The RECALCAR project (Spanish acronym for Resources and Quality in Cardiology Units) uses 2 data sources: a survey of cardiology units and an analysis of the Minimum Basic Data set of all hospital discharges of the Spanish National Health System. From 2011 to 2014, there was marked stability in all indicators of the availability, utilization, and productivity of cardiology units. There was significant variability between units and between the health services of the autonomous communities. There was poor implementation of process management (only 14% of the units) and scarce development of health care networks (17%). Structured cardiology units tended to have better results, in terms of both quality and efficiency. No significant differences were found between the different types of unit in the mean length of stay (5.5±1.1 days) or the ratio between successive and first consultations (2:1). The mean discharge rate was 5/1000 inhabitants/y and the mean rate of initial consultations was 16±4/1000 inhabitants/y. No duty or on-call cardiologist was available in 30% of cardiology units with 24 or more beds; of these, no critical care beds were available in 45%. Our findings support the recommendation to regionalize cardiology care and to promote the development of cardiology unit networks.
Keywords
In developed Western countries, there is a marked trend toward medical professionalism and self-regulation.1–3 The SEC (Spanish acronym for the Spanish Society of Cardiology) has conducted several studies on cardiovascular disease health care,4,5 and, in collaboration with the Ministry of Health, Social Services, and Equality (MHSSE) has published the standards and recommendations document for cardiovascular care units.6 In line with this collaborative effort, the SEC Strategic Plan 2011-2016 included the aim of “Developing a policy of collaboration with Public Administration to promote continuous improvement in the quality of cardiovascular disease health care”. The INCARDIO position paper was published in 2015, with the aim of defining quality markers in cardiology.7,8 Currently, the SEC is conducting the SEC-Quality project9 as an institutional strategic plan that encompasses several subprojects for continuous improvement in the quality of cardiovascular disease health care. One of these subprojects is the “sources and Quality in Cardiology” RECALCAR) project, which uses 2 data sources: a) the resources, activity, and quality of cardiology units (CU) survey, which comprises the registry of CUs accredited by the MHSSE as of interest to the Spanish National Health Service (NHS); and b) an analysis of the Minimum Basic Data Set (MBDS) database of the NHS.
It is increasingly clear that the organizational and administrative aspects of health care are relevant to the quality of health care, patient safety, and efficiency.10,11 Continuous improvement in any organization, including health services, is based on the systematic recording and careful interpretation of the data obtained.12–14 It should be mandatory to record the most relevant aspects of health care activity in order to provide a sound basis for improvements. These aspects form the basis of the RECALCAR project.
Health care policy decision-making should be based on evidence-based clinical, organizational, and administrative criteria. However, there is a striking lack of evidence-based scientific data on the actual operation of health services. Recognition of the need to provide evidence for health policy decision-making has led many developed countries to make a significant investment in comparative effectiveness research.15 Although this is a very challenging situation, there is growing interest in health services outcomes research, especially in the area of health service provision.16–18 Outcomes research is also used to compare health services19 and performance between countries.20 Mortality and readmission are the most widely used outcomes measures, which use risk adjustment methods to ensure that services are comparable. Centers for Medicare and Medicaid Services (CMS) use administrative database outcomes measures to guide center funding and provide patients with the information they need to take informed decisions.21 RECALCAR uses analysis of data from administrative data sources, such as the MBDS, and from the association between structure and process (survey) data and outcomes (MBDS) as an outcomes research method in cardiac health care and as a very useful instrument to propose evidence-based policies.
This article summarizes the RECALCAR project and describes its most important findings in relation to NHS cardiac health care outcomes.
DESCRIPTION OF THE RECALCAR REGISTRYThe RECALCAR registry is based on a survey of NHS CUs (2011 to 2014). The registry included CUs with more than 100 beds in general acute care hospitals. Therefore, hospitals not included in groups 1 to 5 of the MHSSE classification were excluded. Data were collected using an ad hoc questionnaire. Missing information was obtained from the records of the Spanish Cardiac Catheterization and Coronary Intervention Registry22 and the Spanish Ablation Catheter Registry.23
Types of UnitsBased on experience gained from the registry, CUs are classified into 5 groups (Table 1). Type 1 CUs (without a structured cardiology unit) remain within the scope of the registry by providing valuable information on cardiology-related activity in hospitals serving small populations (clusters 1 and 2 of the MHSSE).
