The triage of patients presenting to the emergency department (ED) with acute chest pain remains challenging despite application of several management strategies. Of all patients presenting with acute chest pain, nearly 75% are diagnosed with non-cardiac or non-ischemic cardiac problems and less than 20% of the remaining meet criteria for acute coronary syndromes.1-3 Although patients with acute coronary syndromes as well as those at very low probability for coronary ischemia can generally be identified and triaged in an expedited manner, those with low-to-intermediate risk for ongoing coronary ischemia present a diagnostic dilemma. Often, these patients are admitted (to the hospital or specialized "chest pain" units) for extended observation and varying diagnostic strategies with serial electrocardiograms, cardiac enzymes and often, noninvasive stress testing.4-6 Myocardial perfusion imaging with single-photon emission cardiac tomography (with and without stress), and stress echocardiography have been extensively applied in this setting. Both imaging modalities have been shown to provide incremental information for clinical risk stratification in these patients.7,8 However, the approach of evaluation of acute chest pain patients with extended observation and ancillary testing is expensive and time consuming, incurring an estimated cost of $10 to $12 billion annually in the United States alone.4,9 Moreover, 2%-8% of patients with acute coronary syndromes are still misdiagnosed and inappropriately discharged home, with a doubling of mortality3 and resulting in the majority of malpractice suits against ED physicians.10
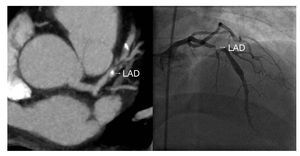
Coronary computed tomography angiography (CCTA) has been rapidly embraced for evaluation of coronary artery disease (CAD) in patients with acute chest pain. The accuracy of CCTA for assessing the presence and severity of CAD has been compared extensively to invasive angiography, in more than 2000 patients.11 The diagnostic performance of CCTA is somewhat dependent on the prevalence of CAD with higher accuracy (sensitivity, specificity, positive predictive value, and negative predictive value were 95%, 83%, 64%, and 99%, respectively) noted in patients with no known prior CAD.12,13 On the other hand, the quantitative severity of lesions on CCTA do not directly translate into stenosis grade on invasive angiography, possibly because CCTA has much greater flexibility in assessing lesions from multiple viewing angles with the extent of disease in diffusely diseased segments being easily discerned. Overall good correlation is noted with invasive angiography (average Pearson correlation, r=0.72) (Figure 1), but with considerable standard deviation, which limits its quantitative accuracy.14
Figure 1. CCTA in a 52-year old male presenting with acute chest pain to the emergency department. Electrocardiogram and cardiac enzymes were unremarkable. CCTA revealed a high-grade lesion in the proximal LAD (left panel). He was taken emergently to cardiac catheterization, where CCTA findings were confirmed (right panel). Successful percutaneous intervention resulted in excellent angiographic results. CCTA, coronary computed tomography angiography; LAD, left anterior descending coronary artery.
The high negative predictive value and speed of CCTA have made it attractive for use in rapid triage of acute chest pain patients. A highly significant decrease in time-to-triage of low-to-intermediate risk patients has been previously reported by our group (with an average time to diagnosis of 3.4 hours as compared to 15.0 hours for standard of care that included myocardial perfusion imaging), with no test complications, subsequent diagnosis of CAD or major adverse cardiac events during 6 months of follow-up.15 Other single-center trials have also demonstrated safety of CCTA in early discharge of patients from the ED with no adverse events.16 In the recently published Rule Out Myocardial Infarction using Computer Assisted Tomography (ROMICAT) study, Hoffmann et al reported 100% negative predictive value of CCTA for subsequent diagnosis of acute coronary syndromes or major adverse cardiac events.17 Importantly, the presence of atherosclerotic plaque as well as severity of stenosis predicted acute coronary syndrome ACS independent of coronary risk factors or the thrombolysis in myocardial infarction (TIMI) risk score used commonly for clinical risk stratification.
