Keywords
INTRODUCTION
Temporary transvenous endocardial pacing was first described by Furman and Robinson in 1958.1 Although there are several types of temporary cardiac pacing (transcutaneous, transesophageal), the most widely used is transvenous, i.e., peripheral venous puncture and placement of an electrode in the right chambers. This type of pacing has been employed since the 1960s, when it was first used in patients with permanent arrhythmias. Since that time, it has become common in the majority of hospitals, and the indications for its use are currently well established by the American College of Cardiology/American Heart Association (ACC/AHA).2
According to these published standards,2 temporary artificial pacing is indicated in various situations, particularly in patients with severe bradyarrhythmia (second- or third-degree atrioventricular block [AVB], or severe symptomatic bradycardia). It can also be used in overdrive atrial pacing to suppress tachyarrhythmias such as atrial flutter, or in overdrive ventricular pacing to treat recurrent ventricular tachycardia or to prevent severe ventricular arrhythmia secondary to prolonged QT interval. In addition, temporary pacing can be used as a bridge when replacing the generator in patients with a permanent pacemaker.
The use of temporary pacing in acute myocardial infarction (AMI) deserves special attention, since the risk-benefit ratio is not well defined in these cases. Although the presence of AVB is thought to imply greater mortality in these patients, death is usually related to the infarct size rather than the conduction disorder.3
Temporary pacing is used in situations of extreme emergency, and the devices are frequently implanted in older uncooperative patients. Implantation is typically accompanied by hemodynamic and/or electric instability that sometimes does not allow perfect placement, thus resulting in greater morbidity and mortality. Furthermore, implantation often must be done by medical residents during on-duty hours when supervision by the cardiology staff may be limited. Due to the progressive ageing of the population, the incidence of AVB is higher, and this fact may explain the higher number of permanent pacemakers and, by extension, temporary pacemakers, that are required.4
The recent literature contains no data on the incidence of complications in this procedure. Therefore, we felt it would be useful to analyze the outcome of temporary pacemaker placement and in-hospital follow-up of patients who need this device, and assess the complications potentially resulting from its use.
The study objectives were to determine the clinical characteristics of patients who required placement of a temporary pacemaker at our hospital, to assess the arrhythmia etiology and clinical follow-up of patients treated during hospitalization, and lastly to compile data on the related incidence and types of complications.
PATIENTS AND METHODS
Patients
A total of 568 patients received a temporary pacemaker over a 6-year period from 7 July 1997 to 31 May 2003; the medical histories for 530 (93%) of them were available for review. The remaining 38 patients correspond to cases transferred to another hospital after placement of the temporary pacemaker and for whom no follow-up was available. The most significant clinical variables (age, sex, concomitant diseases, and drug history) were analyzed, and the data for implantation of provisional pacemakers were also assessed, in particular, clinical symptoms and indication for implantation, route of access, thresholds, radioscopy time, etc. Data on patient progress during hospitalization were also analyzed, specifically, the treatment administered, need for a permanent pacemaker, clinical progress, complications, and in-hospital mortality.
Pacemaker Placement
All temporary pacemaker electrodes were implanted by the coronary care unit of our hospital in the examination room and with the help of a portable image intensifier. In all cases, a previously established protocol was used. The electrode catheters were placed by a cardiologist or by a cardiology resident under the supervision of a cardiologist. Bipolar electrode catheters (caliber, 6 Fr) were inserted in the femoral vein using the Seldinger technique and placed in the right ventricular apex under radioscopy; a pacing threshold of 0.5-0.7 V was considered adequate. Temporary pacing was initially set at voltage values twice the threshold level. In all cases, electrode positioning was confirmed by chest x-ray. The patient remained on bed rest under continuous electrocardiographic monitoring (telemetry) until the permanent pacemaker was implanted or the symptoms causing the indication for a temporary pacemaker had been resolved. All patients received therapeutic doses of anticoagulant therapy until the temporary pacemaker was removed. In most cases, anticoagulation was performed with subcutaneous low-molecular-weight heparin at anticoagulant doses (mg/kg weight/12 h). Intravenous heparin sodium was used in some cases (impaired kidney function, mechanical heart valves, postinfarction, etc), with activated partial thromboplastin time (APTT) monitoring and dose adjustments to maintain this value between 1.5 and 2.5.
Pacemaker malfunction was defined as failure of capture or sense, or both. Only complications directly attributed to the temporary pacemaker were reported. The specific mortality was determined for each cause.
In addition, the incidence of complications was analyzed according to whether the placement was done by a cardiologist or a cardiology resident.