Classification of Units by Type (RECALCAR Survey)
| Typology | Characteristics |
|---|---|
| 1 | Units without hospital beds assigned to cardiology |
| 2 | Units with hospital beds specifically assigned to cardiology, without a cardiac catheterization laboratory |
| 3 | Units with hospital beds assigned to cardiology, with a cardiac catheterization laboratory, without an in-hospital cardiovascular surgery unit |
| 4 | Units with hospital beds assigned to cardiology, with an in-hospital cardiac catheterization laboratory and cardiovascular surgery unit |
| 5 | Units without beds assigned to cardiology with cardiac catheterization activity and/or cardiovascular surgery |
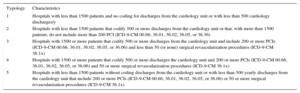
Because the RECALCALCAR survey did not classify all the CUs, MBDS data were used to develop a classification of all hospitals (Table 2).
Classification of Units by Type (MBDS_CAR)
| Typology | Characteristics |
|---|---|
| 1 | Hospitals with less than 1500 patients and no coding for discharges from the cardiology unit or with less than 500 cardiology discharges/y |
| 2 | Hospitals with less than 1500 patients that codify 500 or more discharges from the cardiology unit or that, with more than 1500 patients, do not include more than 200 PCI (ICD-9-CM 00.66, 36.01, 36.02, 36.05, or 36.36) |
| 3 | Hospitals with 1500 or more patients that codify 500 or more discharges from the cardiology unit and include 200 or more PCIs (ICD-9-CM 00.66, 36.01, 36.02, 36.05, or 36.06) and less than 50 (or none) surgical revascularization procedures (ICD-9-CM 36.1x) |
| 4 | Hospitals with 1500 or more patients that codify 500 or more discharges the cardiology unit and 200 or more PCIs (ICD-9-CM 00.66, 36.01, 36.02, 36.05, or 36.06) and 50 or more surgical revascularization procedures (ICD-9-CM 36.1x) |
| 5 | Hospitals with less than 1500 patients without coding discharges from the cardiology unit or with less than 500 yearly discharges from the cardiology unit that include 200 or more PCIs (ICD-9-CM 00.66, 36.01, 36.02, 36.05, or 36.06) or 50 or more surgical revascularization procedures (ICD-9-CM 36.1x) |
ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; PCI, percutaneous coronary intervention; pPCI, primary PCI.
The MHSSE provides the SEC with the MBDS database (MBDS_CAR) for the RECALCAR project. The MBDS_CAR comprises hospital discharges coded according to the IDC-9-CM (International Classification of Diseases, Ninth Revision, Clinical Modification) in NHS hospitals with a principal diagnosis of “cardiovascular disease” (CVD).6 In the absence of this diagnosis, it includes in the process fields coronary interventionists or, in the absence of a principal diagnosis or interventional procedures related to the 2 preceding points, discharges by a cardiology or cardiac surgery unit. The MBDS _CAR comprises approximately 400 000 hospital discharges per year of which approximately 350 000 have a principal diagnosis of CVD. Between 2007 and 2014, the MBDS_CAR provided data on 3 183 370 hospital discharges.
Concordance Between Classifications by Type of UnitThere is a high level of agreement between the RECALCAR survey (Table 1) and the MBDS (Table 2) on the classification of CUs (quadratric weighted kappa = 0.92; 95% confidence interval, 0.86-0.99; P < .0001).
Risk Adjustment and Statistical AnalysisThe multivariable logistic regression risk adjustment model used by RECALCAR has been described in other studies,24 and is based on the methodology developed by Krumholz for the CMS,25–27 adapted to the characteristics of the MBDS_CAR. Unlike the CMS methodology, RECALCAR calculates hospital mortality instead of overall 30-day mortality; only CVD readmissions are estimated because the MHSSE does not provide the complete database. Discharges with a secondary diagnosis (such as shock) cannot be eliminated because the current NHS MBDS does not record them. Risk factors and their coefficients that are positively entered in the adjustment models are derived from those in the MBDS_CAR database.
