Keywords
THE PROBLEM
Refractory angina is a major clinical challenge in contemporary cardiovascular medicine. As therapeutic strategies evolve, there is increased life expectancy for ischemic heart disease with more patients reaching advanced stages. Due to a better understanding of the disease process and technological advances, coronary revascularization by means of coronary by-pass grafting (CABG) and percutaneous coronary interventions (PCI) is now offered to a wide spectrum of high-risk patients. The inception of drug eluting stents in routine clinical practice has reduced the restenosis rates to single digits extending the indications of PCI to poor operative candidates with unprotected left main stenosis or diabetics with diffuse small vessel disease.1 In a similar fashion, more generalized use of major surgical revascularization breakthroughs, such as off-pump CABG and arterial grafts, have resulted in significant improvements in surgical outcomes.2 Despite these advances, a significant proportion of patients with preserved left ventricular ejection fraction and no life-threatening arrhythmias remain symptomatic with severe debilitating angina due to progression of native atherosclerotic disease associated with failure or unfeasibility of revascularization. In a prospective observational study, Hemingway et al showed that at one-year follow-up angina persists in 52% of patients treated with PCI and 40% of those treated with CABG.3 Similar findings were observed in the multicenter international Arterial Revascularization Therapies Study (ARTS) randomized trial, in which only 19% of PCI patients and 38% of CABG patients were free of angina and anti-anginal therapy at 1-year follow-up.4 Moreover, in a meta-analysis of 11 randomized trials comparing PCI with medical therapy in stable patients with chronic coronary artery disease, PCI offered no survival benefit.5
DEFINITION OF REFRACTORY ANGINA
The European Society of Cardiology Joint Study Group has defined refractory angina as a chronic condition (>3 months) characterized by the presence of angina caused by coronary insufficiency in the presence of coronary artery disease which cannot be controlled by a combination of medical therapy, angioplasty and coronary by-pass surgery. The presence of reversible myocardial ischemia should be clinically established to be the cause of the symptoms.6 Multiple clinical studies have shown that the 1-year mortality risk of this group of patients is relatively low.7,8 For example, the sample size estimation in the Impact of Nicorandil in Angina (IONA) trial that enrolled high-risk patients with chronic stable angina was based on the assumption of a 13% event rate after an average of 21 months of follow up in the combined end point of coronary heart disease death, non-fatal myocardial infarction, or unplanned hospital admission for chest pain and an 8% event rate for the composite of coronary heart disease death or non-fatal myocardial infarction (MI).9 The actual all-cause mortality rate at mean follow-up of 1.6 years in the IONA trial was 4.3% in the Nicorandil group and 5% in the placebo group.10 In a more recent study from the Duke Cardiovascular Databank including unselected patients with angina and severe coronary artery disease (¡Ý75% stenosis in 2 or 3 major epicardial vessels), the one-year mortality rate was 11% among patients that were not initially managed with revascularization. Of note, only 9.5% of these patients underwent late revascularization procedures during follow-up.11
Therefore, the relatively moderate to low-event rates in this population suggest that the goal of therapy should be mostly directed at improving quality of life (QOL), provided that the patients do not have additional revascularization opportunities and are already on optimal medical therapy.
