Towards the beginning of the last century, the main role of the cardiologist was in the art of diagnosis and treatment of valvular and congenital heart disease and heart failure. This was transformed around 50 years ago with the discovery of the potential benefits of closed cardiac massage and defibrillation in the management of acute myocardial infarction (MI). Indeed, the consequent development of the coronary care unit (CCU) to allow monitoring and rapid treatment of potentially lethal arrhythmias in acute MI is regarded by many as one of the greatest innovations in cardiology.1 Subsequently, exciting technological advancement in the invasive treatment of coronary artery disease has led to the focus of cardiologists being primarily on this field, and in particular revascularisation. Since its foundation, the demographics of patients admitted to the CCU have changed significantly, with a reduction in the incidence of ST elevation MI, an increased incidence of non-ST elevation MI, and larger numbers of patients presenting with haemodynamic instability related to other cardiovascular conditions. Further, the patient population is increasingly elderly and with greater comorbidities.2, 3 With these changes it is apparent that the roles of both the CCU and the cardiologist responsible for managing the acutely unwell cardiac patient also need to change.
The changing face of the coronary care unitThe history of the CCU had previously been described in four stages, primarily related to management of patients with coronary artery disease. Over recent years, admissions of highly complex patients with complicated MI, acute decompensated heart failure and cardiogenic shock, severe acute valvular disease, prolonged arrhythmias, iatrogenic complications of cardiovascular procedures, and adult congenital heart disease have increased. Further, prolonged life expectancy and increasing comorbidities have increased the challenges of managing this patient population.2 Thus, an additional phase in the CCU has been proposed—the critical care phase (Table 1) —and the CCU renamed the cardiac care unit.3, 4
Table 1. Stages in the History of the Coronary Care Unit.
| Years | Phase | Comments |
| 1912 | Clinical observation | Herrick's classic description of AMI published |
| Infarcted heart considered a wounded organ | ||
| Main treatment rest | ||
| In-hospital mortality 30% | ||
| 1961 | Coronary care unit | Julian's first description of the coronary care unit |
| Dedicated areas with continuous ECG monitoring, defibrillators and resuscitation-trained staff | ||
| Halved in-hospital mortality | ||
| 1970s-80s | Technology | Pulmonary artery catheterisation |
| Coronary angiography | ||
| Beta blockade | ||
| Thrombolysis | ||
| Primary PCI | ||
| 1980s-90s | Evidence-based | Randomised trials as basis for treatment |
| Guidelines from national/international societies | ||
| 2003- | Critical care | Formation of ESC WG ACC |
| Recognition of requirement for validated intensive care knowledge, skills and behaviours for cardiologists (CoBaTrICE) | ||
| Sub-specialisation in acute cardiac care |
AMI, acute myocardial infarction; CoBaTrICE, Competency Based Training programme for Training in Intensive Care Medicine for Europe and other world regions; ECG, electrocardiogram; ESC WG ACC, European Society of Cardiology Working Group on Acute Cardiac Care; PCI, percutaneous coronary intervention.
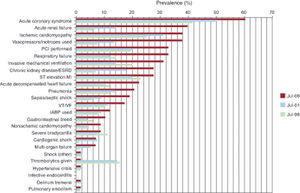
The diversity of healthcare structures, and differing nomenclature used throughout Europe can lead to confusion when defining/describing the CCU. This is further compounded by the increasingly overlapping knowledge base required by the cardiologist responsible for the CCU, and the intensivist responsible for the medical intensive care unit (Figure 1), together with the pathology seen on admission.2, 4, 5 Probably most useful is to put the patient at the centre of the definition, specifying the level and type of care/organ support required, rather than the type/name of unit.6 The main advantage over the more traditional geographical definitions (intensive care unit/cardiac care unit/high dependency unit/cardiac intensive care unit) is that the requirement for specialist care is highlighted.6 Of note, whilst the majority of intensive care units are led by clinicians trained in critical care medicine, and who are in a position therefore to deliver high-quality evidence-based critical care to their patients, in general this is not the case in the CCU.2 Here, many cardiologists erroneously believe that their general cardiology training addresses adequately the competencies required to manage critically ill cardiovascular patients.3, 7, 8
Figure 1. Snapshot of medical comorbidities and therapeutic trends (Duke University Hospital Coronary Care Unit July 1996, July 2001, and July 2006).ESRD, end-stage renal disease; IABP, intra-aortic balloon pump; MI, myocardial infarction; PCI, percutaneous coronary intervention; VF, ventricular fibrillation; VT, ventricular tachycardia. Reproduced from Katz et al., 2 with permission.