Regarding the survey data presented in this article, qualitative variables are expressed as frequency distributions (number of cases and percentage) and quantitative variables are expressed as mean, median, and standard deviation. The chi-square test was used to analyze difference in proportions of qualitative variables. The Student t test was used analyze the normality of the distribution and homogeneity of variance of quantitative variables or, if needed, the Mann-Whitney U test for comparisons between 2 groups and the analysis of variance with the Bonferroni correction, and the Kruskal-Wallis test or the median test for comparisons of 3 or more groups. In all tests, a P value of < .05 was used as a cutoff for statistical significance. All data were analyzed using the SPSS 21.0 software package.
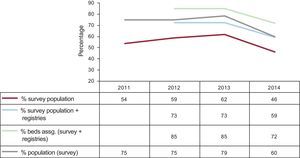
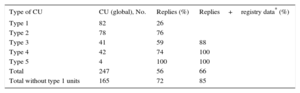
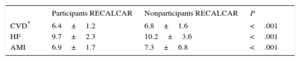
MAIN FINDINGS OF RECALCARDuring the study period, the registry obtained replies from between 96 and 129 CUs (46%-62% of the CUs identified, respectively), which increased to between 59% and 76% when data were included from the registries of the scientific working groups. Replies were obtained from between 60% and 79% of the units belonging to the hospitals serving the population (possibly the best measure of coverage in the survey), whereas the percentage was between 72% and 85% of the population when data on assigned beds were included (Figure). A higher percentage of replies were provided by type 3 and 4 CUs than by type 1 and 2 CUs (Table 3). When the strict criterion of the definition of a CU was applied (excluding type 1 CUs), 72% of CUs replied to the survey in 2015, representing a high participation rate for this type of study. The representativeness of the participating units critically depended on their number. The lowest participation rate was in 2015. The CUs that replied to the survey in that year tended to have better indicators, even within the more homogeneous groups (type 3 and 4 units; Table 4).
Trend in the number of replies and the representativeness of the sample. % survey population, percentage of cardiology units with information on the total number of identified hospitals; % survey population + registry, percentage of cardiology units with information on the total number of hospitals identified plus information from the registries of the scientific sections; % beds assg, percentage of assigned beds in hospitals with units that reported on the total number of assigned beds in identified hospitals (source: National Catalogue of Hospitals28); % population (survey), percentage of the population in the catchment area of hospitals with units that reported on the total population covered by the Spanish National Health System (source: RECALCAR survey29).
Replies to the RECALCAR Survey by Type of Unit in 2015 (Data for 2014)
| Type of CU | CU (global), No. | Replies (%) | Replies+registry data* (%) |
|---|---|---|---|
| Type 1 | 82 | 26 | |
| Type 2 | 78 | 76 | |
| Type 3 | 41 | 59 | 88 |
| Type 4 | 42 | 74 | 100 |
| Type 5 | 4 | 100 | 100 |
| Total | 247 | 56 | 66 |
| Total without type 1 units | 165 | 72 | 85 |
CU, cardiology units.
Risk-Standardized Mortality in Type 3 and 4 Units Participating/Not Participating in the RECALCAR Survey in 2015 (Data for 2014)
| Participants RECALCAR | Nonparticipants RECALCAR | P | |
|---|---|---|---|
| CVD* | 6.4±1.2 | 6.8±1.6 | <.001 |
| HF | 9.7±2.3 | 10.2±3.6 | <.001 |
| AMI | 6.9±1.7 | 7.3±6.8 | <.001 |
AMI, acute myocardial infarction; CVD, cardiovascular disease; HF, heart failure.
Risk-adjusted standardized mortality ratio (for calculation method see Milakovich12), with indicators calculated using the Basic Minimum Data Set for 2014.