GENERAL GOALS OF THERAPY: IMPROVE ADHERENCE TO EVIDENCE-BASED THERAPIES
Aggressive Risk Factor Modification
Similar to other patients with atherosclerotic coronary artery disease, the major determinants of mortality in patients with refractory angina include older age, male gender, low ejection fraction, extent of coronary disease, previous MI, and diabetes mellitus.7 Therefore medical treatments for this patient population should be divided in two groups with separate goals. The first group includes therapies that stabilize atherosclerosis, prevent disease progression, decrease recurrent coronary events, preserve left ventricular function, and improve overall survival. The other set of therapies aim to reduce the anginal threshold by either decreasing oxygen demand or improving hemodynamics to increase myocardial oxygen supply. The first set of goals can be accomplished using appropriate evidence-based medical therapies and aggressive risk factor modification.12 Recommended pharmacological treatments include aspirin, thienopyridines (for patients with aspirin allergy or post-PCI), beta-blockers, nondihydropyridine calcium channel blockers, lipid lowering agents, long acting nitrates, low-intensity anticoagulation, and angiotensin converting enzyme (ACE)-inhibitors. Statin therapy appears to play a crucial role in the management of patients with chronic angina for its effects in decreasing lipid levels and its so called pleiotropic effects. These pleiotropic effects encompass improvements in endothelial dysfunction, increased nitric oxide bioavailability, antioxidant properties, inhibition of inflammatory responses, and stabilization of atherosclerotic plaques.13 In the Reversal of Atherosclerosis with Aggressive Lipid Lowering (REVERSAL) trial, intensive lipid lowering with 80 mg of atorvastatin during 18 months was associated with a significant reduction in progression of atheromatous plaque volume as measured by intravascular ultrasound compared with a moderate regimen consisting of 40 mg of pravastatin.14 The apparent effects observed on plaque stabilization translated into significant clinical benefits in the large multicenter Pravastatin or Atorvastatin Evaluation and Infection Therapy - Thrombolysis In Myocardial Infarction 22 (PROVE-IT - TIMI 22) trial. This study randomized 4,162 patients with acute coronary syndromes (ACS) to the same lipid lowering regimens used in the REVERSAL trial. At a mean follow-up of 24 months, the LDL-c levels in the atorvastatin and pravastatin groups were 62 mg/dL and 92 mg/dL, respectively. This difference was associated with a 16% relative risk reduction in the study primary endpoint (death, myocardial infarction, rehospitalization for unstable angina, revascularization procedures, and stroke) in the group receiving intensive therapy.15 The results of these trials prompted a change in the recommended goal of lipid lowering therapy to LDL-c levels <70 mg dl for high-risk patients 16
Despite the wide availability of clinical management guidelines,12 a number of registries in different settings have shown that proven therapies for ideal candidates are underutilized in real-world clinical practice. The Euro Heart Survey demonstrated that the use of secondary prevention and anti-anginal agents is far from ideal in Europe. This multinational registry enrolled a total 3779 patients with stable angina. Even though all patients in this registry had been evaluated by a cardiologist, the use of aspirin was 78%, statins 48%, beta-blockers 67%, nitrates 61%, calcium channel blockers 27%, and ACE-inhibitors 40%.17 A major reason for not prescribing beta blockers has been attributed to possible side effects. However, there is clear evidence that the general belief that beta-blocker therapy is associated with substantial risks of depressive symptoms, fatigue, and sexual dysfunction is not supported by data from clinical trials.18
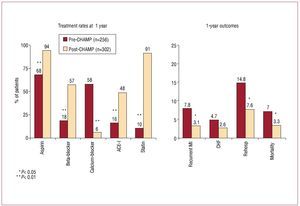
In the United States, the Cardiovascular Hospitalization Atherosclerosis Management Program (CHAMP) aimed at initiating evidence-based therapies such as aspirin, lipid-lowering agents (LDL goal ≤100 mg/dL), beta-blockers, and ACE inhibitors in conjunction with dietary and exercise counseling in patients with established coronary artery disease before hospital discharge. The program was implemented in 1994 and utilized a number of tools designed to facilitate initiation of therapy throughout hospital stay in patients without contraindications. At one year follow-up, patients enrolled in CHAMP showed a substantially higher use of evidence-based medicines, such as aspirin, beta-blockers, statins, and ACE-inhibitors, as compared to patients treated in a period prior to the implementation of the program. Most importantly, as depicted in Figure 1, adherence to recommended therapies resulted in a significant reduction of recurrent ischemic events, heart failure, rehospitalization, and death at 1 year.19
Figure. 1. Adherence to recommended therapies result in improved outcomes. Results from CHAMP.18 ACE-I, indicates angiotensin-converting enzyme inhibitor; CHF, congestive heart failure; MI, myocardial infaction.
