To the Editor:
We present 2 cases of severe vasospastic angina resistant to intensive medical treatment. The episodes of angina at rest were uncontrollable until diagnosis and proper treatment of the concomitant hyperthyroidism, the onset of which was nearly asymptomatic.
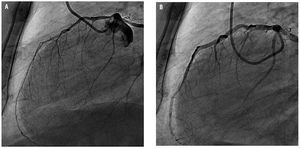
Case 1. The patient was a 75-year-old man with dilated cardiomyopathy and angiographically normal coronary arteries in 2 prior catheterizations. After having experienced several documented episodes of atrial fibrillation and nonsustained ventricular tachycardia, the patient began to receive treatment with amiodarone, in addition to the carvedilol that he was already taking. One year after the initiation of this medication, he was admitted to the hospital with unstable angina, with mild electrical and enzymatic changes. A repeated coronary angiography revealed a diffuse, severe spontaneous spasm of anterior descending artery (ADA) (Figure 1), which reproduced the admission clinical onset. Forty-eight hours later, a level of free thyroxine of 4.82 ng/dL was determined (normal range, 0.89-1.8 ng/dL), whereas thyrotropin was undetectable.
Figure 1. A: diffuse spontaneous spasm of anterior descending coronary artery. B: after administration of intracoronary nitroglycerin.
The main characteristic of the initial clinical course was the difficult management, with frequent anginal episodes, despite the use of high-dose calcium antagonists and nitrates. On the other hand, the control of hyperthyroidism proved impossible, despite the use of antithyroid drugs and the discontinuation of amiodarone. Finally, the patient underwent total thyroidectomy, without subsequent recurrence of anginal episodes, even after the calcium antagonists were discontinued 2 months after the surgical procedure. The duration of the follow-up period was 14 months.
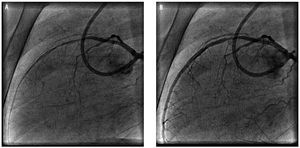
Case 2. A 50-year-old man was brought to our hospital with acute myocardial infarction and precordial ST elevation. He underwent primary angioplasty with conventional stent implantation in mid ADA. Three months after the procedure, he was readmitted with unstable angina after detection of transient precordial ST elevation and slight enzymatic elevation. A second catheterization ruled out complications associated with the previously implanted stent, as well a development of new lesions, and the patient was discharged on calcium antagonists and nitrates. The atenolol that had originally been prescribed was discontinued. Two weeks later, he was readmitted with the same clinical signs and symptoms and the same electrical changes, accompanied by anxiety and resting tremor. Physical examination revealed an arterial pressure of 160/90 mm Hg and a sustained heart rate of 110 beats per minute. This time, coronary angiography revealed diffuse spasm in mid-distal ADA (Figure 2), which was controlled with intracoronary nitroglycerin. The free thyroxine level was 6.41 ng/dL, thyrotropin was undetectable and he exhibited positivity for antithyroid antibodies. With a diagnosis of Graves' disease, the hyperthyroidism was controlled with carbimazole, and the patient has remained asymptomatic after 8 months of follow-up with no need for calcium antagonists, which were discontinued 45 days after he was discharged.
Figure 2. A: severe diffuse spasm in a mid-distal segment of anterior descending coronary artery (distal to a previously implanted stunt). B: after administration of intracoronary nitroglycerin.
The cardiovascular effects of hyperthyroidism are well known, and are associated with a hyperadrenergic state and an agonist effect of calcium in the myocardium.1 Despite the fact that up to 20% of the patients with hyperthyroidism develop angina,2 the documentation of coronary spasm is rare and, to date, there are no published series describing the underlying pathophysiology.3
The present manuscript strengthens the hypothesis concerning causality in the association between hyperthyroidism and vasospastic angina, which, if sufficiently prolonged, can provoke myocardial infarction. Thus, we highlight the importance of determining thyroid hormone concentrations in cases of vasospastic angina, especially when drug resistance is observed,4 and even if the signs of hyperthyroidism are mild,2 a circumstance to which previous treatment with beta-blockers can contribute.
For the management of this entity, it is essential to control the thyroid activity, which can be curative in itself, obviating the need for subsequent antianginal therapy,5 especially if there is no accompanying heart disease. Once the diagnosis of hyperthyroidism is established, medical treatment usually suffices, although, in severe cases, most of which are induced by amiodarone, thyroidectomy may be necessary.6
The authors wish to thank the reviewers for their comments and the suggested modifications, which contributed considerably to improving the manuscript.