Keywords
INTRODUCTION
In recent years, the radial approach has become a valid alternative to the standard femoral approach (FA) for the performance of cardiac catheterization, to the extent that its use is becoming increasingly widespread in catheterization laboratories.1-3
The major advantage of transradial catheterization is that it considerably reduces the morbidity associated with the access site. It does not require bed rest following the study, which makes it easier on the patient since it allows his or her early ambulation.4 In addition to being a safe technique, it is characterized by its high efficacy, with success rates in selected populations of over 90%.5
Despite the reported advantages, in our patient population the FA continues to be the approach of choice in many centers, although the transradial approach is becoming more widely employed (41.4% of the diagnostic procedures).6 One of the major limitations to the generalized application of this approach is the additional technical difficulty for the interventionist as it involves a learning curve for the solution of specific problems.7-10
Most of the information concerning transradial catheterization deals with the right radial approach (RRA). The left radial approach (LRA) has been less extensively studied, and there is little information from randomized studies comparing its efficacy and safety with those of the FA and RRA. However, there are certain advantages from the point of view of the vascular anatomy that make LRA an interesting option.
Our objective was to compare, by means of a randomized study in a large unselected patient population, the LRA with the FA and the RRA. The primary objective was to compare the success rate in the assigned approach. The secondary objectives were to evaluate the differences in the success rates among those cases in which there was no contraindication for the assigned approach, the procedure times and the incidence of vascular complications.
METHODS
Study Population
This prospective, randomized study was carried out in a tertiary-care hospital. The study population included 1005 consecutive patients who underwent cardiac catheterization in our center between January and July 2007. No exclusion criteria were applied. All the procedures were performed by 3 expert interventional cardiologists.
The patients were randomized to undergo FA (n=335), RRA (n=335) or LRA (n=335) using a block design in order to ensure that the same number of patients would be assigned to each technique for arterial access. The randomization list was in the hands of the nursing staff, who informed the interventional cardiologist of the assigned approach prior to the procedure. The catheterizations were performed by 3 interventional cardiologists, with previous experience in transradial catheterization who, over the previous 2 years, had carried out over 1000 procedures via that approach, achieving a success rate of 90% (but with previous selection of the patients; thus, this approach was attempted in less than 70% of the cases).
The study was approved by the ethics committee of our hospital, the patients and their relatives were adequately informed and they were provided with an informed consent form prior to inclusion in the study.
The Allen test was performed in all the patients assigned to the radial approach; transradial catheterization was not attempted if the results of the Allen test were clearly abnormal (in which case, it was considered that the procedure could not be completed via said approach).
Cardiac Catheterization
With respect to the procedure, the Seldinger technique was employed for radial access, preceded by injection of a local anesthetic (2% mepivacaine, 90 to 120 seconds prior to puncture). The puncture of the radial artery was performed with a 20-gauge × 1.5-inch needle (0.9 × 38 mm; Terumo Europe, Leuven, Belgium). Following introduction of a 0.025-inch guide wire, introducers (Radiofocus Introducer II, Terumo, Leuven, Belgium) measuring 11 cm in length, of 4, 5, or 6 French, depending on the criteria of the operator, were inserted. Prior to or during the catheterization, the operator was free to choose another approach. We compiled the reasons why the interventional cardiologist changed the approach for vascular access (absence of canalization, problems arising because of the vascular anatomy, crossover to angioplasty, etc), including a decision made freely by the operator (not only due to personal preferences when faced with certain clinical contexts, but also to certain characteristics of the patient such as weak pulses). Following radial artery cannulation, a combination of 0.2 mg of nitroglycerin, 2 mg of verapamil, and 5000 IU of heparin diluted in 20 mL of physiological saline solution was administered to prevent arterial spasm.
Initially, the catheters to be employed were Judkins left 3.5 (Cordis Corp., Johnson & Johnson, Miami, Florida, United States) for access to left coronary artery via the RRA, Judkins left 4.0 (Cordis Corp., Johnson & Johnson) for access to left coronary artery via the LRA and Judkins right 4 (Cordis Corp.) for access to right coronary artery. However, the operator could choose to utilize other curved catheters, and pigtail catheters for ventriculography. Catheter exchange was carried out using a 0.035-inch guide wire. Revascularization was performed using the techniques suitable for each lesion. Heparin or bivalirudin was administered, depending on the decision of the operator, during coronary angioplasty, as were glycoprotein IIb/IIIa antagonists when required.