Potential Benefits With Optimal Medical Therapy
The Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial evaluated the use of optimal medical therapy vs. percutaneous coronary intervention combined with optimal medical therapy in patients with chronic stable angina. A total of 2287 patients with at least 70% stenosis in one or more vessels were enrolled in the study. The trial aggressively emphasized guideline-driven medical therapy and lifestyle intervention in both treatment arms. The compliance rates at 1, 3, and 5 years were 95%, 95% and 94% for aspirin, 95%, 92%, and 93% for statins, and 89%, 86%, and 86% with beta blockers, respectively. The high compliance rates resulted in a substantial risk factor modification with the achievement of LDL-c levels of <85 mg dl in 70 of patients and achievement blood pressure goals systolic <130 mmhg and diastolic blood pressure <85 mmhg in 65 and 94 of patients respectively it has to be noted that these compliance rates are rarely seen clinical practice there was a significant improvement freedom from anginal symptoms observed the pci group as compared medical treatment at 1 3 years 66 vs 58 72 67 however differences disappeared 5 need for revascularization severe or worsening lower comparison with 21 32 6 i P<.001). The COURAGE trial reported no significant differences in death or non-fatal myocardial infarction at a mean follow-up of 4.6 years between the PCI and optimal medical therapy groups. 20 However, extrapolating the results of the COURAGE trial to clinical practice is problematic for several reasons. Only a 6% of all screened patients were enrolled in the study, therefore the population is not representative. All patients were enrolled after angiography and those with high risk anatomy were excluded creating a selection bias. In addition, the results do not represent contemporary practice due to the very low use of drug-eluting stents of less than 3%.
In a more acute setting, the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines) registry showed that use of evidence-based recommendations continues to be suboptimal, resulting in increased inhospital morbidity and mortality.21
Treatment of Secondary Causes of Angina
Other general therapeutic goals that should not be overlooked include the assessment and correction of anemia, hyperthyroidism, hypoxemia, psychological stress, and tachyarrhythmias. (Table 1) Over the past few years, anemia has emerged as an independent risk factor for adverse cardiovascular outcomes. In the population-based Atherosclerosis Risk in Communities (ARIC) study, the presence of anemia as defined by a hemoglobin value ≤12 g/dL in women and ≤13 g/dL in men was associated with a 40% increase in cardiovascular outcomes defined as definite or probable myocardial infarction, coronary angioplasty, CABG or definite cardiovascular death in 14 410 individuals.22
Re-assess Revascularization Options
In addition to these general measures, the coronary anatomy of patients with refractory angina should be revisited periodically by interventional cardiologists and cardiothoracic surgeons with advanced levels of expertise. As a matter of fact, in clinical practice, revascularization procedures are significantly underused in eligible patients. A multicenter study in Britain showed that 34% and 26% of patients initially treated with medicines were appropriate candidates for revascularization with PCI and CABG, respectively, according to a nine-point scale for specific clinical indications. Over 2.5 years of follow-up, these medically treated patients had higher mortality and a higher prevalence of angina than patients who underwent revascularization. Appropriate candidates for PCI who received medical treatment were more likely to have angina at follow-up (OR=1.97; 95% CI, 1.29-3). Likewise, patients classified as appropriate candidates for CABG but were treated with medical therapy were more likely to have angina at follow-up (OR=3.03; 95% CI, 2.08-4.42). Moreover, these medically-treated CABG-eligible patients were more likely to die or have a nonfatal myocardial infarction during follow-up with a hazard ratio of 4.08 and 95% CI of 2.82-5.93.3 These data are consistent with a recent meta-analysis of 28 prospective randomized trials of patients with non-acute coronary artery disease showing that patients who underwent revascularization by either CABG or PCI had decreased mortality at 1 year (OR=0.74; 95% CI, 0.63-0.88) versus those who were treated with medical therapy alone.23
Drug-eluting stents should be the preferred interventional approach to patients with chronic refractory angina. A random effects and network meta-analysis of 63 trials with a total of 25 388 patients demonstrated a significant reduction in the need for target lesion or vessel revascularization that favored drug eluting stents vs. bare metal stents and drug eluting stents vs. plain balloon angioplasty.24
