A recent meta-analysis of 23 randomized trials has shown that primary angioplasty is associated with a significant reduction in mortality and reinfarction at 30 days.1 These benefits have been explained by a higher rate of TIMI 3 flow achieved by primary angioplasty as compared to thrombolysis. Several reports have shown the safety of transfer for primary angioplasty.2,3 The superiority of primary angioplasty as compared to on-site thrombolysis has been confirmed even when transfer is needed.4 Together, these data have encouraged clinicians to extend primary angioplasty to the vast majority of ST elevation myocardial infarction (STEMI) patients. An increasing number of primary percutaneous coronary intervention (PCI) procedures has been observed in last years across Europe, including Spain.5 However, a larger proportion of mechanical recanalization is not a guarantee of optimal reperfusion. In fact, primary angioplasty requires well-run regional networks, that actually limits a timely application of the procedure to a minority of patients.
Time-Delay to PCI and Survival
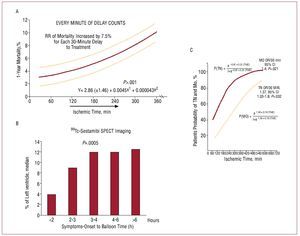
Data from an initial meta-analysis of randomized trials comparing primary angioplasty versus thrombolysis observed a prognostic impact of time-to-treatment only in patients treated with thrombolysis but not with primary angioplasty.6 A major explanation for these results was the time-independence of restoration of TIMI 3 flow with primary angioplasty as compared to thrombolysis. The impact of ischemia time in primary angioplasty was previously analysed by Cannon et al7 by using the database of the National Registry on Myocardial Infarction (NRMI)-2. They observed in a population of 27 080 STEMI patients that, after correction for baseline confounding factors, door-to-balloon time had a significant impact on in-hospital survival. In fact, the strict relationship between ischemia time, the extent of necrosis and survival (as observed in experimental studies)8,9 would be expected to persist despite optimal restoration of epicardial flow (TIMI 3 flow). Supporting these data, several reports have highlighted the importance of ischemia time in primary angioplasty. The Zwolle group analyzed the impact of time-to-treatment as a continuous function in a population of 1791 STEMI patients.10 After correction for baseline confounding factors, they observed that every 30-minute of delay to treatment was associated with an increase in the relative risk of 1-year mortality by 7.5% (Figure 1A). Data from a recent updated meta-analysis of trials comparing primary angioplasty vs thrombolysis,11 have shown similar impact of time-to-treatment for both reperfusion strategies. Several additional studies have been conducted to contribute to explain the prognostic role of ischemia time in primary angioplasty. Our group12 showed in a population of 1072 STEMI patients that time-to-treatment had a significant impact on myocardial perfusion (as evaluated by myocardial blush and ST-segment resolution), enzymatic infarct size and predischarge ejection fraction. Interestingly, these results were confirmed in the analysis restricted to patients with postprocedural TIMI 3 flow. Thus, even though primary angioplasty is able to restore TIMI 3 flow independently from the time of treatment, this can not abrogate the deleterious effects of ischemia time on myocardial necrosis and perfusion. More recently, data from the Enhanced Myocardial Efficacy and removal by Aspiration of Liberalized Debris (EMERALD) trial13 have shown a clear relationship between time-to-treatment, myocardial perfusion and infarct size analysed by scintigraphy. Similar findings have been observed in a pooled analysis of 4 trials performed by Stone et al14 (Figure 1B). A recent study conducted by Tarantini et al15 has evaluated the impact of time-to-treatment on infarct size, estimated for magnetic resonance imaging (MRI). Supporting our previous findings,12 they observed a significant increase in infarct size for every 30 minutes delay to treatment (Figure 1C). Thus, again, "every minute of delay counts." Contrasting with these reports, the Munich group has shown a significant impact of time-to-treatment on infarct size only with thrombolysis but not with primary angioplasty.16 However, the same group has subsequently observed a significant impact of preprocedural TIMI 3 flow (surrogate marker of ischemic time) on scintigraphic infarct size.17
Figure 1. Relationship between time-to-treatment, survival in the Zwolle experience (A, adapted from De Luca G et al,10 and infarct size as evaluated by Technetium SPECT (B, adapted from Stone GW et al14) and cardiac magnetic resonance image (C, adapted from Tarantini G et al15). MO indicates microvascular obstruction; OR, odds ratio; RR, relative risk; TN, transmural necrosis.
