Keywords
INTRODUCTION
Since the demonstration of its advantages over medical treatment,1 surgical revascularization has been considered the treatment of choice for significant disease of the left main coronary artery (LMCA).2 Despite similar short-term results, the greater number of long-term events observed with percutaneous coronary intervention (PCI) in several clinical trials3 does not currently recommend this approach in patients with LMCA disease who are good candidates for revascularization surgery.4 PCI is considered the revascularization treatment of choice only when the LMCA is protected by a permeable graft.
The number of potential patients with significant LMCA disease who are poor candidates for surgical revascularization is unknown. The increase in the mean age of patients referred for coronary angiography, along with the more frequent use of PCI in acute myocardial infarction (AMI),5 favors an increase in the diagnosis of significant LMCA disease in patients who are poor candidates for surgery (either because of poor background characteristics or unstable hemodynamics). The advances made in PCI, especially the almost systematic use of coronary stents, have made this an alternative to medical treatment in patients with LMCA who should not undergo surgery.6,7 However, few data are available on the short and long-term outcomes of this technique.
The aims of the present study were: a) to present in-hospital and short and mid-term PCI results in patients with significant, unprotected LMCA who were poor candidates for revascularization surgery, and b) to determine the possible variables associated with different outcomes in these patients.
PATIENTS AND METHODS
Design
This was an observational, retrospective, single center study involving a historic cohort of patients.
Patient Selection
The study subjects were all those patients who, between April 1 1999, and December 31, 2003, were consecutively diagnosed with significant, unprotected LMCA disease and who were treated with PCI due to their status as poor candidates for revascularization surgery (PCI was defined as an attempt to pass an intracoronary catheter through the lesion, even if this could not be finally achieved). All patients underwent prior evaluation in the cardiovascular surgery department of our hospital, except when LMCA treatment was indicated in the background of an AMI (primary or rescue angioplasty) or cardiogenic shock. At our center there is consensus that urgent surgical revascularization is not indicated in such cases due to the risks associated with this treatment. Patients with LMCA who were good candidates for revascularization surgery but were electively treated with PCI (i.e., surgery was rejected by the patient or by the attending interventionist) were excluded.
Definitions
- Significant LMCA disease: ≥50% (by diameter) stenosis of the reference segment.
- Unprotected LMCA: absence of permeable anastomosed grafts involving the left coronary artery. All PCI procedures performed within 48 h of the onset of an AMI were considered to have been performed in an AMI background.
- Emergency: a procedure performed outside of normal scheduling that obliged the postponement of a programmed procedure, or which required the catheterization room to be opened outside of normal working hours.
The Parsonnet8 and Euroscore9 surgical risk indices were calculated according to their logistic regression models. The LCMA lesion was termed distal when its treatment required balloon inflation or stent implantation in the ostium of the circumflex or anterior descending artery, ostial when it was situated within 5 mm of the ostium of the left coronary artery, and medial when in all other locations.
- Left ventricular function: measured by echocardiography or ventriculography. The highest in-hospital value recorded was that considered in the multivariate models.
- Cardiogenic shock: invasive systolic blood pressure of <80 mm Hg (or <90 mm Hg with inotropic support) with signs of peripheral hypoperfusion.
- Angiographically successful PCI: procedure resulting in a residual stenosis of the LMCA lesion of <20% with a distal TIMI III (thrombolysis in myocardial infarction III) flow.
- Successful procedure: angiographically successful PCI with no worsening of the hemodynamic status nor any other major complications (death in the catheterization room, cerebrovascular accident, AMI in the 12 h following the procedure).
- AMI during follow-up: appearance of new Q waves in electrocardiograms (ECG) performed during follow-up, or an increase in creatine-kinase (CK) over twice our centers' reference value for our center plus significantly increased MB levels.
- Combined event: death, non-fatal AMI, or new revascularization of the LMCA during follow-up.
Procedure
Decisions on the interventionial techniques and devices used, and on whether to use glycoprotein IIb/IIIa receptor inhibitors and intra-aortic counterpulsation balloons, were made by the attending physician. The access route of choice was the femoral route. In all cases attempts were made to implant a stent.