SPECIFIC GOALS OF THERAPY FOR PATIENTS WITH REFRACTORY ANGINA
Quality of Life
Importance of Quality of Life
By definition, patients diagnosed with refractory angina are those who have failed all standard therapies recommended for the management of chronic stable angina and have coronary anatomy not suitable for revascularization as assessed by a cardiothoracic surgeon and an interventional cardiologist. Therefore, treatments in this situation should be aimed at improving the patient's QOL without compromising quantity of life. The extent of QOL compromise in patients with established coronary artery disease has been well defined in the Randomized Intervention Treatment of Angina (RITA) trial that compared PCI versus CABG in 1011 patients. This study showed that angina persists in approximately 15%-20% of all patients 3 years after a revascularization procedure. In this group of patients, the presence and severity of angina had a marked impact on QOL, affecting all aspects of self-perceived health status, including level of energy, sleep, emotional reactions, social isolation, and physical mobility. In addition, angina has an unfavorable impact on employment status.25 Similar results were observed in the ensuing RITA-2 trial that compared medical therapy versus PCI in 1018 patients. In this study, QOL was affected, not only by the presence of angina, but by the presence of shortness of breath and decreased exercise capacity.26
Even though there are no specific data linking QOL and mortality in patients with refractory angina, it has been demonstrated that QOL determines prognosis in patients with a wide variety of cardiac conditions. In the Studies of Left Ventricular Dysfunction (SOLVD), that enrolled 5025 patients with left ventricular systolic dysfunction, the baseline assessment of QOL, more specifically in the domains of activities of daily living and self-reported general health of the short form health survery-36 (SF-36), independently predicted mortality and rehospitalization in asymptomatic and symptomatic patients.27 A substudy from the Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival (EPHESUS) study showed that health status early after hospital discharge is strongly associated with subsequent 1-year hospitalization and death rates in patients with heart failure post-MI.28 Rumsfeld et al. examined the same question in 2480 post-CABG patients in 14 Veteran Affairs Hospitals. Domains of activities of daily living and general health were independently associated with all-cause mortality at 36 months.29 In a cohort of 945 patients treated at Australian public hospitals for unstable angina, MI, chronic ischemic heart disease, and heart failure, Dixon et al found that subjects with low QOL were 2 times more likely to experience an adverse outcome (death or emergency rehospitalization) at 8 months follow-up, even after adjusting for other prognostic clinical variables, as compared to subjects with high scores of QOL.30 In the large IONA trial including 5126 patients with chronic stable angina, the strongest predictor of cardiac death and/or non-fatal MI was baseline angina class, one of the most important determinants of QOL. The adjusted hazard ratio (95% CI) for cardiac death and/or non-fatal MI in the IONA trial was 2.17 (1.44-3.25) for angina class III-IV as compared with class I. This hazard ratio is greater than those for other classic prognostic factors such as age and left ventricular hypertrophy.31 A systematic review of 34 studies exploring the relevance of QOL on the outcomes of a broad spectrum of cardiovascular conditions encompassing myocardial infarction, status post-revascularization procedures, and congestive heart failure, demonstrated that poor self-reported physical health status, as assessed by disease-specific questionnaires, is independently associated with increased mortality and higher rehospitalization rates.32
Improving Quality of Life
QOL can be improved by just implementing standardized management strategies. As demonstrated by Benson and McCallie,33 there is a placebo effect associated with various treatments or procedures. More contemporary evidence supporting this notion comes from the RITA-2 trial in which a significant proportion of patients randomized to the medical arm experienced a significant improvement in ratings of physical role functioning, emotional role functioning, social functioning, pain, and mental health at 3-year follow-up.26 This "placebo" effect was further demonstrated in the Direct Myocardial Laser Revascularization (DMR) in Regeneration of Endomyocardial Channels Trial (DIRECT) trial, which randomized 298 patients with severe refractory angina to low or high dose direct myocardial revascularization with laser or a sham procedure in a blinded fashion. Patients undergoing the sham procedure experienced significant improvements at 6 and 12 months in QOL, exercise duration, time to 1 mm ST-segment depression, and angina severity.34