In the present issue of the Revista Española de Cardiología, Mingo et al18 analyzed reperfusion delays, their determinants and their prognostic implications among 389 patients with STEMI undergoing primary angioplasty in a Spanish primary PCI center between 2005 and 2007. The median total duration of ischemia was 235 min, with a median door-to-balloon time of 79 min. The door-to-balloon time was shorter when the ambulance service was able to notify the on-duty cardiologist, whereas patients who arrived at the emergency department by their own means had the longest door-to-balloon time (100 min vs 74 min; P<.01). In addition, the door-to-balloon time was significantly longer in diabetic patients, females, non smokers, elderly patients and in case of previous angina. A door-to-balloon time >120 min was associated with higher mortality at 30 days. Despite the limitation of population size, this study further underscores the importance of time-delay to PCI as a adeterminant of mortality among STEMI patients. All these data together, strongly support the need to shorten ischemic time, an aim that can be achieved by early diagnosis, early pharmacological reperfusion before transfer to primary PCI centers.
Pharmacological Facilitation: A Paradise Lost?
In order overcome any delay to mechanical reperfusion, increasing interests have been focused on the strategy of combined pharmacological and mechanical reperfusion (facilitated angioplasty). A large randomized trial (The ASsessment of the Safety and Efficacy of a New Treatment Strategy for Acute Myocardial Infarction [ASSENT 4])19 comparing facilitation by full-dose TNK versus conventional primary angioplasty was stopped when an interim analysis showed a paradoxically higher mortality in the facilitation group as compared to control group at 30-day follow-up. These data may be explained by the significantly higher rates of early reocclusion and re-infarction, potentially accounted by the low-rate of abciximab administration as compared to control group (9.5% vs 50.4%).
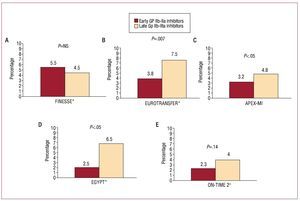
The recent large Facilitated Intervention with Enhanced Reperfusion Speed to Stop Events (FINESSE) trial20 including more than 2400 STEMI patients randomized within 6 hours from symptom onset has shown no benefits with facilitation with both combination therapy or abciximab alone, as compared to periprocedural administration of abciximab (Figure 2A). Several limitations should be taken into account in the interpretation of the results of this trial. First of all, it was prematurely stopped after 4 years, due to slow recruitment. Thus, the very low enrollment rate per center per year certainly lead to a selection bias. In addition, even though the study was focused on facilitation, more than 50% of patients were enrolled in primary PCI centers.
Figure 2. Impact of facilitation with Gp IIb-IIIa inhibitors and survival in randomized trials and registries. * Abciximab; + tirofiban.
Supporting the benefits from early abciximab administration, data from the Eurotransfer registry,21 showed among up to 1000 STEMI patients transferred for primary angioplasty that early abciximab administration improved preprocedural TIMI 3 flow (17.7% vs 8.9%, P<.05) and was independently associated with better 30-day survival (3.8% vs 5.8%, P=.007) (Figure 2B). In addition, in a retrospective analysis from the large Assessment of Pexelizumab in Acute Myocardial Infarction (APEX-MI) trial,22 early glycoprotein IIb-IIIa inhibitors administration was associated with improved preprocedural TIMI 2-3 flow (27.8% vs 21%), postprocedural reperfusion (complete ST-resolution: 53.9% vs 49.5%), and reduced 90-day mortality (3.2% vs 4.8%), as compared to periprocedural administration (Figure 2C).