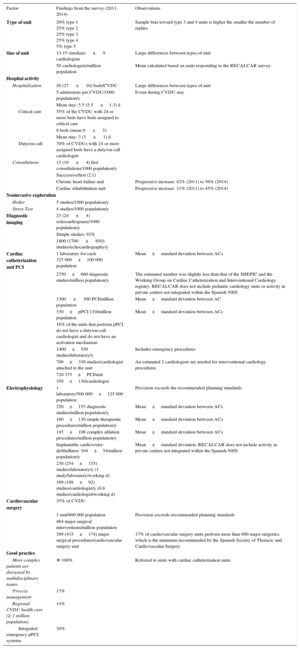
From 2011 to 2014, considerable stability was maintained in all the availability, utilization, and productivity indicators (Table 5). The median number of cardiologists per CU ranged from 13 to 15, with significant variations between CUs (standard deviation ± 9). There was a mean of 50 cardiologists/million population with significant variations between autonomous communities. The mean rate of CU discharges was 5/1000 population/y with a mean stay of 5.5 ± 1.1 days. No duty or on-call cardiologist was available in 30% of CUs with 24 or more beds; of these, no critical care beds were available in 45%. The mean rate of initial consultations was 16 ± 4/1000 population/y, with a ratio of 2:1 between successive and initial consultations. During the period analyzed, there was an increase in the number of heart failure (HF) units (42%-56%) and cardiac rehabilitation units (31%-45%). The mean rate of echocardiographic studies was 23 ± 4/1000 population/y, most of which were simple diagnostic imaging studies (92%). There was considerable variability in the productivity of echocardiography machines (1800 ± 650 studies/y), which in part may be due to variations in the amount of equipment (the survey asked respondents to only include equipment in the echocardiography laboratory, but some also included equipment in operating rooms, cardiac catheterization laboratories, etc.).
Summary of Data and Indicators (RECALCAR Survey)
| Factor | Findings from the survey (2011-2014) | Observations |
|---|---|---|
| Type of unit | 20% type 1 25% type 2 25% type 3 25% type 4 5% type 5 | Sample bias toward type 3 and 4 units is higher the smaller the number of replies |
| Size of unit | 13-15 (median) ± 9 cardiologists | Large differences between types of unit |
| 50 cardiologists/million population | Mean calculated based on units responding to the RECALCAR survey | |
| Hospital activity | ||
| Hospitalization | 26 (27 ± 16) beds/CVDU | Large differences between types of unit |
| 5 admissions per CVDU/1000 population/y | Event during CVDU stay | |
| Mean stay: 5.5 (5.5 ±1.3) d | ||
| Critical care | 55% of the CVDU with 24 or more beds have beds assigned to critical care | |
| 8 beds (mean 9 ± 5) | ||
| Mean stay: 3 (3 ± 1) d | ||
| Duty/on-call | 70% of CVDUs with 24 or more assigned beds have a duty/on-call cardiologist | |
| Consultations | 15 (16 ± 4) first consultations/1000 population/y | |
| Successive/first (2:1) | ||
| Chronic heart failure unit | Progressive increase: 42% (2011) to 56% (2014) | |
| Cardiac rehabilitation unit | Progressive increase: 31% (2011) to 45% (2014) | |
| Noninvasive exploration | ||
| Holter | 5 studies/1000 population/y | |
| Stress Test | 4 studies/1000 population/y | |
| Diagnostic imaging | 23 (24 ± 4) echocardiograms/1000 population/y | |
| Simple studies: 92% | ||
| 1800 (1700 ± 650) studies/echocardiography/y | ||
| Cardiac catheterization and PCI | 1 laboratory for each 325 000±100 000 population | Mean±standard deviation between ACs |
| 2750±660 diagnostic studies/million population/y | The estimated number was slightly less than that of the SHEPIC and the Working Group on Cardiac Catheterization and Interventional Cardiology registry. RECALCAR does not include pediatric cardiology units or activity in private centers not integrated within the Spanish NHS | |
| 1300 ± 300 PCI/million population | Mean±standard deviation between AC | |
| 330±pPCI 110/million population | Mean±standard deviation between ACs | |
| 16% of the units that perform pPCI do not have a duty/on-call cardiologist and do not have an activation mechanism | ||
| 1400±550 studies/laboratory/y | Includes emergency procedures | |
| 700±330 studies/cardiologist attached to the unit | An estimated 2 cardiologists are needed for interventional cardiology procedures | |
| 720 375±PCI/unit | ||
| 350±130/cardiologist | ||
| Electrophysiology | 1 laboratory/500 000±125 000 population | Provision exceeds the recommended planning standards |
| 250±155 diagnostic studies/million population/y | Mean±standard deviation between ACs | |
| 160±130 simple therapeutic procedures/million population/y | Mean±standard deviation between ACs | |
| 145±108 complex ablation procedures/million population/y | Mean±standard deviation between ACs | |