Before the intervention, all patients received aspirin (200 mg/day orally or a single intravenous dose of 300 mg) and sodium heparin (10 000 U, except in patients receiving abciximab, in which case 3500-5000 U were administered according to the weight of the patient). As part of the habitual protocol of our catheterization room, all patients with AMI were treated using a 7 Fr catheter guidewire. All patients who were successfully implanted with a stent also received clopidogrel (loading dose of 300 mg plus 75 mg/day for 4 weeks after the procedure). The performance of an angiographic control was left to the criterion of the attending physician; the recommendation coming from the catheterization laboratory was that this should be performed at 4 and 7 to 8 months.
Follow-up
Creatine kinase and CK-MB levels were monitored and an ECG performed immediately after the procedure, and then again at 6, 12, and 18 h, and every 6 h after the onset of chest pain. The following events were registered during follow-up: readmission for any reason, readmission due to ischemic cardiomyopathy, death, non-fatal AMI, and non-scheduled revascularization (PCI or surgery) of the treated LMCA or of lesions in other vessels. Binary angiographic restenosis was deemed to have occurred during follow-up when quantitative analyses showed ≥50% stenosis.
Angiographic Measurements and Statistical Analysis
The pre-and post-intervention LMCA lesions were analyzed off-line by an experienced cardiac interventionist using an automatic edge detection system (CAAS II, version 4.1.1; Pie Medical Imaging Maastricht, The Netherlands). Continuous variables are shown as means±standard deviation (SD). The differences between groups were analyzed using the Student t test (for continuous variables) and the χ² test (for proportions). Using variables recorded in the literature as associated with a poorer in-hospital prognosis, a logistic regression model was constructed, from which those variables that did not affect the coefficients of others were removed. Similarly, 2 Cox regression models were used to determine the predictors of death and combined events during follow-up. Significance was set at P<.05. All calculations were made using SPSS software (version 11.0) for Windows.
RESULTS
Between April 1 1999 1 and 31 December 2003, 83 patients met the inclusion criteria and formed part of the study. During this time, 437 other patients were diagnosed with significant LMCA disease who were candidates for surgery. Five patients who were good candidates for revascularization surgery underwent angioplasty of the LMCA and were not included in the study (none of these showed complications during their time in the hospital). One of these patients (20%) died suddenly in the seventh month; the remainder survived until the end of follow-up (3 had not completed 6 months of follow-up when the experimental period ended).
Of the 83 patients included, 22 (27%) received percutaneous treatment for their LMCA disease in the context of an AMI (14 [64%] primary angioplasties and 8 [36%] rescue angioplasties). Nineteen of these 22 patients (86%) arrived at the catheterization room in cardiogenic shock. In 15 of the same 22 (68%), the LMCA lesion was considered to be the cause of the episode (in 4 patients [18%] the LMCA was occluded). In the remaining seven patients, the anterior descending artery (n=5) or the right coronary artery (n=2) was the causal vessel.
In 22 of the 83 patients (27%), surgery was contraindicated due to the poor state of the distal beds (n=16), comorbidity (n=3; malignant neoplasms under treatment), or a combination of the latter categories (n=3; poor distal bed status plus a malignant neoplasm [n=2] or poor distal bed status plus advanced liver disease [n=1]). In 39 patients (47%), surgical revascularization was contraindicated because of the risks associated with the procedure. Table 1 shows the baseline characteristics of the patients with and without AMI. All patients showed symptoms at rest during their initial hospital admission. Table 2 shows the general characteristics of the procedures and the baseline and post-intervention angiographic results. Brachial access was necessary in three patients since femoral access was impossible. In 31 of the 35 patients (89%) with a distal lesion, a simple implant technique was used to locate the stent in the main branch of the LMCA (the descending anterior artery in 24 patients [69%]), with later dilatation of the ostium of the secondary branch if it was compromised. In the remaining 4 patients, 2 trouser stents were implanted and the procedure completed with a kissing-balloon. Eleven of these same 35 patients (31%) with a distal lesion underwent rotational atherectomy, and 2 (6%) were treated with a cutting balloon due to the presence of severe calcification.
The procedure could not be considered successful in 7 patients: in 3 because no satisfactory angiographic result was achieved (1 patient died during the procedure), in 1 because the patients' Killip class worsened during the procedure (from 2 to 4), and in 3 because of death in the catheterization room despite a good angiographic result.
Few non-fatal events were recorded during hospitalization (Table 3). One patient required emergency percutaneous intervention because of the occlusion of the stent (implanted just 2 h before in a proximal anterior descending artery); the patient died of cardiogenic shock during the procedure. Overall in-hospital mortality was 28.9%. The causes of in-hospital death were acute refractory pulmonary edema in two patients and cardiogenic shock in the remaining 22.