At the end of the procedure, once the introducer was withdrawn, in 60% of the cases of transradial catheterization, hemostasis was achieved by means of a radial band system (TR band, Terumo, Leuven, Belgium), which was progressively removed over the 6 hours following the procedure (this corresponds to the percentage of patients who remained in our center once the catheterization had been completed). In the patients transferred to other centers, manual compression and a pressure dressing were utilized. In those patients in whom the transradial approach had been employed, ambulation was permitted immediately after the procedure had been completed; the patients who had undergone diagnostic catheterization were discharged from the hospital on the same day as the procedure. With respect to the femoral introducer, it was removed according to the standard protocol followed in our center and manual compression was applied in every case until adequate hemostasis was achieved, and no closure devices were employed.
Variables Analyzed
Several clinical variables were recorded, as were different procedure times (Table 1). In agreement with previous reports,2 we differentiated between major vascular complications (retroperitoneal hematoma, a decrease in hemoglobin of 5 grams, the need for transfusion or for vascular surgery) and minor ones (pseudoaneurysm, hematoma >5 cm in diameter, and loss of the radial pulse).
Objectives
The primary endpoint was to analyze the percentage of procedures completed using the assigned approach, which was understood to mean that the catheterization could be performed from start to finish via the initially assigned approach, without applying exclusion criteria. In this way, we intended to obtain a real image of the percentage of patients whose catheterization can be completed using the LRA in daily practice, comparing it with the RRA and FA. The inability to finish the procedure via the assigned approach involves both failures in the vascular access and situations that make it impossible or difficult to attempt the assigned approach.
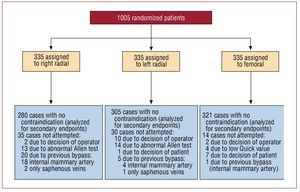
One of the secondary endpoints was to analyze the success rate in those cases in which there was no contraindication for any approach or crossover due to a decision made by the operator or by the patient (this analysis was carried out to obtain results that were not affected either by the patients in whom it was not possible to attempt the assigned approach due, for example, to abnormal Allen test results, or by the decision of the operator; contraindications taken into account were an abnormal Allen test for the transradial approach, previous bypass surgery for the RRA, a low value on Quick's test, mainly in the FA, and crossovers based on the decision of the operator or the patient) (Figure 1). The remaining secondary endpoints were the differences in procedure times (in the attempted cases) and the incidence of vascular complications.
Figure 1. Diagram of the distribution of the patients upon randomization and the number of cases excluded at each vascular access site for the secondary endpoint (cases in which there were no previous contraindications).
Statistical Analysis
The continuous variables are presented as the mean (standard deviation) and the categorical variables, as percentages. The differences among the clinical features of the patients were examined using analysis of variance for continuous variables and χ2 for categorical variables.For the differences between the LRA and RRA, and between the LRA and FA, Student t test was utilized for continuous variables and χ2 for categorical variables. The sample size was estimated on the basis of the primary endpoint, through our previous experience and the differences found in the literature (between the LRA and RRA)11; for a power of 90%, the number of patients required to detect a difference of 5% between groups was calculated to be at least 1002 in all. The SPSS 13.0 software package (SPSS Inc., Chicago, Illinois, United States) was utilized. A P value less than .05 was considered to indicate statistical significance.
RESULTS
The baseline characteristics of the study population and their distribution into the 3 groups are shown in Table 2. There were no significant differences among the 3 groups with respect to their baseline characteristics.
Successful Completion of Access
Among the 1005 patients included, the percentage of cases completed using the LRA was comparable to that of RRA (LRA, 71%; RRA, 68%; P=.67) and, in both cases, were significantly lower than those recorded for the FA (FA, 92%; P<.0001).
The transradial approach was attempted in the majority of the cases (86%) in which it was initially assigned. The interventional cardiologists attempted 90% of the procedures assigned to the LRA, 96% of those assigned to the FA and 83% of those assigned to the RRA (P<.0001).