A recent individual patients' data meta-analysis (including 1662 patients) of randomized trials comparing early versus late administration of Gp IIb-IIIa inhibitors in primary angioplasty23 has demonstrated significant benefits in preprocedural TIMI flow with all the molecules. However, only abciximab was associated with significant benefits in postprocedural TIMI flow, myocardial blush, distal embolization and survival (Figure 2D). Of note, facilitation did not significantly increase the risk of major bleeding complications (3.2% vs 2.9%).
Further evidence of benefits from early Gp IIb-IIIa inhibitors (Tirofiban) has been observed in the Ongoing Tirofiban in Myocardial Infarction Evaluation 2 Trial (On-TIME 2).24 In this study 984 patients were randomized to early, prehospital administration of high-dose tirofiban (25µg/kg bolus followed by a 0.15µg/kg-per-minute maintenance infusion) or placebo. Of note, all patients received early high-dose (600 mg) clopiodgrel adminstration. Early tirofiban was associated with improved pre and postprocedural reperfusion, with reduced mortality (2.3% vs 4.0%, P=.14) (Figure 2E).
Thus, despite the negative results of the FINESSE trial,20 there is evidence of beneficial effects of early Gp IIb-IIIa inhibitors administration that should still be considered a reasonable strategy, especially in high-risk patients and within the first hours from symptom onset.
The Reperfusion of the Future
Despite being less effective in terms of restoration of epicardial flow, especially in late presenters, thrombolysis offers the great advantage of out-of-hospital administration, whereas primary angioplasty requires well-run networks, that actually limit a timely application of the procedure to a minority of patients. Several randomized trials and registries have clearly shown the feasibility and the benefits of out-of-hospital fibrinolysis.25 The Spanish Out-of-Hospital Fibrinolysis Evaluation Project group (PEFEX)26 included 2372 patients with acute infarction attended out-of-hospital between 2001 and 2004. Out-of-hospital fibrinolysis was administered in 19.7% and of note, started within 2 hours from symptom onset in 68% of patients who received it. The authors concluded that out-of-hospital fibrinolysis is performed safely and reduces in-hospital and 1-year mortality in the "real world."
Several randomized trials and registries have recently shown the safety and feasibility of a strategy of early PCI soon after thrombolysis.27-29 In light of these data, it must be recognized that even though mechanical reperfusion has shown benefits in mortality and reinfarction as compared to thrombolysis, early angiography and PCI may certainly reduce the risk of reinfarction and potentially reduce the gap in terms of survival between the two strategies, especially among low-risk patients. The ideal aim of any reperfusion therapy is preventing the infarction.30 While being currently still a dream for the vast majority of STEMI patients, in coming decades large public campaigns and improvements in STEMI networks with higher rates of out-of-hospital diagnosis, may contribute to increase the number of STEMI patients presenting and treatable within the first 2 hours from symptom onset (Golden Hours). And in this contest, I am strongly convinced that we will easily prove the great advantages of a combined reperfusion strategy.
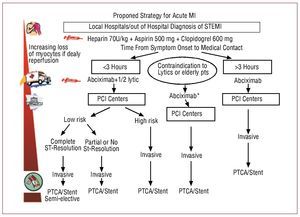
Until further data become available, early pre-hospital pharmacological reperfusion, when the patient's delay to first medical contact is within 3 hours, followed by angiography and angioplasty if thrombolysis is ineffective or in high-risk patients, is a reasonable strategy (Figure 3). In fact, due to unsatisfactory results of stem cell therapy to regenerate myocardium, the only way to save lives is to save as much as possible muscle in the acute phase of coronary occlusions.
Figure 3. Proposed strategy for ST elevation myocardial infarction. *if not contraindicated. MI: myocardial infarction; PCI: percutaneous coronary intervention; PTCA: percutanerous transluminal coronary angioplasty.
SEE ARTICLES ON PAGES 15-22
Correspondence: Dr. Giuseppe De Luca.
Cardiología Intervencionista. División de Cardiología. Hospital Maggiore della Carità. Universidad del piemonte Oriental.
Corso Mazzini, 18. 28100 Novara. Italia.
E-mail: giuspepe.deluca@maggioreosp.novara.it