In addition to the expedited triage of ED patients with chest pain, an important consideration for use of this technology is the decrease in absolute costs. In our study, this approach resulted in a decrease in cost by 16% ($1586 in the CCTA arm compared to $1872 in the standard of care arm).15 In a study by Rubinshtein et al, the need for hospitalization among acute chest pain patients was shown to decrease by nearly 50% with a CCTA-based approach.18 The 16-center Coronary Computed Tomography for Systematic Triage of Acute Chest Pain Patients to Treatment (CT-STAT) trial recently completed enrollment, randomizing 750 low-to-intermediate risk patients to the standard of care arm (including stress myocardial perfusion imaging) or CCTA. The study is designed to compare the safety, accuracy, and time-to-diagnosis as well as cost-effectiveness of these 2 triage strategies.
Non-Coronary and Non-Cardiac Findings on CCTA
Nearly 1 in 6 patients without CAD detected on CCTA have noncardiac findings that could explain their presenting symptoms.19 A routine CCTA examination should include examination and reporting of all pathology within the cardiac field of view, offering the opportunity to define pericardial, myocardial, valvular, and vascular structural abnormalities, as well a functional abnormalities using cine-CT displays. The three-dimension data covered by the standard CCTA examination provides access to vascular and non-cardiovascular thoracic and upper abdominal anatomy, including the mediastiunum, hilum, trachea and bronchi, lung parenchyma, pleura, chest wall, esophagus, stomach, spleen, and colon. In particular, CCTA, as compared to stress testing, provides the advantage of being able to simultaneously examine other non-cardiac structures such as the aorta and pulmonary arteries, to rule out the 3 most potentially fatal causes of chest pain: CAD, acute aortic dissection, and pulmonary embolism. The major technical challenge of a "triple rule out" scan protocol is to obtain high and consistent contrast intensity in all 3 vascular beds, mandating a carefully tailored imaging and injection protocol. A "tri-phasic" injection protocol and a caudalcranial scan acquisition have been shown to provide good opacification of the coronary and pulmonary arteries and the aorta.20
Although the "triple rule-out" protocol can diagnose a myriad of cardiac and non-cardiac pathology, it should not be used unless there is a high index of suspicion for 2 of the 3 pathologies in question, since prior studies of patients with acute chest pain have shown that the incidence of "occult" pulmonary embolism or aortic dissection in patients without suggestive signs or symptoms is very low.21 Additionally, radiation dose is directly proportional to the scan length, increasing by 30%-50% in "triple rule-out" scans. Novel 320-slice CT scanners may result in much lower radiation doses with the triple rule-out protocol.22
Barriers for CCTA Use in the Ed
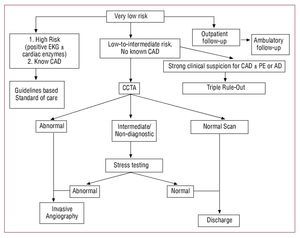
CCTA has several important limitations that affect its usefulness in the triage of ED patients with acute chest pain. Clinical presentation and risk stratification of patients presenting with acute chest pain is of paramount importance in selecting patients for CCTA (Figure 2). Even with the new generation 64-slice CT scanners, image quality is inversely correlated with heart rate, requiring premedication with beta-blockers to lower heart rates during acquisition in most patients. Nearly 15% of ED patients have some contraindication to beta-blockers, rendering them unsuitable for CCTA.21 Dual-source or other novel scanners may obviate the need for beta-blocker administration in such patients. In addition, because ECG-gating is critical to coronary imaging, any arrhythmias, ectopy or ECG artifacts result in degradation of image quality. Currently, CCTA in atrial fibrillation is a more difficult examination and requires specialized acquisition and reconstruction protocols. New scanner improvements may make acquisition possible within a single heartbeat, making high quality results during arrhythmias consistently available.
Figure 2. Suggested algorithm for CCTA based protocol in evaluation of acute chest pain patients in the emergency department. AD, acute aortic dissection; CAD: coronary artery disease; CCTA, coronary computed tomography angiography; EKG, electrocardiogram; PE, pulmonary embolism.