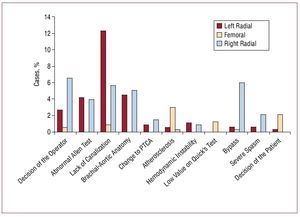
With regard to the reasons for failure to complete the procedure via the assigned approach (Figure 2), that most frequently reported for the LRA was lack of canalization of the artery (12.3%), followed by abnormal Allen test results (4.2%). Atherosclerosis of the iliofemoral vascular territory was the most common cause in the FA. For the RRA, the most common reasons for changing the access were previous bypass surgery in the patient and the decision of the part of the operator (6% and 6.6%, respectively), followed by the lack of canalization of the artery (5.7%). Excluding the cases of abnormal Allen test results or of bypass in the RRA, there were no significant differences between the LRA and RRA in terms of the rate of attempts (RRA, 92%; LRA, 94%; P=.16).
Figure 2. Reasons for the need for crossover to another approach in the totality of the patients. PTCA indicates percutaneous transluminal coronary angioplasty.
Analysis of the Cases Without Previous Contraindication for a given Approach
For these subanalyses, we excluded all the cases with a previous contraindication for any of the approaches or in which the patient or operator decided to make a crossover (Figure 1) (n=907).
Successful access increased for the transradial approach, with no significant differences between the 2 options (LRA, 80%; RRA, 82%; P=.25), and again, the FA was the most successful technique (transradial, 81%; FA, 96%; P<.001).
The most common reason for crossover from the LRA to another approach continued to be the lack of canalization of the artery (13%); in the case of the FA, it was atherosclerosis of the iliofemoral vascular territory (3.1%) and in the RRA, the lack of canalization, followed by problems derived from the anatomy of the aorta (6.8% and 3.6%, respectively).
Thus, in comparing the 2 options for radial access, the rate of failure was higher in left radial cannulation (LRA, 13%; RRA, 6.8%; P=.005). In the RRA, there was a greater need for crossover due to difficulties related to the vascular anatomy of the aorta (mainly tortuosities in right brachiocephalic trunk) (RRA, 3.6%; LRA, 0.7%; P=.01) and a greater tendency for severe arterial spasms (RRA, 2.5%; LRA, 0.7%; P=.07).
Procedure Times
With respect to the procedure times in the patients in whom access was actually attempted (n=900) (Table 3), cannulation took more time in the LRA than in the RRA, and in both cases, took longer than in the FA. The time to diagnosis tended to be shorter with the LRA than with the RRA, but was even shorter with the FA than with the transradial approach. The fluoroscopy time in the exclusively diagnostic procedures (n=533) was shorter via the FA, and there were no differences between the LRA and RRA. There were no differences among the 3 approaches with respect to the amount of contrast medium administered in the diagnostic procedures. The compression time and the time to ambulation were shorter with the transradial approach than with the FA, with no differences between the 2 types of radial access. The 3 approaches were comparable in terms of the total duration of the diagnostic procedure.
Coronary interventional Procedures
Of the 900 patients in whom the assigned access was actually attempted, 367 underwent interventional procedures. The rate of interventional procedures was comparable between the LRA and RRA (LRA, 38%; RRA, 36%; P=.31), and was lower when compared with the FA (LRA, 38%; FA, 48%; P=.006). However, once coronary angioplasty was carried out, there were no differences among the three approaches in terms of the time required to perform it (Table 3).
Vascular Complications
The incidence of vascular complications was considerably reduced with the transradial approach as compared to the FA. There were only 4 major vascular complications, all of them in the femoral artery (LRA, 0; FA, 4; RRA, 0; P=.07). The reduction in the incidence of minor vascular complications did reach statistical significance (LRA, 0.8%; FA, 3.1%; RRA, 0.4%; P=.01).
Implications of Patient Selection
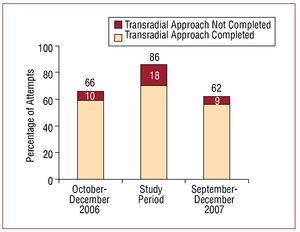
In order to analyze the influence of the percentage of attempts to achieve access on the results in terms of the completion rate, we recorded our experience immediately prior to and after the study. In our previous experience (the 3 preceding months; n=327), we performed a preselection of the patients who were to undergo transradial catheterization (66% of all the procedures), and achieved a success rate of 90%. After the completion of the present study (the following 3 months; n=318), again, with preselection of the ideal patient, the rate of attempts at radial access was 62%, with comparable success (91%) (Figure 3).
Figure 3. Percentage of attempted transradial approaches among all the patients subjected to cardiac catheterization and the success with this approach during the three months of previous experience (October to December 2006), the study period and the 3 subsequent months (September to December 2007).
