into angles >60o and <60o, and analyzed loss of stent area after SB dilatation and the degree of recovery after KB; we found no differences between the 2 groups. In 6 (26%) patients, stent area ranged from 4 to 5 mm2 and only 3 (14%) remained with a luminal area <4 mm2, above which perfusion defects are considered unlikely to.14-18
After KB inflation, stent geometry is not restored (IS after SB dilatation, 0.74; IS after KB, 0.77; P=.168) and complete recovery of stent area does not occur (baseline lower diamond area, 5.9 mm2; lower diamond area after KB, 5.6 mm2; P<.05), gaining 7% of the area lost after SB dilatation. Therefore, although the MV balloon was larger in diameter than the SB balloon and pressure applied during KB was greater in the stent balloon, we were unable to fully restore the distortion produced in the lower diamond. In our study, the segment after SB origin was where less expansion was achieved in relation to the other segments studied. Angiographic analysis of the lesions before treatment shows 20 (87%) patients had disease distal to the bifurcation, which may explain this phenomenon. In patients with a distal stent, as expected, no modification occurred with respect to the baseline situation, given that at this level there was no additional manipulation during the stages of the intervention.
The influence of these strategies, which determine changes in stent geometry, on long-term results is currently unknown. This study only analyzes the acute influence on geometry and the ultrasound measurements of the stent in the main vessel. We did not perform volumetric studies of plaque or IVUS analysis of the SB, which may be considered limitations of the study. In any case, randomized studies are needed to determine the long-term clinical influence of these changes on stent geometry.
CONCLUSIONS
A small distortion in the lower diamond area occurs after SB dilatation and is not fully restored with simultaneous inflation of 2 balloons. Kissing balloon inflation reduces the chance of bad stent apposition, although it produces an increase in area in the proximal segment and a significant loss of IS. Ultrasound is an excellent tool to monitor treatment of bifurcations.
ABBREVIATIONS
IVUS: intravascular ultrasound
KB: kissing balloon
MV: main vessel
SB: side branch
SEE EDITORIAL ON PAGES 911-3
Correspondence:
Dr. J. Suárez de Lezo.
Servicio de Cardiología.
Hospital Universitario de Gran Canaria Dr. Negrín.
Barranco de la Ballena, s/n. 35010 Las Palmas de Gran Canaria. Las Palmas. España.
E-mail: jslht@yahoo.es
Received January 5, 2008.
Accepted for publication May 6, 2008.