| Implantable cardioverter-defibrillator: 104±54/million population/y | Mean±standard deviation. RECALCAR does not include activity in private centers not integrated within the Spanish NHS | |
| 230 (254±155) studies/laboratory/y (1 study/laboratory/working d) | ||
| 169 (188±92) studies/cardiologist/y (0.8 studies/cardiologist/working d) | ||
| Cardiovascular surgery | 35% of CVDU | |
| 1 unit/900 000 population | Provision exceeds recommended planning standards | |
| 464 major surgical interventions/million population | ||
| 389 (433±174) major surgical procedures/cardiovascular surgery unit | 17% of cardiovascular surgery units perform more than 600 major surgeries, which is the minimum recommended by the Spanish Society of Thoracic and Cardiovascular Surgery | |
| Good practice | ||
| More complex patients are discussed by multidisciplinary teams | ≅ 100% | Referred to units with cardiac catheterization units |
| Process management | 17% | |
| Regional CVDU health care (≥ 1 million population) | 14% | |
| Integrated emergency pPCI systems | 38% | |
AC, autonomous community; CVDU, cardiovascular disease unit; PCI, percutaneous coronary intervention; pPCI, primary percutaneous coronary intervention; SHEPIC, Statistics on Health Establishments Providing Inpatient Care; NHS, National Health System; RECALCAR, Resources and Quality in Cardiology Units project.
Unless otherwise specified, data are expressed as mean ± standard deviation. Values have been rounded for purposes of readability.
The number of cardiac catheterization laboratories varied by autonomous community. Although sufficient, the number was less than that recommended in the standards document (400 000 population per laboratory).6 These data did not take into account the age of the laboratories. There was marked variability between autonomous communities in the rate of catheterization studies, particularly in diagnostic studies (2750 ± 660/million population/y). There was also marked variability between units in productivity indicators, such as the number of studies by laboratory and cardiologist (1400 ± 550 studies per laboratory per year and 700 ± 330 studies per cardiologist attached to the unit). These figures suggest that there is room for improvement in resource use. The mean rate of percutaneous coronary interventions (PCI) per unit and cardiologist was more than the minimum recommended by the SEC Working Group on Cardiac Catheterization and Interventional Cardiology.30
In general, there was a sufficient number of electrophysiology laboratories, although less than that recommended in the standards document (600 000 inhabitants per laboratory).6 There was an occasional lack of laboratories in some autonomous communities. There was marked variability between autonomous communities in the rate of electrophysiological studies, particularly in diagnostic studies (2750 ± 660/million population/y).
The RECALCAR registry sometimes included questions on cardiovascular surgery units. According to the data collected, only 17% of cardiovascular surgery units performed more than 600 major surgical interventions, which is the minimum number recommended by the Spanish Society of Thoracic and Cardiovascular Surgery.6
In relation to “good practice” recommended in the standards document, there was poor implementation of process management (only 14% of the units) and scarce development of CVD health care networks (17%).
The most relevant finding was the marked variability in structure, activity, and management indicators between CUs and between the autonomous community health services. In general, there was no shortage of equipment. However, there were organizational and administrative issues: no duty or on-call cardiologist was available in 28% of CUs with 24 or more beds; of these no critical care beds were available in 50%; there was poor implementation of process management; and scarce development of CVD health care networks.
Comparisons Between Types of UnitsThe results of comparisons between different types of units are shown in Table 6. More complex units had significantly more cardiologists, assigned beds, discharges, and external consultations. However, it is striking that no significant differences were found in relation to mean stay or the ratio of successive to first consultations.