On the other hand, the severity of angina, degree of disability, and treatment satisfaction may not directly correlate with the severity and extent of coronary artery disease. Increased levels of anxiety, depression, and psychological stress play a major role in patients with refractory angina. A number of studies have shown that response to therapy depends more on psychological features such as anxiety, depression, neuroticism, and hypochondrias rather than extent and degree of coronary disease. Misconceptions about the nature of anginal episodes may further contribute to the increased levels of stress in this patient population.35-38 Therefore, education, coaching, optimal implementation of secondary prevention therapies and exercise programs are key elements in the management of patients with refractory angina. The implementation of a dedicated patient-centered multidisciplinary program for the management of refractory angina in the United Kingdom was associated with significant improvements in QOL. This program involves extensive education, optimization of medical therapies, rehabilitation, and other specific therapies. Patients, relatives, and physicians were able to define realistic goals and tailor therapies accordingly based on full knowledge of all available and relevant therapeutic options. The one-year results of this program were evaluated in a cohort of 66 patients using three instruments including the abbreviated short form health survey (SF-12), the Seattle angina questionnaire, and the hospital and depression scale. All patients received outpatient counseling, cardiac rehabilitation, and cognitive behavior therapy while 64% received transcutaneous nerve stimulation and 14% received temporary sympathectomy. At one year, patients enrolled in the program experienced clinically significant improvements in angina stability, angina frequency, treatment satisfaction, and QOL. In addition, levels of anxiety and depression were reduced by 38%.39
Cardiac Rehabilitation
Cardiac rehabilitation is an important component in the management of patients with chronic ischemia that includes exercise therapy as a key element in its therapeutic approach. The major goal of cardiac rehabilitation programs is to optimize functional capacity, improve QOL, and slow or reverse the progression of the underlying pathophysiologic process. A meta-analysis of 48 trials including 8,940 patients showed a significant reduction in all-cause (OR=0.80; 95% CI, 0.68-0.93) and cardiac mortality (OR=0.74; 95% CI, 0.61-0.96) among patients enrolled cardiac rehabilitation in comparison with patient managed with usual medical therapy, but failed to show any significant difference in rates of non-fatal myocardial infarction, revascularization, or health-related QOL.40 Despite the evidence supporting its use, cardiac rehabilitation continues to be substantially underutilized in the elderly, females, non-white minorities, and Medicaid beneficiaries.41
Other strategies such as the wide implementation of nurse-led clinics to promote medical and lifestyle aspects of secondary prevention have also been tested in patients with established coronary artery disease. A study conducted in Northeast Scotland included 1173 patients, 50% of them with chronic angina, and showed that nurse-led clinics were associated with significant improvements in functional status and less hospital admissions at 1-year. However, angina, depression, and anxiety scores were marginally affected.42 At 4 years, patients who attended the secondary prevention clinics not only achieved better control of their risk factors but also obtained a significant survival benefit. Cumulative death rates were 14.5% for the intervention group and 18.9% for the control group (P=.038) and the relative risk for total mortality was 0.78 (95% CI, 0.61-0.99). Attendance to the clinics was associated with better adherence to risk factor modification measures including aspirin use, blood pressure control, lipid management, and exercise.43 The optimal compliance rates in the COURAGE trial and the use of nurse practitioners as a means of close supervision also highlights the role of optimal medical management and risk factor modification in patients with chronic stable angina.20
Achieving Quantifiable Goals of Therapy
Novel Anti-Anginal Agents