Follow-up was possible for 82 (99%) patients in total (including 98% of the patients who survived the hospitalization stage). One patient was lost after 1 year of follow-up. Mean follow-up time was 17.0±9.9 months (median, 16.99 months; percentiles 25-75, 10.2-24.0 months). Mean survival was 19.7±2 months (95% CI, 15.7-23.8 months). Table 3 shows the events registered during and after the first year of follow-up. Overall mortality at the end of follow-up was 48% (59% of the patients who presented with AMI and 38% of the rest). In the first year of follow-up, 3 patients suffered sudden death, 1 died of congestive heart failure, 3 died during revascularization surgery for restenosis, and 1 due to an inferior AMI. Four patients died due to non-cardiac causes. In 1 patient the cause of death was unknown (although it was taken to be cardiac-associated). No cardiac deaths occurred after the first year of follow-up (2 patients died from malignant neoplasms).
Twenty eight of the 59 patients who survived the hospitalization stage underwent coronary angiography once more during the first year of follow-up. Nineteen (68%) of these procedures were performed as scheduled (without symptoms), and 9 because of the reappearance of symptoms. Seven patients presented with angiographic restenosis of the treated lesion and were treated again (Table 3). Four of these restenoses were detected during scheduled coronary angiography (21%) and 3 in patients who presented with symptoms (33%). Nine patients died before they received follow-up coronary angiography (2 because of cancer), 1 was lost to follow-up, and in the remaining 21 no coronary angiography was performed due to medical decision or patient unwillingness. No patient required a new revascularization after the first year of follow-up.
Logistic regression analysis (which included variables such as age, sex, presence of diabetes, emergency undertaking of the procedure, presence of hemodynamic shock, angiographic failure, and ventricular function <40%) showed that only the need to perform the procedure urgently was independently associated with greater in-hospital mortality (odds ratio [OR]=4.48; 95% CI, 1.14-19.36; P=.045). A tendency was seen towards greater mortality in patients with a left ventricular function <40% (OR=3.4; 95% CI, 0.89-13.32; P=.072). The model explained 84% of all deaths (95% CI, 74%-93%) according to the ROC curve. The inclusion of the Parsonnet and Euroscore indices did not improve the model's predictive power; they were therefore excluded.
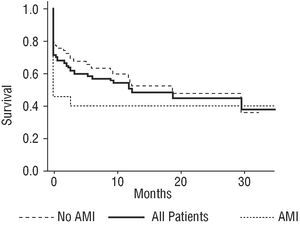
Figure 1 shows the survival curves for the clinical events studied when PCI was performed in patients presenting with and without AMI. Figure 2 shows the survival curves for combined events.
Fig. 1. Survival curves for readmission for: any cause, ischemic heart disease, revascularization of the LMCA, revascularization of another lesion, surgical revascularization and death (for patients with and without AMI), and for the entire patient population.
Fig. 2. Survival curves for combined events (death, non-fatal acute myocardial infarction, revascularization of the LMCA) (for patients with and without AMI and for the entire patient population).
In the Cox analysis (Table 4), no variable was independently associated with greater long-term mortality during follow-up. Only patients with diabetes, male, and with angiographic failure showed a certain tendency towards greater mortality (Table 4). No variable was found to be independently associated with any combined event during follow-up (Table 4).
DISCUSSION
The results show that PCI can be used to treat unprotected LMCA lesions in patients who are poor candidates for revascularizatio n surgery. However, despite a high proportion of angiographic success, the short- and long-term mortality remained high (in-hospital mortality 29%, 48% by the e nd of follow-up). The only factor that was independently associated with greater in-hospital mortality was the need for to perform the procedure urgently. During follow-up, none of the variables studied was independently associated with greater long-term mortality or incidence of combined events.
It is estimated that the mortality rate for medically treated LMCA disease of >50% is 21% per year and 50% at 3 years.10,11 Surgical revascularization improves survival12-15 compared to balloon angioplasty.16,17 The use of stents, along with other technical advances in PCI, has improved the results of treatment for unprotected LMCA.7,17-23 However, the occurrence of restenosis, sometimes manifested as sudden death,7,22,23 makes surgery the treatment of choice.
The extension of the use of diagnostic coronary angiography to older patients with poorer hemodynamic status means that more patients who are poor candidates for surgical revascularization are diagnosed with LMCA disease. The results that can be achieved with PCI, however, depend heavily on the condition of the patient.