Statistical Analysis
Results are expressed as mean ± standard deviation (SD) in the case of quantitative variables, and as percentages with 95% confidence interval (CI) using the exact binomial method in the case of qualitative variables. The statistical analysis used Student's t test for independent samples in the case of quantitative variables and the chi-square test for qualitative variables. In the between-group analysis of pacemaker malfunction and death, the statistically significant variables were introduced in multivariate analyses using forward stepwise logistic regression (0.5 for entry, 0.10 for removal) to assess the independence of variables. SPSS for Windows, version 11.0 (SPSS Inc. Chicago, United States) was used for the statistical analysis. Significance was set at a P-value <.05.
RESULTS
Mean age of the patients assessed (530) was 74.8±11 years (range, 15-98); 285 were men and 245, women. The clinical variables are listed in Table 1. A total of 67 patients (13%) presented AMI complicated by some advanced type of conduction disorder such as AVB, acute bifascicular block or asystole. This group presented special characteristics, with a lower age and different prevalence of risk factors than the group without AMI. Demographic and comorbidity data are shown in Table 2.
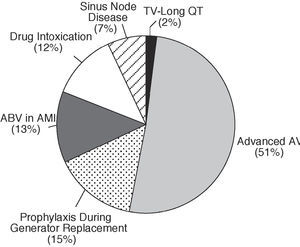
The indications for a temporary pacemaker included symptomatic advanced AVB in 270 cases (51%), prophylactic use due to generator replacement in 78 patients (14.7%) with a permanent pacemaker, bundle-branch block in the acute phase of AMI in 67 patients (13%), bradyarrhythmia due to drug intoxication in 65 patients (12.2%), symptomatic sinus node disease in 39 patients (7.4%), and long QT interval or ventricular tachycardia in 13 patients (2.5%) (Figure 1).
Fig. 1. Indications for placement of temporary pacemaker. AMI indicates acute myocardial infarction; AVB, atrioventricular block; VT, ventricular tachycardia.
The clinical manifestations leading to implantation were syncope in 214 patients (40.4%) and light-headedness in 112 (21.1%); 126 patients (23.8%) exhibited the clinical symptoms of left-sided heart failure, and 63 (11.9%), right-sided heart failure. In 15 patients (3%), the initial symptoms could not be determined from the clinical history. Cardiac arrest requiring cardiopulmonary resuscitation occurred in 42 patients (7.9%).
The mean ventricular rate at the time of pacemaker placement was 35±8 bpm.
Implantation was through the femoral vein in 99% of the cases, with the right femoral used most often (96%). The subclavian and jugular veins were used in two cases each.
Evolution
After placing the pacemaker, 97% of the patients were given low-molecular-weight heparin sodium at therapeutic doses. Anticoagulation was not used in 3%, mainly because of early implantation of a permanent pacemaker. The duration of temporary pacing was 4.2 days (range, 1-31). A total of 369 patients (69.6%) required a permanent pacemaker during hospitalization.
Complications
There were a total of 148 complications in 116 patients (22%) (Table 3).
Mortality
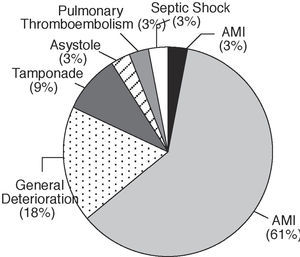
Thirty-four deaths (6%) occurred after implantation of a temporary pacemaker (Figure 2); 21 of these patients died of complications resulting from AMI. The group with AMI and a temporary pacemaker included 67 patients; thus, in-hospital mortality in this group was 31%.
Fig. 2. Causes of mortality (n=34). AMI indicates acute myocardial infarction.
Seven patients died of causes unrelated to cardiac disease: 6 from general deterioration and 1 from massive stroke.
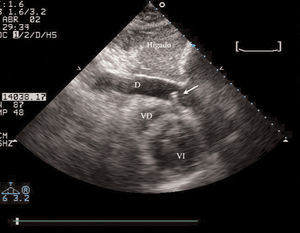
Another 6 patients (1%) died of complications attributable to the temporary pacemaker. Three deaths were due to tamponade caused by perforation of the right ventricle with the electrode catheter (Figure 3). In 1 case, death occurred due to asystole during insertion of the pacemaker. Another patient died from a massive pulmonary thromboembolism secondary to thrombosis of the femoral vein used for electrode placement. Finally, there was 1 death due to septic shock, also attributable to the pacemaker.
Fig. 3. Echocardiographic image from subcostal view. Severe pericardial effusion with image of the visible electrode tip in the pericardial cavity (arrow), after perforation of the right ventricle. PE indicates pericardial effusion; RV, right ventricle; LV, left ventricle.