Comparisons Between Types of Units (Survey)
| Types of units | P | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Units, No. | 15 | 25 | 35 | 43 | |
| Beds assigned (hospital) | 212.0±98 | 399.5±211 | 567.0±167 | 970.0±320 | <.001 |
| Total cardiologists | 4.83±4.19 | 7.31±3.52 | 15.12±3.96 | 24.33±5.98 | <.001 |
| Beds in CU, No. | 7.4±8.2 | 15.3±8.2 | 27.1±11.0 | 40.9±13.3 | <.001 |
| Discharges, No. (MBDS) | 774±424 | 659±316 | 1.187±345 | 1.767±387 | <.001 |
| Mean stay (MBDS) | 6.05±1.62 | 5.91±1.14 | 6.27±1.49 | 6.55±1.34 | .621 |
| First consultations | 2337±1878.00 | 2.703±1267.00 | 4774±2181.81 | 6927±2687.00 | <.001 |
| Successive/first | 1.88±0.69 | 2.15±0.83 | 2.34±0.98 | 2.38±1.25 | .445 |
| Echocardiograms, No. | 4138±2561 | 4524±2978 | 6727±2212 | 10 570±4160 | <.001 |
| Echocardiography/ultrasound | 1510±978 | 1525±596 | 2003±778 | 1976±710 | .162 |
| Catheterization laboratory | |||||
| Catchment population | 451 993±145 625 | 750 302±299 109 | <.001 | ||
| CC & PCI cardiologists | 3.24±1.11 | 4.87±1.15 | <.001 | ||
| Cardiac catheterization laboratories, No. | 1.09±0.47 | 2.25±0.62 | <.001 | ||
| Cardiac catheterization, No. | 1043±415 | 2092±826 | <.001 | ||
| PCI, No. | 540±244 | 976±335 | <.001 | ||
| PCI for AMI, No. | 167±83 | 304±127 | <.001 | ||
| pPCI for AMI, No. | 116±69 | 252±122 | <.001 | ||
| Studies/laboratory, No. | 1459±705 | 1432±487 | .703 | ||
| Studies/cardiologist, No. | 665±267 | 883±295 | .002 | ||
| Electrophysiology laboratory | |||||
| Catchment population | 234 897±123 688 | 436 566±139 838 | 727 851±276 007 | <.001 | |
| EE cardiologists | 1.33±0.58 | 2.69±0.75 | 3.31±0.88 | .180 | |
| EE laboratories, No. | 0.08±0.24 | 0.72±0.45 | 1.37±0.59 | <.001 | |
| Diagnostic procedures, No. | 50±14.1 | 99±66.1 | 202±162.6 | .127 | |
| Therapeutic procedures, No. | 70.25±47.00 | 78.90±43.70 | 196.00±112.40 | <.001 | |
| Ablation procedures, No. | 18.0±0.0 | 33.9±26.2 | 87.1±74.7 | .088 | |
| Studies/laboratory, No. | 149.3±150.0 | 294.1±233.5 | 555.2±331.7 | .004 | |
| Studies/cardiologist, No. | 74.7±75.0 | 142.1±128.3 | 245.9±173.0 | .003 | |
| Is the unit accredited for MIR teaching in cardiology? | 0.0% | 0.0% | 78.3% | 96.9% | <.001 |
| Research projects (public and private calls) | 0.87±2.56 | 0.67±1.09 | 1.65±1.85 | 7.32±7.43 | <.001 |
| Clinical trials involving at least 1 member of the unit | 1.00±0.00 | 3.07±2.43 | 5.15±4.40 | 18.68±20.17 | <.001 |
| Publications (JCR) | 2.83±1.72 | 6.23±9.24 | 8.11±6.58 | 34.29±33.34 | <.001 |
| Process management | 26.67% | 22.73% | 5.00% | 25.93% | .011 |
| CVDU health care network (600 000 or more) | 6.67% | 14.29% | 14.29% | 18.52% | <.61 |
AMI, acute myocardial infarction; CU, cardiology units; CVDU, cardiovascular disease units; ES, electrophysiological studies; CC, cardiac catheterization; JCR, Journal Citation Reports; MBDS, Minimum Basic Data Set; PCI, percutaneous coronary intervention; pPCI, primary PCI.
In relation to cardiac catheterization activity, type 4 units had a significantly larger catchment population and more cardiologists attached to CUs, laboratories, and activity than type 3 units, with a similar per-laboratory performance and higher productivity per cardiologist attached to the CU (665 ± 267 in type 3 units vs 883 ± 295 in type 4 units; P = .002).