In the present study, the large number of patients who presented with AMI might be the foremost factor conditioning in-hospital mortality compared to other studies.7,17-23 The present results show that 86% of the AMI patients presented in shock, and that 57.9% died in the hospital. Both the SHOCK24 study and later studies25 report a short-term mortality of >45% in patients who required early revascularization. Zeymer et al25 recently reported that the corrected mortality of patients in shock was 8 times greater when the culprit artery was the LMCA. The fact that primary angioplasty was undertaken with no AMI limitations in the present study (it was even performed in elderly patients in cardiogenic shock) may have led to the inclusion of patients with little chance of survival; this would explain the relatively poor results obtained. Even so, emergency percutaneous revascularization (ideally primary angioplasty) seems to be the most efficient treatment--if not the only treatment--that can be offered to patients who present with an AMI and who are poor candidates for surgical revascularization.
The only variable independently associated with greater in-hospital mortality was the need to perform PCI urgently. The sample size may have been the reason for this. However, other authors working with the same7,26 or slightly larger numbers22 of patients report other predictors of in-hospital mortality, i.e., variables not found to be predictors in the present study. The homogeneity of the present patients, all of whom were at increased risk, may explain why only those who were least stable or who were in the most critical condition showed greater mortality. There was a only a trend towards left ventricular dysfunction and greater in-hospital mortality. Its dependence on treatment and evolution time (with late improvements sometimes occurring even after hospital discharge) may have been a confounding factor. Unlike in earlier studies,27,28 no angiographic predictor of events in the short nor the long term was discovered. The clinical characteristics of more heterogeneous patients may have annulled the prognostic importance of lesion peculiarities. In the present study, LMCA disease was, on occasion, just another facet of terminal heart disease, the treatment of which was only palliative; while acute symptoms might have improved, the long-term prognosis could only remain the same. Some 35% of the re-admissions seen in the first year were not due to ischemic heart disease, and 28% were not due to cardiac causes at all; this shows the overall poor clinical status of the patients studied.
Counterpulsation balloons were used less often than expected, both in situations of shock and as a prophylactic measure. They were used systematically in patients in shock except when the immediacy of the resolution or the presence of peripheral vascular disease prevented their implantation. Their prophylactic use was mainly left to the criterion of the interventionist.
The need to repeat the revascularization of the LMCA in the first year was 9.6%. If the 3 patients who died suddenly during this same time period are added (probably because of restenosis of the LMCA), a figure for restenosis with clinical implications of 13% is obtained. Although studies with stents coated with anti-proliferative agents for LMCA disease are only in their early stages,29 and none are yet available with a diameter of >3.5 mm (often needed for the treatment of this problem),30 their use (which was infrequent among the present patients) might reduce the rate of restenosis and improve long-term prognosis.
LIMITATIONS
The study was performed only at one center and therefore these results should not be generalized. The decision not to perform revascularization surgery (except in patients with AMI) was reached by consensus between cardiologists and cardiovascular surgeons. Although based on internationally accepted objective criteria, the existence of a subjective component to these decisions cannot be ruled out. The influence of the center where the work was performed cannot be disregarded either: past experience and results may affect the decisions taken. Nonetheless, the size of the sample and the need for consensus almost certainly mean that the majority of the present patients would have been considered poor candidates for surgery at any center in Spain. The high risks calculated for surgery support the objectivity of the decisions made. The sample size may have been rather small for identifying independent predictors in multivariate analysis. Finally, it cannot be excluded that some of the trends seen may have become significant had the sample size been larger.
CONCLUSIONS
Percutaneous revascularization for LMCA disease in patients considered poor candidates for revascularization surgery is reliable and achieves a high level of angiographic success. Nevertheless, it is still associated with high in-hospital and long-term mortality. The need for emergency PCI identifies a subgroup of patients at greater risk of in-hospital death. The high mortality associated with PCI in patients with unprotected LMCA disease who are poor candidates for surgery warrant therapeutic alternative studies. Finally, physicians should be keenly aware of the different treatment options available to them.
See Editorial on Pages 1009-13
This work was partially presented as an oral communication at the XXXIX National Congress of the Sociedad Española de Cardiología, Seville, 2003.
Correspondence: Dr. R. López-Palop.
Ricardo Gil, 20, 3.° dcha. 30002. Murcia. España.
E-mail: mlopezs@meditex.es