The study population was divided into 2 groups according to mortality, and the most significant clinical variables were compared (Table 4). Acute myocardial infarction (AMI) or tamponade during evolution were statistically significant variables. In the logistic regression analysis, performed by introducing the most relevant clinical variables in the model, the independent predictors of mortality continued to be AMI (odds ratio [OR]=21.4; 95% CI, 9.3-48.9; P<.001) or cardiac tamponade during the course of the condition (OR=15.6; 95% CI, 3.1-78.4; P<.05).
Pacemaker Malfunction
In 48 patients (9%), pacemaker function was compromised due to migration of the electrode catheter, which required reimplantation. Between-group comparison showed a higher incidence of patient disorientation in the group with malfunction (19%) than in the group without malfunction (1.9%) (P<.001) Table 5). Logistic regression analysis of clinical variables potentially influencing the existence of malfunction showed that disorientation was the strongest independent predictive variable, with a 10.7-fold higher risk of malfunction (95% CI, 3.8-29.9; P<.001) in patients presenting with disorientation than those without. Tamponade was found to be more a consequence of the procedure than a predictive variable. Other variables likely to be predictive of malfunction, such as duration of pacing, threshold and radioscopy time were not statistically significant.
Other Complications
In 50 patients (9%), there were 57 severe complications: in 15 cases, the patient developed a considerable femoral hematoma (4 required transfusion) although anticoagulant overdose was not detected; 15 presented ventricular tachycardia or ventricular fibrillation during placement; 10 patients presented with fever >38ºC (3 had sepsis with positive blood culture), which the clinician attributed to the pacemaker; 9 experienced acute cardiac tamponade, with 6 of these undergoing urgent pericardiocentesis; in addition, there were 4 cases of deep venous thrombosis, 2 pericarditis with moderate effusion and 2 perforations of the femoral artery.
Comparison of Groups With and Without Acute Myocardial Infarction
The clinical variables for patients with and without AMI were compared (Table 2), as were patient evolution and complications (Table 6), showing differences in the duration of temporary pacing (6.1±5 vs 3.9±3 days; P<.01), need for a permanent pacemaker (9% vs 78%; P<.001), mortality (31% vs 2.8%, P<.001), and total number of complications (48% vs 18%; P<.05).
Comparison of Implantation by Cardiologists or Medical Residents
Of the 530 procedures, 98 were carried out exclusively by cardiologists. The remaining 432 were implanted by cardiology residents under the supervision of a cardiologist. The main demographic characteristics of the 2 groups are shown in Table 7. There were no differences in the overall percentage of complications between the 2 groups.
DISCUSSION
Types of Patients
The mean age of patients with temporary pacemakers was very high (35% were over 80 years old), and many had a number of important cardiovascular risk factors and concomitant diseases. Hence, the population has an inherently high risk of complications. A high percentage also presented severe symptoms and a low mean ventricular rate before pacemaker placement.
Indications
The indications in our series are very similar to those reported by other authors. Half the indications mentioned in the 1996 article by Murphy5 were due to complete AVB, and a lower percentage due to complications of AMI. In 1997 Ochoa et al6 found that the indications in more than half the population studied were AVB and sinus node disease, and rhythm disturbances secondary to AMI were the second most frequent cause. Conversely, older series, such as the one published by Jowet et al in 1989,7 report that up to 84% of patients requiring a temporary pacemaker presented AMI. This change in the proportion of indications is probably due to advances in the treatment of patients with AMI. The use of fibrinolytics and the rapid care given to these patients have led to spectacular improvements in the incidence of complications and survival.8
Implantation Data
The femoral approach, which allows rapid access and easy compression in case of bleeding, is preferred in our unit and was predominant in our series. The other approaches, used in very few cases, were alternative options when the femoral vein was not accessible. Other series5,9 present a greater predominance of the subclavian and jugular approaches, which were seldom used at our hospital.
The mean duration of temporary pacing was 4.2 days, a number justified by patients required prolonged pacing, for example, those presenting AMI or receiving treatment for bradyarrhythmia secondary to drug intoxication, who account for 25% of our series (Figure 1).
Complications
Temporary pacing has been associated with multiple complications since it was first used. However, there are considerable differences in the reported morbidity and mortality. A study conducted in 1983 by Hynes et al9 with 1022 patients, the largest series published to date, reported no deaths and only 13.7% with complications, of which pericardial rub was most frequent (5.3%).9 In contrast, in 1996 Murphy5 reported complications in 68 patients (35%) and death of 55 (28%) in a series of 194 patients. The author attributed this high percentage of complications to limited training of the young doctors and minimal supervision by more experienced physicians, as well as the use of central venous approaches that allow little compression. In 1999 Petch10 also cited physicians' limited experience as the reason for a high number of complications. In a series of 81 patients in Spain, Ochoa et al6 reported complications in less than 20% and no cases of perforation or death.