DISCUSSION
The major finding of our study is that, in a large population of patients subjected to cardiac catheterization, the success rate with the LRA is similar to that obtained with the RRA, without prolonging the total procedure time, while offering the same advantages as the RRA (minimum vascular complications and early ambulation of the patient); thus, it is an alternative as valid as the RRA as compared to the FA. The rate of completion in both types of radial access was lower than that of the FA.
Left Transradial Approach and Femoral Approach
Of all the patients referred for catheterization, the percentage of patients in whom the procedure could be completed via the LRA was approximately 70%, and 81% in those cases in which there was no previous contraindication for any of the approaches. It is lower than with the FA and lower than that reported in other studies published to date. After a systematic review of 14 randomized studies comparing radial access and the FA published up to 2004, Agostini et al5 reported a rate of failure with the transradial approach of 7.2%,5 and they refer to the lack of an adequate previous learning curve as the major cause of the failure of the procedure. More recent studies even mention success rates comparable to those achieved with the FA, higher than 97%.9
However, the majority of the studies on transradial catheterization establish exclusion criteria that, on occasion, distance them from daily clinical practice. Failure of the transradial approach increases when we find ourselves in an unfavorable clinical context, as was recently seen in the FARMI study (primary or rescue angioplasty in patients with acute myocardial infarction in Killip class I), with a failure rate of 12% in the radial group.12
The previous experience of our center included more than 1000 transradial procedures, with a success rate of 90%, but with prior selection of the patients, a third of whom directly underwent the FA. Once we had completed the inclusion of patients for the present study, our success rates returned to nearly 90%, but again, the attempt rate was much lower than during the study (Figure 3). Throughout the study, the rate of attempted radial access was very high, excluding situations such as abnormal Allen test results or bypass in RRA (>90%). Therefore, it seems that previous patient selection is an important factor in the success of the transradial approach; the success diminishes when radial access is attempted in more unfavorable contexts. We consider that this fact supports the idea of performing proper patient selection for the radial approach. To interpret these results, it is important to remember that our study was based on a pragmatic design (with initial inclusion of all the patients), which attempts to reflect the reality of daily practice, distorted on occasion in some studies that start with a strict preselection of the patients.
Considering all the patients who underwent catheterization without exception, our percentage of completion using the assigned approach would approximate that of routine clinical reality. In this respect, it is not unusual that, out of every 10 patients who underwent the intervention, one had abnormal Allen test results, that in one there were problems with the cannulation of the artery due to a weak pulse or that in one, clinical or hemodynamic instability made rapid access necessary or the interventional cardiologist may have felt more comfortable with the FA.
With the LRA, the time required for cannulation of the artery is prolonged since the compression time is drastically reduced with respect to the FA. With regard to the differences in procedure times, those reported in previous studies are quite variable.5 In our series, the FA slightly reduced the diagnostic time, although this did not influence the total duration of the time on the catheterization table since it required more prolonged compression.
In agreement with other reports,13,14 in our series, radial access was also associated with a longer fluoroscopy time than the FA in diagnostic procedures, regardless of the use of the LRA or RRA. This is an interesting fact that supports the growing opinion concerning the possible need for increased radiological protection in transradial catheterization.
Left Radial and Right Radial Approaches
Considering all the patients who undergo cardiac catheterization without exception, the LRA is as valid an alternative to the FA as the RRA. In the majority of centers, the RRA is more frequently used for radial access, probably for the sake of convenience and familiarity with performing the study while positioned to the right of the patient, as in the FA. However, there are certain anatomical differences between the two routes of access, such as the presence of the right common brachiocephalic trunk, mainly of the innominate artery. Wu et al15 pointed out that passage through the latter, primarily in elderly patients, could generate difficulties for right transradial catheterization. The LRA offers the theoretical advantage of avoiding this passage and permitting a more direct access to ascending aorta. The possibility of achieving adequate catheterization of left internal mammary artery is another advantage of the LRA.
These differences have been reflected in clinical terms in certain studies such as those of Kawashima et al,16 in which the LRA shortened the procedure and the examination time, and of Fernández-Portales et al11 in which the RRA was associated with a higher failure rate due to problems with the tortuosity and atherosclerosis of the right common brachiocephalic trunk.
In our series, the success rates with the right and left approaches are comparable; however, once the patients were assigned to the LRA or RRA, the LRA was attempted more often, mainly because of the patients with left internal mammary artery who had undergone previous bypass surgery and were assigned to RRA, in whom it was systematically necessary to change the approach. There were no differences in the attempt rates, with the exclusion of the cases of abnormal Allen test results and bypass.
