Keywords
INTRODUCTION
Patients with diabetes mellitus account for approximately one quarter of those who undergo percutaneous coronary revascularization procedures.1 They also have a worse post-intervention prognosis than patients without diabetes.2
It is still a matter of debate as to what is the best coronary revascularization strategy to use in diabetic patients with multivessel disease. In recent years, drug-eluting stents (DES) have proved superior to conventional stents in randomized studies in this population.3-6 However, evidence that this approach may provide an alternative to coronary artery bypass surgery (CABG) in multivessel diabetic patients is still scarce.7
Currently, bypass surgery is the recommended treatment for diabetic patients with multivessel coronary disease. American guidelines (AHA/ACC) include percutaneous coronary intervention as a Class IIB recommendation for diabetic patients with 2 or 3 vessel disease affecting the proximal anterior descending artery when either stable angina or acute coronary syndromes are present.8,9
Our objective was to compare the evolution over the medium term (2 years) of diabetic patients with a multivessel condition in which DES or surgery were used to revascularize the proximal anterior descending artery.
METHODS
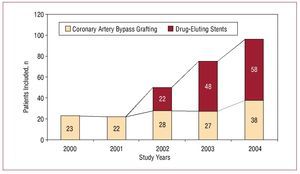
We performed a retrospective cohort study (2000-2004) in which we consecutively included diabetic patients with multivessel disease who underwent a first elective coronary revascularization with either DES (July 2002 to December 2004) or CABG (January 2000 to December 2004). Figure 1 shows the number of patients included for each year of the study.
Figure 1. Number of patients and study year.
Multivessel coronary disease was considered to be present when ≥70% stenosis was observed in 2 or 3 epicardial coronary arteries >2 mm. It was a requirement of the study that disease be present in the proximal anterior descending artery. We excluded patients who had undergone previous percutaneous or surgical revascularization (n=60), who required concomitant valve surgery (n=8), or who were without significant disease in the proximal anterior descending artery (n=90). We also excluded those receiving primary angioplasty for acute myocardial infarction (n=15) or who were treated concomitantly with conventional stents (n=30). Patients were considered diabetic if they had been previously diagnosed with the condition and were being treated with oral antidiabetics or insulin. Demographic, clinical, and angiographic data were recorded together with data on the type of intervention (percutaneous or surgical). Revascularization was defined as complete when the intervention was performed on all affected vessels. The study was approved by the hospital ethics committee and complied with the declaration of Helsinki. Informed consent was obtained from all patients.
During the study period, selection criteria for percutaneous or surgical revascularization were based on the coronary anatomy and individual risk profile, based on a joint decision between the interventional cardiologist, cardiac surgeon, and the cardiologist who had requested the coronary catheterization. Patient preferences were also taken into account. The surgical option was preferred in patients with left main stem disease, more complex coronary anatomy, and a lower preoperative risk of mortality.
The complexity of coronary artery disease was quantified using the SYNTAX score,10 while risk of mortality at 30 days after cardiac surgery was estimated using the EuroSCORE11 in both groups of patients.
Coronary revascularization Procedures
Coronary angioplasty and stent implantation (sirolimus-releasing—Cypher, Cordis, Johnson & Johnson—or paclitaxel—Taxus, Boston Scientific Corp.—) was performed according to the operator's criteria following the center's usual practice (visual estimation of the angiogram to a satisfactory outcome of residual stenosis <20% with TIMI III flow). Unfractionated heparin in bolus (100 U/ kg, or 70 U/kg in the case of concomitant use of abciximab, based on the operator's criteria) was administered before the percutaneous intervention. All patients received aspirin (100-300 mg) and clopidogrel 75 mg daily (300 mg loading dose in patients not previously taking the treatment) for 3 months after implantation of the sirolimus-releasing stent and for 6 months after receiving the paclitaxel stent.
The bypass procedure used was decided on by the cardiac surgeon and was performed without extracorporeal circulation (ECC) in most cases. All patients received at least one internal mammary artery.