Regarding electrophysiology laboratory activity, the more complex units tended to have a significantly larger catchment population and more cardiologists attached to CUs, laboratories, and activity than less complex units. Type 4 units had significantly higher performance per laboratory and productivity per cardiologist attached to the CU.
Most type 3 and 4 units (78% and 97%) were accredited to teach the MIR program (Spanish acronym for the intern and resident physician program). More complex units conducted significantly more research activity (research projects, clinical trials, publications).
Regarding the “best practice” recommended in the standards document,6 there was poor implementation of process management, especially in type 3 units, and scarce development of CVD health care networks.
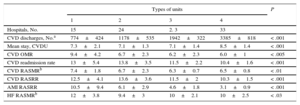
Associations Between Structure and Activity Data and Minimum Basic Data Set IndicatorsAssociations between structure and activity data for 2014 (obtained from the 2015 survey of CUs) and MBDS indicators for 2013 were analyzed. As expected (Table 7), hospitals with the most complex units had more discharges for CVD, with a longer mean stay in hospitals with type 4 units, which was probably due to the higher complexity of the disease processes treated. The more complex units had better mortality and readmission rates with type 4 units obtaining the best outcomes (Table 7).
Comparison of Types of Units. Basic Minimum Data Set. Results at Hospital Level
| Types of units | P | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | ||
| Hospitals, No. | 15 | 24 | 2. 3 | 33 | |
| CVD discharges, No.a | 774±424 | 1178±535 | 1942±322 | 3385±818 | < .001 |
| Mean stay, CVDU | 7.3±2.1 | 7.1±1.3 | 7.1±1.4 | 8.5±1.4 | < .001 |
| CVD OMR | 9.4±4.2 | 6.7±2.3 | 6.2±2.3 | 6.0±1 | < .005 |
| CVD readmission rate | 13±5.4 | 13.8±3.5 | 11.5±2.2 | 10.4±1.6 | < .001 |
| CVD RASMRb | 7.4±1.8 | 6.7±2.3 | 6.3±0.7 | 6.5±0.8 | < .01 |
| CVD RASRR | 12.5±4.1 | 13.6±3.6 | 11.5±2 | 10.3±1.5 | < .001 |
| AMI RASRR | 10.5±9.4 | 6.1±2.9 | 4.6±1.8 | 3.1±0.9 | < .001 |
| HF RASMRb | 12±3.8 | 9.4±3 | 10±2.1 | 10±2.5 | < .03 |
CVD, cardiovascular disease; CVDU, cardiovascular disease unit; HF, heart failure; RASMR, risk-adjusted standardized mortality ratio; RASRR, risk-adjusted standardized readmission ratio; OMR, overall mortality rate.
Hospitals with type 5 units were excluded from the comparisons due to their small numbers (2).
RECALCAR focused its first outcomes research on the 2 most prevalent disease processes in CU discharges: acute myocardial infarction (AMI) and HF. The first article published in this line showed that, within the Spanish NHS, the characteristics of the hospital, treatment in a CU, and PCI were associated with survival in patients hospitalized for myocardial infarction. The study recommended that the Spanish NHS establish health care networks that promote PCI and the participation of CUs in the care of patients with AMI.24 Based on RECALCAR data, Worner et al.31 found that in hospitals accredited to teach the MIR cardiology program with CUs that incorporated critical care and acute cardiovascular care units, risk-adjusted in-hospital mortality due to AMI was significantly lower than in those without these units. This finding supports the position statement of the SEC. Cequier et al.,32 found an association between the development of primary PCI health care networks, an increase in the PCI rate, and a regional decrease in the AMI mortality rate. Rodríguez-Padial et al.33 found similar AMI mortality rates, with lower readmission, mortality, and HF after AMI in patients with PCI treated in a CU and in hospitals with higher volume of activity.33 The 2 main recommendations of this study were the regionalization of units and the development of regional primary PCI networks (still incomplete in the Spanish NHS).