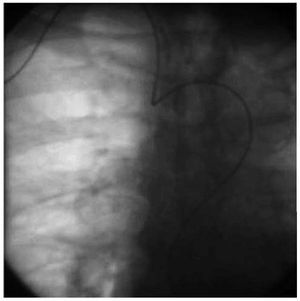
The cannulation of the artery using the LRA took longer than via the RRA, a fact that probably indicates the greater inconvenience for the interventional cardiologist when performing the puncture. Thus, the inability to cannulate the artery was the most common cause of failure of the LRA. With respect to the time to diagnosis, the difficulties produced in the passage through the right brachiocephalic trunk (Figure 4) are reflected in a greater tendency for severe arterial spasm when the RRA is employed and that the time to diagnosis is longer with that approach. These differences may be even greater if we take into account the fact that the LRA has been used more often in studies performed in patients with previous bypass surgery (5.7% of all the procedures involving the LRA and 1.6% of the procedures with the RRA; P=.02), and the cannulation of the grafts, as we know, prolongs the procedure. With respect to the fluoroscopy time, we have observed no significant differences. Our study has the limitation that it employs the examination time as the only indirect parameter of the exposure to radiation, but it offers as advantages its simplicity and reproducibility. Thus, it is not possible to adequately assess, for example, the reduced protection provided by the protective shield in the LRA as compared to the RRA.
Figure 4. Image showing the loop formed in the diagnostic catheter due to marked vascular tortuosity in the right radial approach.
With operators of short stature and corpulent or obese patients, the LRA can prove to be complex; this did not occur in our group, but it can be important in certain cases.
Coronary interventional Procedures
In our study, the FA was associated with a higher rate of interventional procedures than the transradial approach. The attempt of the latter in unfavorable contexts and the inclusion of patients for treatment with primary or rescue angioplasty may have influenced these data, but they probably reflect the fact that our group (and almost certainly many other laboratories) is more at ease and feels safer with the FA, mainly when rapid reperfusion is required or in technically complex angioplasties.
Once coronary angioplasty was initiated, there were no differences among the 3 approaches in terms of the time employed in the interventional procedure. This circumstance would indicate that, once experience with this technique is acquired, the procedure via the LRA neither takes more time nor is more complex.
Vascular Complications
The incidence of vascular complications is significantly reduced with radial access, even in situations in which these complications are especially relevant, as in the context of acute myocardial infarction, with the use of glycoprotein IIb/IIIa or fibrinolytic agents in a high percentage of the cases,17 or in the octogenarian patient.18 In our series, in accordance with other studies, the transradial approach was associated with a significant reduction of the incidence and severity of vascular complications. The LRA is found to be as safe as the RRA. Using the transradial approach, there were only 3 minor vascular complications: 2 hematomas measuring over 5 cm, in the context of intense anticoagulant and antiplatelet therapy, and a single case of pulse loss, with no clinical translation.
Limitations
This study was carried out in a single center. Given our interest in presenting a view as close as possible to clinical practice, we employed a pragmatic approach, randomizing all the patients, without exception; thus, on the basis of the primary endpoint of the study, the inclusion of patients with abnormal Allen test results or previous bypass surgery in the right radial group, as well as the decision of the operator, may penalize the radial approach to a certain extent, and should be taken into account for the correct interpretation of the results. Our group already had extensive experience with the LRA, a circumstance that may explain the difference with respect to the RRA and LRA in crossovers based on a decision made freely by the operator.
CONCLUSIONS
Of all the patients referred for catheterization, the percentage of cases in which the LRA was successfully completed was the same as for the RRA, although lower than with the FA. It prolongs the cannulation time, but without lengthening the procedure or the interventional procedure. Like the RRA, it eliminates the risk of major vascular complications and enables early ambulation.
ABBREVIATIONS
FA: femoral approach
LRA: left radial approach
RRA: right radial approach
SEE ARTICLE ON PAGES471-3
Correspondence:
Dr. V. Bodí.
Servicio de Cardiología. Hospital Clínico y Universitario de Valencia. Avda. Blasco Ibáñez, 17. 46010 Valencia. España.
E-mail: vicentbodi@hotmail.com
Received April 24, 2008.
Accepted for publication December 16, 2008.