Most clinical trials testing pharmacological agents or devices for refractory angina are designed on the basis of more quantifiable goals than QOL. Common endpoints used in testing these therapies include frequency of angina attacks, use of short-acting nitrates, and exercise-testing parameters such as exercise duration, time to onset of angina, and time to 1-mm ST-depression. However, these endpoints may not be evaluable in an older and debilitated population with multiple comorbidities restricted in the capacity to adequately exercise in a treadmill. As depicted in Table 2, specific novel anti-anginal therapies including ranolazine, ivabradine, and nicorandil have been able to achieve improvements in most of these endpoints in moderate-sized clinical trials.8,44-48 Ranolazine is the only drug approved by the Food and Drug Administration (FDA) in this group and has been further tested in patients presenting with non-ST elevation ACS in the placebo-controlled "Metabolic Efficiency with Ranolazine for Less Ischemia in Non-ST-segment elevation acute coronary syndromes - Thrombolysis in Myocardial Infarction 36" (MERLIN-TIMI 36) study. In a subgroup analysis including 3565 patients with prior chronic angina, the use of ranolazine was associated with a greater reduction in worsening angina (HR=0.77; 95% CI, 0.59-1; P=.048), a reduction in the intensification of anti-anginal therapy (HR=0.77; 95% CI, 0.64-0.92; P=.005), and increased exercise duration (514 vs 482 seconds; P=.002) at 8 months.48
Non-Invasive Anti-anginal Therapies
Non-invasive methods such as enhanced external counterpulsation (EECP) and transcutaneous electrical nerve stimulation have also shown similar results in terms of quantifiable endpoints.49,50 In a Scandinavian centre, 55 patients with chronic refractory angina were treated with EECP. Anginal symptoms were significantly improved in those patients with Canadian cardiovascular class III and class IV but not in those with class II at one year.51 The International EECP Patient Registry, with a total of 1427 patients, was used to study the effects of EECP on angina and showed very similar results with decreased anginal symptoms in those patients with Canadian class III and IV angina.52
Invasive Anti-anginal Therapies
Satisfactory results have been obtained using neuromodulation through spinal cord stimulation (SCS). During SCS an electrical current is applied to the spinal cord with an electrode placed in the epidural space between C7 and T1. The electrode is connected to a pulse generator located in a subcutaneous pocket in the anterior abdominal wall. An observational study using SCS in 517 refractory angina patients showed significant improvement in angina class.7 SCS has been further tested in a randomized trial versus CABG, assessing frequency of angina attacks, use of short-acting nitrates, and time to ischemia in exercise testing. The results showed that CABG (n=51) and SCS (n=53) had similar efficacy in reducing nitrate consumption and frequency of angina attacks. However, CABG was associated with better exercise capacity and less ST-segment depression at maximum workload.53
In contrast with non-invasive therapies and SCS, disappointing results were obtained with gene therapy and percutaneous myocardial laser revascularization (PMLR) and transmyocardial laser revascularization (TMLR). Despite promising preliminary data in small sample size trials, larger randomized studies showed no benefit associated with the use of these therapies.34,54,55
Scintigraphic endpoints have also been used in clinical trials testing therapies for refractory angina. However, scintigraphic endpoints seem to be less consistent than exercise capacity or symptoms of angina. Most studies using scintigraphic endpoints are smaller trials that provide preliminary data for larger studies using symptom and/or exercise endpoints. In general, myocardial perfusion is evaluated with a radionuclide scintigraphy at baseline and at different timepoints after starting a new therapy for refractory angina. Scintigraphic parameters include tracer uptake, magnitude of reversibility, average thickening fraction, and left ventricular ejection fraction. Even though multiple observational retrospective studies examining the effects of EECP have shown significant resolution of perfusion defects, a more recent prospective multicenter study did not show any improvements in scintigraphic parameters despite significant improvements in angina attacks and exercise capacity.56 Similar observations were reported with other therapeutic modalities such as TMLR, PMLR, and medical therapies. These results suggest that improvements in exercise capacity and symptom relief may not be directly related to enhanced myocardial perfusion.