Adverse Events and Follow-up
Patients were followed up in the cardiology clinic or by telephone. Coronary catheterization was carried out at the cardiologist's discretion when symptoms or signs of myocardial ischemia were present. The study endpoint was based on a combination of the following major adverse cardiac and cerebrovascular events (MACCE): death from any cause, non-fatal myocardial infarction, stroke, and coronary revascularization at 24 months. Patients were considered to have suffered a myocardial infarction if they met at least 2 of the following criteria: chest pain, development of Q waves in at least 2 contiguous leads of a surface electrocardiogram, and increased creatine to at least twice the normal laboratory range. Periprocedural infarction was deemed to have occurred when creatine values were elevated to twice the normal range after a percutaneous intervention or 5 times the normal range after surgery.
Secondary outcomes were overall survival and survival free of revascularization at 24 months. An analysis of cardiac mortality (sudden death, death due to myocardial infarction, or heart failure) was also performed.
Statistical Analysis
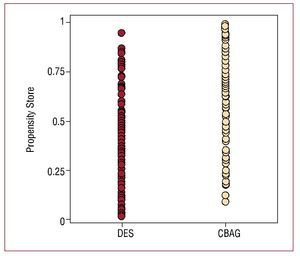
Given the non-randomized nature of the study and the multiple factors that could influence the choice of the type of treatment, the analysis was performed using a propensity score.12,13 This type of analysis takes into account the bias inherent in observational studies used to assess treatment effectiveness. The propensity score provides an estimate of the likelihood that any given individual will receive a treatment based on their baseline characteristics. We calculated the probability of being included in the surgical group of patients using a logistic regression model in which the dependent variable was CABG (DES=0, CABG=1). Baseline characteristics and pre-procedural angiographic variables as listed in Table 1 were included as predictor or independent variables. In the surgical group, the propensity score averaged 0.68 (0.22) compared to 0.35 (0.25) in the percutaneous group. The C statistic for the propensity score model was 0.83, indicating excellent differentiation between the 2 groups. The distribution of the propensity score is shown in Figure 2 for both groups.
Figure 2. Propensity score distribution in both groups. CABG group: median, 0.72; 25th percentile, 0.52; 75th percentile, 0.85. DES group: median, 0.28; 25th percentile, 0.13; 75th percentile, 0.54. CABG indicates coronary artery bypass grafting; DES, drug-eluting stent
We used a non-conditional logistic regression model to determine independent predictors of MACCE, death, and the need for revascularization during follow-up. Models were adjusted for the propensity score by introducing it as a covariate in each model.13 Event-free survival was analyzed using the Kaplan-Meier method and the log-rank test was used for between-groups comparisons. We used Fisher's exact test and a paired t test for comparisons between categorical and quantitative variables, respectively. Quantitative variables were expressed as mean (standard deviation) and categorical variables as percentages. Statistical analysis was performed using SPSS (Statistical Package for Social Sciences) version 14.0 for Windows. A P value less than .05 was considered statistically significant.
RESULTS
We analyzed 270 consecutive patients. Of these, 128 were treated percutaneously (DES) and 142 were treated surgically (CABG). Baseline clinical characteristics are shown in Table 1.
Patients in the DES group were older and more likely to have a previous history of stroke or high blood pressure. Of the DES patients, 35.2% had a EuroSCORE indicating high risk (≥6) compared to 30.3% of patients in the CABG group (difference not statistically significant). In addition, patients selected for surgery had more severe coronary artery disease (greater frequency of triple vessel and main stem disease) and a higher SYNTAX score. The majority of revascularization procedures (81.5%) were performed during elective admission for acute coronary syndrome. Angiographic characteristics and revascularization procedures are included in Table 2.
Paclitaxel- and rapamycin-eluting stents were used with similar frequency in the percutaneous group. A mean of 2.12 (1) stents was implanted per patient with a mean length of 25 (12) mm. Glycoprotein IIb/IIIa inhibitors were used in most cases. Using the ARC (Academic Research Consortium) classification,14 there were 2 definite cases of thrombosis (1 subacute and 1 late), 1 case of probable thrombosis, and 3 cases of possible thrombosis. Stent thrombosis occurred in 4.6% of patients in the percutaneous group.
All patients in the CABG group received at least 1 arterial conduit (left-internal mammary artery). A further 19% received an additional arterial conduit (radial artery or right internal mammary). Surgery was performed without ECC in 68.1% of cases. The mean number of conduits per patient was 2.5 (7). Two patients had mediastinitis. Anatomically complete revascularization was achieved more frequently in the surgical group.