Extensive coronary calcification that obscures the coronary lumen may substantially limit analysis of segments or even entire arteries by CCTA. Thus, this technique may be of limited application in patients with a high likelihood of significant coronary calcification, such as the elderly or in patients with prior calcium scores >1000 Agatston units.23 Similarly, patients with pre-existing CAD often have extensive coronary calcifications, known intermediate severity coronary lesions, and/or coronary stents with resultant metal artifacts or prior coronary bypass grafting with extensively calcified native vessels and small caliber distal coronary arteries. In this scenario, the question is not the presence or extent of CAD, but its role in the patient's current symptoms of ischemia. This question is better answered by physiologic, rather than anatomic testing.
Obesity increases radiation scatter within the patient's body and consequently degrades image quality due to a reduction of the signal-to-noise ratio. All of these factors diminish the diagnostic accuracy of CCTA, rendering it probably inappropriate for ED triage in patients with a body mass index over 39 kg/m2. Technical advances exist on dual source scanners that have extended the capability of CCTA to morbidly obese patients with good image quality.23
Radiation exposure is a significant consideration in CCTA, resulting in a non-negligible lifetime attributable risk of cancer and this should be weighed against potential benefits, especially in sensitive populations such as women under 45 years of age.23 Dose reduction techniques and avoidance of technical errors is of paramount importance. Radiation dose can be modified by adjusting the tube voltage, tube current, pitch, and scan time. Further reduction in radiation dose can be accomplished by utilizing a lower tube voltage (for example, 100 kV in non-obese patients).23 Some groups have recently investigated the use of "prospective" gating only (in which data is acquired for a short segment in diastole only) for patients with low and very stable heart rate; yielding total radiation doses less than 5 mSv, with no compromise in image quality compared to retrospective gating.24
An important consideration is that CCTA, just as with invasive angiography, delineates anatomy only and can therefore only infer the impact of any given luminal narrowing on coronary blood flow. Anatomical assessment of the coronaries is most clinically reassuring when the vessels are normal or have minimal disease, and may reliably predict the physiological significance of very severe stenoses. However, anatomic data by itself is limited in assessing the physiological significance of stenoses of "intermediate severity" (30%-70% diameter stenoses). Whether such anatomically defined lesions are responsible for symptoms, or are "innocent bystanders" requires adjudication by physiological determination of coronary blood flow.25
A team approach is required to implement a CCTA-based ED triage protocol. ED physicians and expert CCTA interpreters must be well educated regarding the application and inherent limitations of CCTA. Patient selection must be rigorous to avoid the potential for over-utilization of CCTA and to avoid unnecessary radiation.
Future directions
Atherosclerosis of the coronary arteries is a dynamic process, with stable disease interspersed with periods of instability and rapid increase in plaque volume.26 Additionally, the majority of acute myocardial infarctions result from atherosclerotic plaques previously demonstrating stenoses <50% on angiography.27 Characterization of plaque in addition to severity, particularly in patients with chest pain may be important. One study examining patients presenting with acute coronary syndromes reported plaque morphology similar to that seen on invasive angiography, with characteristics of plaque disruption including lesion haziness, positive remodeling, ulceration, and intraplaque contrast penetration.28 Hoffmann et al have demonstrated higher plaque burden and remodeling in patients with acute coronary syndromes compared to those with stable angina.29 Currently, however, plaque characterization is limited to images of very high quality and may not be applicable in average clinical practice.
Cardiac CT also has potential for evaluation of myocardial perfusion and viability. Quantitative analysis of myocardial perfusion is based primarily on differences in CT attenuation values and the ability to adequately assess areas of myocardial hypoattenuation, indicative of diminished myocardial perfusion.30 This application can be of use in ED patients with chest pain and lesions of "intermediate" severity and the possibility of a "one-stop shop."
Conclusion
Historically, ED evaluation of acute chest pain patients has entailed lengthy and expensive diagnostic testing. Preliminary research suggests that the application of CCTA can potentially revolutionize the evaluation of appropriately selected patients. Multicenter trials are in progress to determine if these promising single center studies can be confirmed. Although the future of this technology holds great promise, the limitations and risks, particularly that of radiation exposure must be considered carefully prior to selection of patients for CCTA.
Correspondence: Gilbert L. Raff, MD, FACC
William Beaumont Hospital, 3601 W. 13 Mile Road, Royal Oak, MI 48073 United States
E-mail: GRaff@beaumont.edu