Recent innovative studies are evaluating stem cell therapy in patients with refractory angina and chronic myocardial ischemia. Study endpoints include subjective and objective measures, such as severity of angina and scintigraphic assessments. A Phase I/IIA double blind randomized controlled trial explored the use of autologous CD34+ stem cells, inserted via intramyocardial, transendocardial injections, in 24 patients with Canadian Cardiovascular Society (CCS) class 3 or 4 angina who were managed with optimal medical treatment and were not candidates for mechanical revascularization. Patients who received stem cell injections experienced a greater reduction of symptoms, nitroglycerin use, and had slightly improved exercise time at 3 and 6 months. However, single-photon emission computed tomography imaging showed inconsistent findings with improvements in both cell-treated and control groups with a slightly greater improvement in the visually estimated score in the cell-treated group.57
A randomized controlled trial in the Netherlands evaluated the use of imtramyocardial bone marrow stem cell injection in 50 patients with severe angina despite optimal medical therapy. At 3 months, stress myocardial perfusion imaging, left ventricular ejection fraction, CCS angina class, and Seattle Angina questionnaire were examined. The summed scintigraphic score improved in the bone marrow cell group from 23.5 to 20.1 (P<.001) versus 24.8 to 23.7 (P=.004) in the placebo group. The bone marrow group also had a 3% absolute increase in left ventricular ejection fraction, evaluated by magnetic resonance imaging, at 3 months versus the placebo group that showed no significant difference in left ventricular ejection fraction. CCS angina score in the bone marrow group also significantly improved as compared to no improvement in the placebo group (-0.79; 95% CI,-1.1 to -0.48). These improvements were also evident in the QOL score as evaluated by the Seattle Angina questionnaire.58
CONCLUSIONS
Refractory angina is a debilitating condition and its treatment remains problematic. Due to advances in revascularization strategies and medical therapies the survival of patients with atherosclerotic coronary artery disease has improved substantially over the past two decades. In fact, the 1-year survival rate of patients with refractory angina is approximately 90%. The goals of therapy need to be individualized in each case and expectations should be discussed with the patients and their families. The coronary anatomy should be reviewed periodically by interventional cardiologists and cardiothoracic surgeons to confirm whether or not revascularization is an option. Assuring adherence to evidence-based therapies and correction of precipitating factors is crucial for the stabilization of atherosclerosis, which in turn may result in a survival benefit. Therapies that reduce the anginal threshold by decreasing oxygen demand or improving hemodynamics also play an important role. Management strategies aimed at improving QOL are fundamental in the management of these patients and may also be associated with a survival benefit. These strategies include psychological support, education, and exercise programs (cardiac rehabilitation). More specific therapies such as EECP, transcutaneous electrical nerve stimulation, and SCS also have a place in the treatment of these patients keeping in mind that there is a significant "placebo" effect with each one of these specific therapies. Regenerative medicine with use of stem cells is currently a very active research area and may have an important role in the recovery of these patients.
ACKNOWLEDGMENTS
The authors acknowledge the excellent editorial assistance of Eric Scot Shaw in the preparation of this manuscript.
Correspondence: Dr M. G. Cohen.
University of Miami Hospital,
1400 N.W. 12th Avenue, Room 1179, Miami, FL 33136, USA
E-mail: mgcohen@med.miami.edu