The MACCE are shown in Table 3. Their distribution over the study period (during the first month, or otherwise) is shown in Table 4. Revascularization was not required during the first month in either group.
Follow-up to 24 months was completed in 97.4% of patients, and there were no differences between groups. Table 5 shows the adjusted odds ratio [aOR] for the different events studied. The percentages of MACCE observed were similar in the 2 groups (CABG, 18.7%; DES, 21.8%; adjusted OR =0.93,; 95% confidence interval [CI], 0.47-1.86; P=.85) as were those for the combined event of death, non-fatal myocardial infarction, and stroke (CABG, 15.8%; DES, 12.9%; adjusted OR =1.19; 95% CI, 0.72-1.88; P=.67). There were fewer revascularizations in the CABG group (CABG, 4.3%; DES, 12.1%; adjusted OR =0.42; 95% CI, 0.16-1.14; P=.09). This was partly due to a higher percentage of complete revascularization in the surgical group and to higher rates of revascularization of the treated lesion in the DES group.
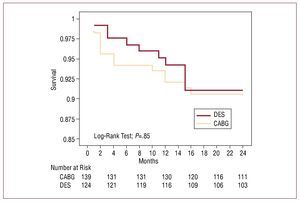
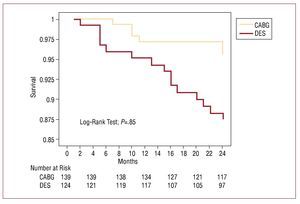
The Kaplan-Meier survival curves showed no difference between groups over the medium-term (CABG, 90.79%; DES, 91.31%; log-rank test, P=.85) (Figure 3). Moreover, the Kaplan-Meier curve charting survival free of subsequent revascularization showed the percentage free of revascularization at 24 months was higher in the surgical group (95.5% vs 88.46%; log-rank test, P=.03) (Figure 4).
Figure 3. Kaplan-Meier curve showing survival at 24 months. CABG: coronary artery bypass grafting; DES indicates drug-eluting stent.
Figure 4. Kaplan-Meier curve showing revascularization-free survival at 24 months. CABG indicates coronary artery bypass grafting; DES, drug-eluting stent.
We constructed 3 propensity score-adjusted Cox multivariable logistic regression models to identify factors predicting MACCE, death, and revascularization (Table 6). Kidney failure and prior stroke were independently associated with increased risk of MACCE. Age (per year increase), prior stroke, and left ventricular ejection fraction <45% were independent risk factors for death. Finally, CABG was identified as a protective factor against further revascularization procedures.
DISCUSSION
This paper summarizes the medium-term clinical results of 2 strategies for myocardial revascularization in a selected population of diabetic patients with multivessel disease. The approaches compared were surgery and percutaneous treatment using drug-eluting stents.
Due to the non-randomized nature of the study, multivariable logistic regression and a propensity score analysis were used to try to increase comparability between the 2 groups.12,13 Using this statistical method, it is possible to take into account the likelihood that a patient will be referred to one treatment group or the other based on their baseline characteristics. When combined with multivariable logistic regression analysis, the propensity score method ensures a greater degree of control over confounding factors. However, these factors may still be present if variables which were not taken into account when calculating the propensity score actually influenced the choice of treatment. Although the score was developed using a wide range of variables, it is not possible to control for all confounding factors and only random assignment can provide an unbiased estimate of treatment effect.
The adjusted analysis showed that, after 2 years of follow-up, there were no differences between the 2 approaches in terms of mortality, heart attack, or stroke. The main benefit of coronary artery bypass surgery was a reduction in the need for subsequent revascularization (OR =0.42; 95% CI, 0.16-1.14; P=.09). This benefit, although not comparable to a reduction in mortality or myocardial infarction, still has considerable clinical relevance because of its impact on quality of life (reduction in readmissions and in the morbidity associated with additional revascularization) and in economic terms (additional hospital stays, cost of further revascularization).
In the era of balloon angioplasty15,16 and conventional stents,17-19 most randomized trials which assessed revascularization strategies in multivessel coronary artery disease concluded that surgery was superior to percutaneous treatment both in terms of mortality and the need for further revascularization.