Similar preliminary results have been obtained in relation to HF (the second line of health outcomes research in RECALCAR).34–36
INFORMATION PROVIDED BY RECALCAR AND ITS LIMITATIONSRECALCAR has provided very important data on the structure, organization, functioning, and utilization of CUs and has greatly improved the information that became available in 2011 (the year of publication of the standards document).6 The stability of the data obtained between 2011 and 2014 made it possible to establish reliable planning and productivity criteria. The most striking finding was the significant variability in CU structure and process indicators. Given that this level of variability affected all aspects of CU activity, indicating marked differences in efficiency and productivity, there is much opportunity for improvement. These findings should act as a stimulus to the CUs that have not participated in the registry, because they will not only improve their outcomes but also improve the organizational and administrative aspects that significantly affect quality of care.10
There are marked gaps in quality, such as the poor implementation of process management and the scarce development of CU health care networks. Therefore, it is recommended that a duty or on-call cardiologist should be available in CUs with 24 or more beds, cardiologists should participate in the care of critical care patients,7,31 and the development of primary PCI regional networks should be completed.7,32,33
More complex units, particularly type 4 units (those with a cardiac catheterization laboratory and cardiovascular surgery unit) tended to obtain better outcomes in resource and personnel performance and in health outcomes. Studies derived from RECALCAR have reported an association between increased complexity and better outcomes, between hospital volume and mortality due to AMI and HF,33–35,37 and between hospital volume and readmissions after AMI, a trend that is contrary to that found in noncardiological processes (fewer readmissions with lower volume).38 These findings may to be related to improved critical care,31,39 the availability of cardiac catheterization laboratories,39 or treatment to discharge.39,40 As recommended in the standards document, it is important to confirm the need to regionalize cardiology units41 and to develop CVD health care networks that integrate different types of CU such that the patient can be provided with optimum treatment and efficient management at the most appropriate time and place.42
LimitationsThe main limitation of the data obtained is that their provision was voluntary and therefore cannot be extrapolated to all CUs. However, the participation rate was 72%, which is high for surveys of this kind. Despite this rate, the information may have been biased in favor of the participating CUs to the extent that these CUs showed better performance indicators than nonparticipating CUs. The reliability of the data collected in the survey has been verified by audits and compared with those obtained from other sources, such as the MBDS or the registries of the scientific working groups. There was a high level of agreement between the different sources.
Some of the limitations of the MBDS_CAR have beenmentioned. The MHSSE does not provide the complete database (with all discharge figures), and secondary diagnoses (such as shock) at admission cannot be eliminated. The MHSSE does not provide the SEC with the identity of the hospital, which is therefore deduced by indirect methods. This approach may lead to errors when analyzing associations between structure and activity data obtained from the survey and outcome indicators calculated using the MBDS. Furthermore, the MBDS has its own limitations because it is an administrative database. However, the use of administrative records to assess health service outcomes has been validated by comparison with data from clinical registries.37,38 In addition, the Spanish NHS MBDS undergoes regular audits and is a reliable information source.24
CONCLUSIONSRECALCAR provides relevant information on the structure, organization, functioning, and utilization of CUs. The RECALCAR survey had a high level of participation (72% of CUs with a structured cardiology unit), particularly from type 2 and 4 units, which tended to have better indicators. The marked stability of the data over the period analyzed (2011-2014) made it possible to establish reliable planning and productivity criteria.
Given the marked variability of the CU structure and process indicators, indicating significant differences in efficiency and productivity, there is much room for improvement. Regarding quality standards, it is recommended that there should be a duty or on-call cardiologist available in CUs with 24 or more beds, cardiologists should participate in the care of critical care patients, and the development of primary PCI regional networks should be completed. The most notable gaps in good management practice are the poor implementation of process management and the scarce development of CVD health care networks.
The RECALCAR project also provides information relevant to decision-making in health policy by analyzing associations between structure and resources and health outcomes. The most relevant aspects of this line of work, as set out in the standards document, are the recommendations to regionalize cardiology units and to develop CVD health care networks in order to provide better health care and improve the efficiency of the available resources.
FUNDINGThe RECALCAR project receives unconditional funding from Laboratorios Menarini.
CONFLICTS OF INTERESTElola Consultores receives funding for the development and management of the RECALCAR project.