With increasing evidence that both intensive care unit and in-hospital mortality is reduced by clinicians specifically trained in intensive care,2, 9, 10, 11, 12 if cardiologists are to continue to optimally manage the CCU there is clearly a need for training in intensive care for these specialists. Further, demonstration that intensivists improve the utilisation of resources in the critical care setting has led to calls in some countries that all intensive care units should be managed exclusively by dedicated intensivists.2 With a high incidence of cardiovascular disease in the general intensive care setting ( > 11%-29%),5, 13 and the increasing range and number of immediately relevant investigations and interventions potentially undertaken by the cardiologist, the case for training cardiologists in intensive care medicine is increasingly compelling. There is, of course, a parallel requirement to ensure that intensivists are adequately trained in cardiology, in particular given the rapid recent advances in the treatment of heart failure, and percutaneous interventions.
The coronary care unit cardiologistThe extended skill set required to manage the modern CCU has led to the development of the subspecialty of acute cardiac care, together with a relevant syllabus and curriculum.8 This aims to define the knowledge, skills, and attributes required to manage the acutely unwell cardiac patient throughout the whole patient pathway, irrespective of the setting. In addition to obtaining the key cardiological skills, cardiologists are also required to develop the relevant competencies required for intensive care medicine as outlined by the European Society of Intensive Care Medicine collaboration, Competency Based Training programme for Intensive Care Medicine for Europe and other world regions (ESICM, CoBaTrICE).14 This acute cardiac care curriculum is therefore far beyond the scope of the core/general cardiology curriculum, recognising the developments in both intensive care medicine and acute cardiology that have occurred over recent years and the requirement for a multi-system approach to the critically ill patient. This clearly requires additional training within the general and cardiovascular intensive care unit setting, and mandates close collaboration between cardiologists and intensivists. Similarly, the American Board of Internal Medicine proposed requirements for Advanced Critical Care Certification for those with cardiology training in order to address this need.2, 15, 16
It is increasingly likely that some cardiologists may wish to train fully as intensivists as part of a complementary/dual training programme. Growing recognition by societies (both cardiological and intensive care) that cardiology is indeed an appropriate base specialty for intensive care training is to be welcomed.2, 15, 17 Although this will significantly increase the duration of training, the presence of such cardiologist-intensivists is likely to increase cross-specialty collaboration, benefitting a range of areas including training, education, direct patient care, and research into the pathophysiology and management of the critically ill cardiovascular patient. Availability of appropriately trained cardiologists in this field should lead to increased and improved dialogue between all the relevant specialties, extend the availability and visibility of the relevant skills of the cardiologist, and thus improve management of this critically ill patient population.
ConclusionsThe CCU has changed dramatically since its initial inception, and with it has changed the required skill set of the CCU cardiologist. It is no longer acceptable to assume that all cardiologists are trained in acute cardiac care and can manage the critically ill cardiac patient. Application of high quality, appropriate, evidence-based medicine to these complex, high-risk cardiac patients requires formal training in this field, and an ongoing collaboration between cardiology and intensive care medicine.
Conflicts of interestNone declared.
Corresponding author: Royal Brompton Hospital, Sydney St, London SW3 6NP, United Kingdom. S.Price@rbht.nhs.uk