However, those studies drew conclusions on diabetic patients using subgroup analysis and they did not include systematic arterial revascularization in the surgical group. Nor did they include the use of glycoprotein IIb/IIIa inhibitors (a treatment which has shown a clear benefit in diabetic patients with acute coronary syndromes20) in the percutaneous intervention and of course they did not include the use of DES.21
Moreover, randomized studies of revascularization strategy in multi-vessel patients employed strict inclusion criteria, resulting in under-representation of a majority of patients seen in routine clinical practice. For example, only 36% of patients included in the European registry of coronary revascularization (EuroHeart Survey on Coronary Revascularization) were considered eligible to participate in a trial to compare percutaneous and surgical strategies.22
Outcomes in "real world" clinical registries, in which the best strategy is individualized, often differ from those observed in large randomized trials. A classic example is the BARI registry, in which no difference in survival was observed in diabetic patients in the percutaneous and surgical groups; in both cases, the survival rate was 74%.23 This finding was in direct contrast to that of the corresponding randomized trial.
The results of the present study are in line with those from previously published observational studies. The ARTS II registry7 showed that, in a subgroup of diabetic patients, 84.3% of those treated with a sirolimus-releasing stent were MACCE free after one year compared with 85.4% of those assigned to surgery in the ARTS I trial. Our results are similar, with no differences between groups after 2 years of follow-up.
After 1 year of follow-up, Brigouri et al24 found no significant differences in the target outcome of combined death, myocardial infarction, and stroke between DES patients and those undergoing CABG without ECC. They did, however, observe an increased need for revascularization in the DES group (19% vs 5%), a finding which they attributed to a higher rate of follow-up angiography in this group (53% vs 4.5%).
It is well known that, compared with nondiabetics, diabetic patients have higher morbidity and mortality after early and late CABG.25 In our series, 68.1% of patients underwent bypass surgery without ECC, though it is still unclear whether this technique is superior to surgery with ECC in terms of mortality or morbidity in diabetic patients.26,27 In our study, 13.6% of patients revascularized without ECC died or had a heart attack or stroke compared with 17% of patients in which ECC was used (no statistically significant differences). All patients received at least one arterial graft (internal mammary in all cases), which has been shown to reduce mortality in diabetic populations undergoing surgery.28
We applied a strict definition of complete revascularization,29 which did not take into account vessel caliber or myocardial viability. Our series therefore had lower rates of complete revascularization than those seen in other series. In line with other studies, the percentage of complete revascularization was lower in the DES group than in the surgical group. This aspect is of great importance in diabetic populations, in which the atherosclerotic process is accelerated and plaque instability is often present. Surgery protects a larger amount of myocardium and could prevent events caused by proximal lesions.
The incidence of stent thrombosis in our study (2.3% if definitive and probable cases are summed, and 4.6% if possible cases are also considered) was influenced by the use of the ARC classification criterion and was similar to that seen in other series which used the same classification.30
At present, the only comparative data available for DES and CABG was obtained in observational studies. Clinical trials currently underway, including SYNTAX,31 CARDIA,32 and FREEDOM33 will provide more evidence of the best revascularization strategy to use in multivessel diabetic populations.
Limitations
The main limitation of this study is that it was non-randomized, a fact which exposes it to the usual limitations associated with observational studies. Selection bias to one or another type of treatment may have been further magnified by the different inclusion periods for patients in the 2 cohorts. Despite the use of multivariable logistic regression analysis and a propensity score, confounding factors and differences between groups can persist. Data on the level of glycemic control was not available and could have affected the results.34 In terms of late loss, the effect of rapamycin and paclitaxel may not be comparable in diabetic patients, although there is no evidence that this translates into a clinical impact.35
CONCLUSIONS
In an unselected population of diabetic patients with multivessel coronary disease in which the proximal anterior descending coronary artery was affected, the principle advantage of CABG was the reduced need for revascularization. There was no difference in the rate of death, MI or stroke.
ABBREVIATIONS
CABG: coronary artery bypass grafting
DES: drug-eluting stents
ECC: extracorporeal circulation
OR: odds ratio
MACCE: major adverse cardiac and cerebrovascular events
Dr Domínguez Franco was awarded a contract by the Instituto de Salud Carlos III under the 2005 call to provide support in Specialized Postgraduate Health Care research.
Correspondence:
Dr. A.J. Domínguez Franco.
Campus de Teatinos, s/n. 29010 Málaga. España.
E-mail: antoniodominguez@secardiologia.es
Received June 27, 2008.
Accepted for publication February 10, 2009.