In our series, 22% of the patients presented complications of some kind. This high incidence of complications may be attributed to the fact that these pacemakers were inserted in emergency cases and in patients with AMI or poor clinical condition. Another possible explanation would be that a large number of pacemakers were implanted by medical residents under the supervision of more experienced cardiologists (82% of our population). The groups in whom implantation was done by cardiologists or residents (Table 7) were not randomly distributed. Therefore the patients' baseline severity and prognostic factors could be controlled, despite the inherent methodological problems, the analysis shows that in our setting and with our clinical protocol there were no differences in the complications observed between the groups. In contrast, there was a non significant tendency for patients in whom placement was done by experienced cardiologists to present more complications, possibly because these physicians take on the cases with a greater initial risk, e.g., patients with AMI (Table 7). Temporary pacemaker implantation by medical residents in our setting was not associated with a higher number of complications.
Mortality was 6% in our series, and was much higher in the group with AMI (30%) than the group without AMI (2.8%). The causes of mortality in the AMI patients were complications of the infarction in all cases. Only 6 patients died of causes possibly related to the procedure (3 tamponades due to right ventricle perforation, 1 asystole, 1 massive pulmonary thromboembolism, and 1 sepsis), accounting for 1% of all patients. Mortality in the AMI group appears to be lower than that reported in earlier series, which had levels of around 50%.3,7 This decrease in mortality is probably a partial reflection of the increased survival of patients with AMI in recent years.8
On logistic regression analysis, only the presence of AMI and cardiac tamponade were independent risk factors for mortality in our series.
Perforation
Perforation occurred at a level very similar to that reported in other articles, which have shown that perforation of the right ventricle can cause death; however, in many cases this is not dangerous and only causes failure to capture.11,12
Infection
The percentage of infection at the puncture site and sepsis was extremely low in our review. This may be because asepsis was maintained despite the urgency with which temporary pacemakers were implanted in our patients. In other series, the percentage of infection was very similar, being around 1%.5,13,14
Thromboembolism
In our series, clinically recognized pulmonary embolism occurred in only 1 patient, who died. Another 3 patients presented clinical symptoms of deep venous thrombosis. In previous series, the presence of deep venous thrombosis ranges between 25% and 39%.5,10,15 The low prevalence in our patients could be due to 2 factors: a) the use of therapeutic doses of heparin as part of the pacemaker implantation protocol, not routinely used in previous series, and b) diagnosis established by ultrasound techniques and phlebography in the series described, with most patients presenting no symptoms.
Malfunction
Malfunction due to electrode migration was 9% in our series, much lower than the reported levels of 18%-43% in previous series.5,6 This problem could be due to incorrect electrode positioning in the endocardium caused by the urgency of the procedure or by the duration of pacing. After logistic regression analysis, the only factor independently related to malfunction was patient disorientation, which indicated a 10.7-fold higher risk of this occurring. Disorientation, which is extremely common among older patients, would lead to mobilization of the limb and the electrode catheter, causing malfunction. In our series, however, the duration of pacing was not an independent variable for malfunction, probably because it was shorter than that of other series.5,7
Limitations of the Study
This retrospective, descriptive study has the limitations inherent to this type of design. Despite the high number of patients reviewed, the data obtained from this single hospital may not be applicable to all patients with temporary pacing. Nevertheless, the findings provide an accurate picture of actual clinical practice with this procedure in our setting. This previously unavailable information could serve as a basis for a prospective, multicenter registry of temporary pacemaker use.
Conclusions
Temporary pacemakers are necessary, as they decrease mortality in patients with severe bradyarrhythmia. Such devices are frequently used in elderly patients, many with multiple conditions, and occasionally with bradyarrhythmia secondary to acute myocardial infarction (13%). The most frequent arrhythmia is complete AVB. There are important clinical differences between patients who present complete AVB either spontaneously or drug-induced and those in whom it is secondary to AMI. In our population and at the short-term, most patients are treated by placement of a permanent pacemaker (69.6%). The incidence of complications affected 22% of our patients, although many were not serious. Less frequent, but serious complications, included cardiac tamponade (1.7%) and death (6%). The mortality was much higher among patients with AMI, up to 30%. Procedure-related mortality was 1%. In 9%, the electrode had to be reimplanted due to malfunction.
ACKNOWLEDGEMENTS
The authors would like to thank Conxa Julià, nursing supervisor, and all the nurses of the Coronary Unit of the Hospital Universitari Germans Trias i Pujol, as it would have been impossible to obtain this registry without their assistance.
Correspondence: Dr. J. López Ayerbe.
Servei de Cardiologia. Hospital Universitari Germans Trias i Pujol.
Ctra. de Canyet, s/n. 08916 Badalona. Barcelona. España.
E-mail: jlopezayerbe@hotmail.com